Multiple Pregnancies in the First Trimester
INTRODUCTION
The widespread use of assisted reproductive technologies along with increasing maternal age has resulted in a steady rise in the frequency of multiple pregnancies over the past two decades.1 Pregnancies with twins and higher order multiples are at an increased risk for many maternal and fetal/child complications to include miscarriage, gestational diabetes, hypertensive disorders, preterm birth, fetal genetic and congenital malformation, fetal growth restriction, perinatal death, and cerebral palsy.2,3
Ultrasound is an integral part of the clinical care of multiple pregnancies, from the initial diagnosis to guiding the delivery of the neonates. In this chapter, we review the utility of ultrasound in the diagnosis and management of multiple pregnancies in the first trimester with a focus on twin pregnancies. Detailed evaluation of fetal congenital abnormalities is covered in subsequent chapters of this book. Table 7.1 lists the benefits of first trimester ultrasound in multiple pregnancies.
PREGNANCY DATING IN TWINS
There are no significant differences in the first trimester fetal biometric measurements between fetuses of multiple pregnancies and singleton fetuses and thus singleton-derived reference measurements of crown-rump length (CRL), biparietal diameter (BPD), head circumference (HC), abdominal circumference (AC), and femur length can be used in multiple pregnancies.4 Criteria for first trimester assignment of gestational age on ultrasound are also similar in twins and singletons and are discussed in detail in Chapter 4 of this book. Twin pregnancies are best dated when the CRL measurement is performed between 11+0 and 13+6 weeks of gestation.5 In twin pregnancies conceived by in vitro fertilization, the oocyte retrieval date or the embryonic age should date the pregnancy.5 In early gestation, the growth rate of twins is no different than that of singletons. On occasions, differential growth in twin fetuses can be detected by differences in biometric measurements such as CRL, BPD, and HC. When this situation is noted, it is recommended to date the twin pregnancy based on the biometric measurements (CRL) of the larger twin.5 For twin pregnancies presenting after 14 weeks of gestation, the larger HC should be used for pregnancy dating when biometric discrepancy is noted.6
Table 7.1 • Benefits of First Trimester Ultrasound in Multiple Pregnancies | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
ETIOLOGY AND PLACENTATION IN TWINS
Twin pregnancies are classified into two main categories—dizygotic and monozygotic—based upon the number of eggs fertilized at conception.
Dizygotic Twins
Dizygotic twins, also called fraternal, occur when two eggs are fertilized with two separate sperms resulting in two fetuses that are distinct genetically but share the same uterus. Dizygotic twins are always dichorionic/diamniotic, as each fetus has its own set of placenta and membranes. Several factors affect the rate of dizygotic twinning including maternal age, race, increasing parity, geographic area and presence of assisted reproduction.7 The rate of dizygotic twinning varies significantly around the world with high rates reported in
parts of Nigeria and low rates reported in Southeast Asia and Latin America.7,8
parts of Nigeria and low rates reported in Southeast Asia and Latin America.7,8
Monozygotic Twins
Monozygotic twins (also referred to as identical) occur when one egg is fertilized by one sperm followed by division of the embryo into two. These twins are therefore typically identical genetically. Unlike dizygotic twins, the rate of monozygotic twins is fairly constant throughout the world at 1/250 pregnancies9 excluding pregnancies of assisted reproduction. Monozygotic twins are associated with higher pregnancy complications and perinatal morbidity and mortality than dizygotic twins. Monozygotic twins can have various types of placentation based upon the timing of the division of the fertilized egg. Table 7.2 shows types of placentation in monozygotic twins in relation to the timing of embryo cleavage. Although conceptually monozygotic twins are identical, post-fertilization genetic events result in genetic heterogeneity between the twin pairs.10,11 Furthermore, discordance in fetal malformations, which poses significant challenges in clinical management, is not uncommon in monozygotic twins.
Zygosity and Chorionicity in Twins
Zygosity refers to whether the twins are genetically identical or not, whereas chorionicity refers to the type of placentation in twins. As shown in Table 7.2, monozygotic twins (identical) can have different types of placentation based upon the time of division of the fertilized egg, whereas dizygotic twins always have two separate placentas that on occasions can appear fused on ultrasound. Parents commonly ask at the time of the ultrasound examination whether their unborn twins are identical or not. It is important to note that the sonographic diagnosis of identical twins can only be made when the criteria for a monochorionic pregnancy (discussed later in this chapter) are met. When a dichorionic spontaneous twin pregnancy is diagnosed by ultrasound, the chance of identical twins in this setting is about 10%. From the point of view of pregnancy care chorionicity is therefore more important than zygosity.
Table 7.2 • Types of Placentation in Monozygotic Twins in Relation to Timing of Embryo Cleavage | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
DETERMINING CHORIONICITY/AMNIONICITY IN TWINS
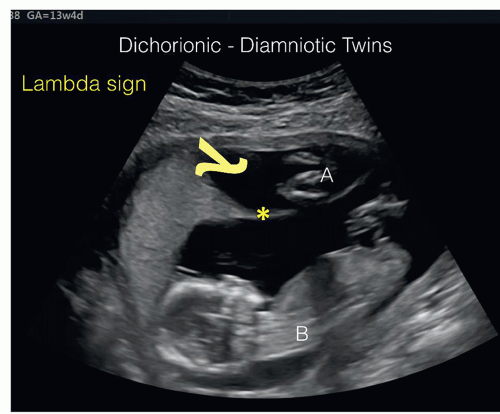
First trimester ultrasound can determine the type of placentation in twins with high accuracy. The diagnosis of dichorionic/diamniotic twin pregnancy can be made accurately when two separate and distinct chorionic sacs are seen in the endometrial cavity as early as the fifth week of gestation (Fig. 7.1). Indeed, until about 8 weeks of gestation, the presence of two distinct gestational sacs on ultrasound with embryos/cardiac activities confirms a dichorionic/diamniotic twin gestation (Fig. 7.2). Later on in early gestation, when two adjoining gestational sacs or fetuses are seen within the endometrial cavity, the characteristic of the dividing membrane(s), when present, is the most accurate way for determining chorionicity. Indeed, chorionicity should be ideally determined between 11+0 and 13+6 weeks of gestation if feasible.6 If the placenta
appears to fill the junction of the dividing membrane(s) at its insertion into the placenta, resulting in a thick wedge-shaped configuration (lambda or twin-peak sign), this is diagnostic of dichorionic/diamniotic placentation (Figs. 7.2, 7.3 and 7.4).
appears to fill the junction of the dividing membrane(s) at its insertion into the placenta, resulting in a thick wedge-shaped configuration (lambda or twin-peak sign), this is diagnostic of dichorionic/diamniotic placentation (Figs. 7.2, 7.3 and 7.4).
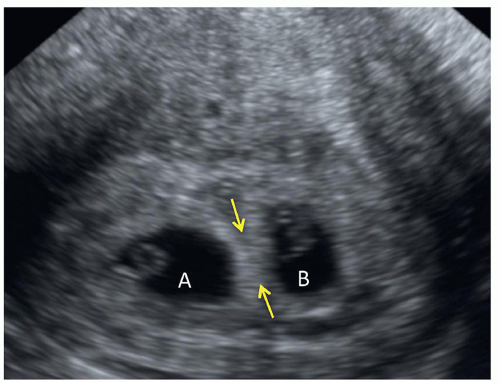 Figure 7.1: Sagittal plane of the uterus at 5 weeks of gestation with two distinct chorionic sacs A and B. The thick separation of the chorionic sacs (arrows) suggests a dichorionic twin gestation. |
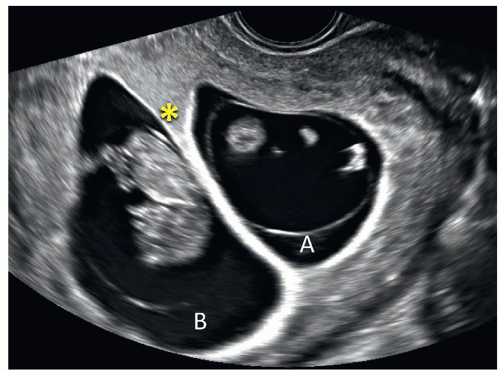 Figure 7.2: Dichorionic-diamniotic twins (A and B) at 9 week of gestation. Note the thick dividing membrane with a twin-peak sign (asterisk) at the placental insertion of the membranes. |
 Figure 7.3: Dichorionic-diamniotic twins (A and B) at 11 weeks of gestation. Note the thick dividing membrane with a twin-peak sign (asterisk) at the placental insertion of the membranes. |
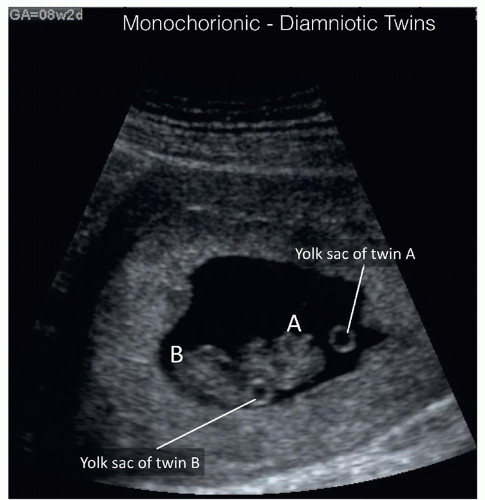
In monochorionic pregnancies, the dividing membrane attach to the uterine wall in a thin T-shaped configuration without any placental tissue at its insertion site (Figs. 7.5 and 7.6). The shape of the placental attachment of the dividing membranes (T-shaped) has a very high sensitivity and specificity for the diagnosis of monochorionicity between 11 and 14 weeks of gestation. Commonly, the presence of communicating fetal vessels on the surface of the twin placenta can be documented by ultrasound in color Doppler and this finding confirms the presence of monochorionic pregnancy (Fig. 7.6). The demonstration of such vessels however has no clinical relevance to twin pregnancy management. Although in general the number of yolk sacs correlates with the number of amnions (Fig. 7.7), this rule has many exceptions, as monoamniotic twins can be associated with a single yolk sac, a partially divided yolk sac, or two yolk sacs. For pregnancies beyond 8 weeks of gestation, the number of placental masses can be assessed as the presence of two distinct placental masses signifies a dichorionic gestation. The reliability of the number of placental masses is questionable, however, as in about 3% of monochorionic twin pregnancies two placental masses can be seen on ultrasound.12 The thickness of the twin separating membrane can also be used for determining chorionicity, and similar to findings
in the second trimester, this technique is not reliable to be solely used for chorionicity diagnosis. Occasionally the use of three-dimensional ultrasound can help in assessing membrane thickness in the first trimester of pregnancy (Fig. 7.8). Discordance in fetal gender at 13 weeks of gestation and beyond implies the presence of dichorionic gestation.
in the second trimester, this technique is not reliable to be solely used for chorionicity diagnosis. Occasionally the use of three-dimensional ultrasound can help in assessing membrane thickness in the first trimester of pregnancy (Fig. 7.8). Discordance in fetal gender at 13 weeks of gestation and beyond implies the presence of dichorionic gestation.
 Figure 7.5: Monochorionic-diamniotic twins (A and B) at 13 weeks of gestation. The dividing membrane (asterisk) is thin with a T-shape configuration at placental insertion (T). See Figure 7.6. |
 Figure 7.9: Monochorionic-monoamniotic twins (A and B) at 10 weeks of gestation. Note the presence of a single amniotic sac (labeled) with no dividing membrane. |
When no dividing membrane is noted on ultrasound, especially with high-frequency transvaginal or transabdominal transducer, the diagnosis of monoamniotic twins can be performed (Fig. 7.9). Color and pulsed Doppler confirms the diagnosis of monoamniotic twins by demonstrating the presence of cord entanglement (Fig. 7.10), which is almost universally seen in these pregnancies (discussed later in this chapter). Conjoined twins are diagnosed by ultrasound in the first trimester when shared tissue is noted between twins and
confirmed on color Doppler evaluation demonstrating shared vasculature (discussed later in this chapter).
confirmed on color Doppler evaluation demonstrating shared vasculature (discussed later in this chapter).
The first trimester ultrasound is thus very accurate in determining chorionicity in twin pregnancies with rates approaching 100% when correlated with delivery. Chorionicity should be determined before 14 weeks of gestation if feasible as the accuracy of ultrasound in determining chorionicity decreases with advancing gestation. It is therefore imperative that an early gestation ultrasound, preferably in the first trimester, be part of the management of twin gestation and that chorionicity is determined and reported at that time when feasible. As pregnancy advances, the accuracy of determining chorionicity and amnionicity decreases. The accuracy of determining chorionicity and amnionicity is estimated around 90% in the second and third trimester of pregnancy with the twin-peak or lambda sign being the most accurate and reliable method.13,14
ULTRASOUND LABELING OF TWIN FETUSES
Accurate labeling of twin pregnancy by ultrasound is important and should be clearly reflected in the report. Traditionally, twins have been labeled as twin A and twin B based upon fetal presentations in relationship to the cervix. This is confusing as fetal presentations may change during pregnancy and it is not uncommon for twin B to be born first at cesarean section, which presents confusion for parents. It is recommended to follow a descriptive process for twin labeling that takes into account the location of each gestational sac in relationship to maternal right or left side and the position of the sac in the uterus as upper or lower.5 For instance, twin A can be referred to as “on maternal left with posterior placenta and lower gestational sac.” This can be performed in the first trimester by the 13th week of gestation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree