Osteoarthritis of the hip joint is caused by a combination of intrinsic factors and extrinsic factors. Different surgical techniques are being performed to delay or halt osteoarthritis. Success of salvage procedures of the hip depends on the existing cartilage and joint damage before surgery; the likelihood of therapy failure rises with advanced osteoarthritis. For imaging of intra-articular hip pathology, MR imaging represents the best technique because of its ability to directly visualize cartilage, superior soft tissue contrast, and the prospect of multidimensional imaging. This article gives an overview on the standard MR imaging techniques used for diagnosis of hip osteoarthritis and their implications for surgery.
Osteoarthritis (OA) of the hip is caused by a combination of intrinsic factors, such as joint anatomy, and extrinsic factors, such as body weight, injuries, diseases, and load. Possible risk factors for OA are especially instability and impingement. Different surgical tequniques such as osteotomies of the pelvis and the femur, surgical dislocation, and hip arthroscopy are being performed to delay or halt OA. Success of salvage hip procedures depends on the existing cartilage and joint damage prior to surgery; the likelihood of therapy failure rises with cases of advanced OA.
For imaging of intra-articular pathology, MR imaging represents the best technique because of its ability to directly visualize cartilage, superior soft tissue contrast, and the prospect of multi-dimensional imaging. Opinions differ on the diagnostic efficacy of MR imaging and the question of which MR imaging technique is most appropriate. Many techniques showing similar promising data have been introduced for the knee. Conditions within the hip are different, and the relatively thin hip cartilage and the spherical-shaped joint pose difficulties in the diagnosis of cartilage and labral injury. High MR imaging resolution and contrast-to-noise ratio between bone, cartilage, synovium, and soft tissue such as labrum and capsule are required.
There is an ongoing investigation for the optimal MR imaging technique for imaging of the hip. Currently, MR arthrography using intra-articular contrast material has been established as the standard method for imaging of labral lesions; however, the diagnostic reliability of cartilage lesion remains moderate. The diagnostic reliability of acetabular cartilage delamination by MR imaging is still challenenging. The aim of this article is to discuss the current use of MR imaging in hip OA and its implications for surgery. As femoroacetabular impingement (FAI) becomes an increasingly important clinical diagnosis of the hip joint and is recognized as a precursor to the onset of hip OA, we will focus on this entity. Current standards, difficulties, and possible solutions using high-field MR imaging and future approaches are covered.
Femoroacetabular impingement
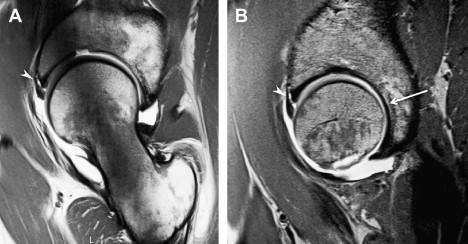
During the past decade, FAI has gained increasing attentiveness as a possible trigger of hip OA. The incongruency of the hip (eg, after Perthes disease) might be denominated as static form of impingement, whereas more subtle anatomic deformities, in which the incongruency of the hip joint exists only in certain positions during motion, are the dynamic form of impingement. Depending on the anatomic abnormality, there are two types of FAI: cam and pincer. In cam FAI, the cause of impact is a nonspherical shape of the femoral head coming along with insufficient femoral head-neck offset. In cam FAI, shear forces lead to acetabular cartilage damage ( Fig. 1 ), especially through forced flexion and internal rotation of the hip. In pincer FAI, the impact arises from acetabular overcoverage or other false configuration or shape of the acetabulum. The shape of the femoral head is spherical; however, the proximal femoral neck abuts frontally against the labrum and the acetabular rim. That way, the labrum is damaged primarily through recurrent trauma ( Fig. 2 ) before a cartilage damage occurs. Further causes for FAI are rotational anomalies with reduced femoral neck antetorsion and reduced acetabular version or an overcorrection after periacetabular osteotomy (PAO), also called “Bernese disease.”

Untreated FAI can lead to premature OA of the hip. To relieve symptoms such as limited range of motion and pain and further delay or halt the progression of OA, surgical treatment is necessary. Surgery includes reshaping of nonspherical femoral head in terms of cam, trimming the acetabular rim, or use of PAO in case of pincer FAI. The outcome of surgery depends on the quantity of pre-existing OA, with poor results occurring in patients with advanced degenerative changes. Follow-up examinations after open or arthroscopic FAI surgery showed favorable results, particularly in the subgroup of patients who did not have signs of advanced hip OA. In patients who have FAI, it is important to identify early stages of cartilage degeneration to identify patients who could profit from osteo- or chondroplastic types of surgery.
Diagnosis of Femoroacetabular Impingement
Diagnosis of FAI is based on clinical findings and radiographic analysis, including MR arthrography. Clinical symptoms of FAI include a slow onset of inguinal pain, which is usually pronounced with physical activities or prolonged sitting. During physical examination this can be reproduced by the “impingement test,” which examines hip pain produced by passive flexion, internal rotation, and adduction. A positive impingement test result can be correlated to acetabular labrum lesions. Radiographic assessment by means of standard anteroposterior and lateral views is used to asses late stages of hip OA and abnormal femoral head morphology, specifically the pistol grip deformity. Plain radiographic analysis is important in assessing acetabular version and coverage.
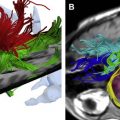
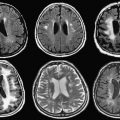
In cases of FAI, plain radiographs are often inadequate in terms of femoral head-neck junction morphology assessment and assessment of early-stage OA. Because of the importance of detecting these early hip joint lesions in FAI, MR imaging assessment is quickly becoming the standard tool for diagnostic assessment. It is becoming clear that standard coronal, axial, and sagittal MR imaging planes are less reliable than radially reconstructed planes perpendicular to the acetabular labrum in detecting early degenerative pathologies of the hip ( Fig. 3 ). For the assessment of the femoral head-neck morphology, radial reconstructions along the femoral neck axis improve the understanding of the FAI pathomechanism and correlate well with the prediction of FAI and intraoperative findings. This imaging technique is increasingly recognized as an important tool for morphologic assessment of FAI and an improved technique to detect early labral and chondral damage in the hip.

Measurements in Femoroacetabular Impingement
Different MR imaging parameters are defined for assessment of FAI, such as alpha angle, head-neck-offset, acetabular depth, and acetabular version. According to Pfirrmann and colleagues, the alpha angle can be measured between an axis parallel to the femoral neck passing through the narrowest portion of the femoral neck and an axis passing through the point at which the head contour passes into the metaphysis ( Fig. 4 ). An angle of 55° or more is considered increased and pathologic. An interval of 30° among the radial reformats should be used to assess alpha angle. The offset can be determined based on the method described by Ito and colleagues. It is the quotient of two lines defining the radius of the femoral head and the extension of the head-neck junction, which is defined by point at which the head contour passes into the metaphysis.

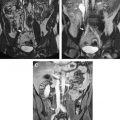
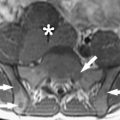
Offset is considered as reduced when it has a ratio of 1.2 or less. The acetabular coverage can be measured by assessing the acetabular depth within the axial reformat. The depth is expressed as distance between a line drawn among anterior and posterior acetabular horn and the center of the femoral head ( Fig. 5 ). The acetabular version can be measured using two- or three-dimensional axial T1-weighted MR imaging through the acetabular roof as the anterior and posterior rims become apparent. The acetabular version is measured between the distance of the acetabular and posterior rim to the anterior and posterior axis of the pelvis, as shown in Fig. 6 . Fig. 7 shows examples of different acetabular versions in patients with cam-type impingement (anteversion), mixed-type impingement (no version), and pincer-type impingement (retroversion).



Assessment of the acetabular labrum
For MR imaging assessment of the acetabular labrum, noncontrast techniques and arthrographic techniques are used. Based on comparison studies of different techniques in correlation to intraoperative findings, MR arthrography is more reliable in the diagnosis of acetabular labrum lesions. The contrast material, which is administered into the joint under fluoroscopic control, distends the capsule and allows better separation of the labrum and joint capsule. Labral tears may be better revealed through contrast filling into the clefts of the labrum. The diagnostic sensitivity of MR arthrography ranges from 90% to 71%; however, the interobserver reliability is only moderate.
It is not possible to assess the thickness and orientation of the acetabular lesion when a two-dimensional MR imaging technique is used. It is an invasive procedure that bears the risk of iatrogenic injury to adjacent neurovascular structures. Regarding staging and grading, most evaluation studies that have been described only determine location (anterosuperior, superolateral, and posterior) and whether a lesion is present. The added grading classification of grades 1 to 3 used by Czerny and colleagues depends on the degree of infiltration of the contrast agent into the acetabular labrum, a description of the tear, and changes of signal intensity, not yet correlated with structural changes of the acetabular labrum. In addition to staging there is still a lack of diagnosis for changes of the surface morphology, such as fibrillation, and changes on the junction between the acetabular cartilage and the acetabular labrum at 1.5 T.
Assessment of the acetabular labrum
For MR imaging assessment of the acetabular labrum, noncontrast techniques and arthrographic techniques are used. Based on comparison studies of different techniques in correlation to intraoperative findings, MR arthrography is more reliable in the diagnosis of acetabular labrum lesions. The contrast material, which is administered into the joint under fluoroscopic control, distends the capsule and allows better separation of the labrum and joint capsule. Labral tears may be better revealed through contrast filling into the clefts of the labrum. The diagnostic sensitivity of MR arthrography ranges from 90% to 71%; however, the interobserver reliability is only moderate.
It is not possible to assess the thickness and orientation of the acetabular lesion when a two-dimensional MR imaging technique is used. It is an invasive procedure that bears the risk of iatrogenic injury to adjacent neurovascular structures. Regarding staging and grading, most evaluation studies that have been described only determine location (anterosuperior, superolateral, and posterior) and whether a lesion is present. The added grading classification of grades 1 to 3 used by Czerny and colleagues depends on the degree of infiltration of the contrast agent into the acetabular labrum, a description of the tear, and changes of signal intensity, not yet correlated with structural changes of the acetabular labrum. In addition to staging there is still a lack of diagnosis for changes of the surface morphology, such as fibrillation, and changes on the junction between the acetabular cartilage and the acetabular labrum at 1.5 T.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree