Abstract
Multiple lucent lesions are most often the result of infectious diseases. Multiple cavities frequently complicate virulent bacterial, tuberculous, and parasitic or fungal infections. Septic emboli cause multiple cavities that are in the periphery of the lungs but may often resemble the appearance of necrotizing pneumonia. The distinction of septic emboli from necrotizing pneumonia is often based on patient history. A patient with a known malignant tumor may have multiple cavitary metastases that must be distinguished from cavitary opportunistic infections. Granulomatosis with polyangiitis is a chronic disease that causes ischemic necrosis with recurrent cavities. Chronic diseases that cause bronchiectasis, bullae, or multiple cysts are all possible causes of multiple lucent lesions that must be distinguished from cavities.
Keywords
amyloidosis, bullous emphysema, cavities, cystic bronchiectasis, cysts, diaphragmatic hernia, granulomatosis with polyangiitis, Langerhans cell histiocytosis, lymphangioleiomatosis, lymphocytic interstitial pneumonia, metastases, rheumatoid lung, septic emboli, vasculitis
Questions
- 1.
Refer to Fig. 24.1 . Which of the following is the best diagnosis?
- a.
Adult respiratory distress syndrome.
- b.
Pneumatoceles.
- c.
Multiple abscesses.
- d.
Bronchopleural fistula.
- e.
Necrotizing pneumonia, abscesses, and bronchopleural fistula.

Fig. 24.1
- a.
- 2.
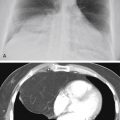
Which is the most likely diagnosis in the case illustrated in Fig. 24.2, A and B ?
- a.
Metastatic squamous cell carcinoma.
- b.
Histoplasmosis.
- c.
Tuberculosis.
- d.
Necrotizing pneumonia.
- e.
Mycoplasma pneumoniae.

Fig. 24.2
- a.
- 3.
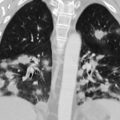
The multiple cavities with surrounding reticular opacities shown in Fig. 24.3 are consistent with which of the following diagnoses?
- a.
Klebsiella pneumoniae .
- b.
Metastases.
- c.
Coccidioidomycosis.
- d.
Mycoplasma pneumoniae .
- e.
Pseudomonas aeruginosa .

Fig. 24.3
- a.
Discussion
Many of the entities considered in Chapter 19 , Chapter 22 , Chapter 23 also result in multiple lucent lesions. In fact, some entities more typically produce multiple lesions. The latter include necrotizing pneumonias, septic emboli, cystic bronchiectasis, pneumatoceles, bullous emphysema, honeycomb lung, and metastatic tumor. Although the precise location of the solitary lucent defect is important, the distribution of multiple lucencies assumes an even greater importance in their radiologic analysis ( Chart 24.1 ).
- I.
Cavities
- A.
Infection
- 1.
Bacterial pneumonias 207 (Staphylococcus, Klebsiella, mixed gram-negative organisms, anaerobes, and Nocardia)
- 2.
Fungal infections
- a.
- b.
Blastomycosis 450
- c.
Coccidioidomycosis 373
- d.
Cryptococcosis 200 , 229 , 293
- e.
Mucormycosis 33
- f.
Sporotrichosis 89
- g.
Aspergillosis (invasive) 591
- a.
- 3.
- 4.
Parasites (echinococcal disease) 435
- 1.
- B.
Neoplasms
- 1.
Metastases 118
- 2.
Lymphoma (rare) 356
- 3.
Invasive mucinous adenocarcinoma (pseudocavities) 621 , 623
- 4.
Pulmonary papillomatosis 190
- 1.
- C.
Vascular
- A.
- II.
Cystic bronchiectasis (e.g., recurrent pneumonias, tuberculosis, cystic fibrosis, agammaglobulinemia, allergic aspergillosis)
- III.
Tracheobronchomegaly (Mounier-Kuhn syndrome) 381
- IV.
- V.
Bullous emphysema (see Chapter 22 )
- VI.
Honeycomb lung (see Chapter 19 )
- VII.
Cystic pulmonary airway malformation (CPAM) 357 , 626
- VIII.
Herniation of small bowel (congenital or traumatic)
- IX.
Idiopathic lung diseases with cysts
- 1.
Langerhans cell histiocytosis 20
- 2.
Lymphangioleiomyomatosis 424
- 3.
Lymphocytic interstitial pneumonia 398
- 4.
Amyloidosis 175
- 1.
Cavities
Infection
As in solitary cavities, infection is the most common cause of multiple pulmonary cavities (see Fig. 24.1 ). Acute pyogenic infections are radiologically characterized by areas of air space consolidation, a clinical course of elevated temperature, and often diagnostic laboratory findings, including elevation of the white blood cell (WBC) count with an associated shift to the left and positive sputum cultures. The development of multiple lucencies in the midst of an acute pneumonia (see Fig. 24.2, A and B ) is the expected appearance of necrotizing pneumonias. Peripheral cavities from necrotizing pneumonias and septic emboli are at high risk for rupture into the pleural space with bronchopleural fistulas causing pneumothorax. (Answer to question 1 is e .) Other causes of lucent spaces in the consolidations caused by pneumonia include the following: (1) resolution of the process with intervening normal lung; and (2) pneumatoceles. The pathogenesis of these processes was considered in Chapter 23 . Clinical correlation is extremely valuable in making this distinction. When the patient appears to be recovering from illness, the holes likely represent normal aerated lung or pneumatoceles. The radiologic observation of a round, sharply defined lucency with a discrete smooth wall suggests that the lucencies represent pneumatoceles. Ill-defined lucencies without a distinct margin are more typical of reaerated lung. The development of air-fluid levels in the midst of an area of consolidation indicates the development of spaces in the lung parenchyma that are most probably the result of tissue necrosis and abscess formation.
Air-fluid levels are not encountered in normally aerated lung or pneumatoceles; they are likely to appear when the patient is profoundly ill. In such cases, they are diagnostic of a virulent necrotizing pneumonia. The most common organisms to result in such a process include Staphylococcus, Klebsiella, Pseudomonas , anaerobes, and mixed gram-negative organisms ( Chart 24.2 ). (Answer to question 2 is d. ) As emphasized earlier, it is exceptional for pneumococcal pneumonia, Mycoplasma pneumonia, or viral pneumonias to cavitate, but cavitary Mycoplasma has been reported. 338 , 540
- I.
Infections
- A.
Necrotizing pneumonias 207
- 1.
Staphylococcus aureus
- 2.
Beta-hemolytic streptococci
- 3.
Klebsiella pneumoniae
- 4.
Escherichia coli
- 5.
Proteus, Aerobacter
- 6.
Pseudomonas
- 7.
Anaerobes
- 1.
- B.
Aspiration pneumonia (usually mixed gram-negative organisms)
- C.
Septic emboli 664
- D.
Fungus
- E.
Tuberculosis 641
- A.
- II.
Neoplasms
- III.
Vascular and collagen vascular diseases
- A.
Emboli with infarction
- B.
Granulomatosis with polyangiitis
- A.
- IV.
Trauma
- A.
Contusion with pneumatoceles 139
- A.
Septic emboli ( Fig. 24.4, A and B ) are another cause of necrotizing pulmonary infection that may result from infection with some of the same organisms that cause necrotizing pneumonia, especially staphylococcus and, more recently, methicillin-resistant Staphylococcus aureus (MRSA). 411 Septic emboli may result from any cause of systemic sepsis. Bacterial endocarditis of the right heart is a complication of intravenous (IV) drug abuse that places the patient at high risk for MRSA septic emboli. 312 Other sources of septic emboli include long-term indwelling vascular lines, pacemaker wires, septic thrombophlebitis, and organ transplants. 491


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree