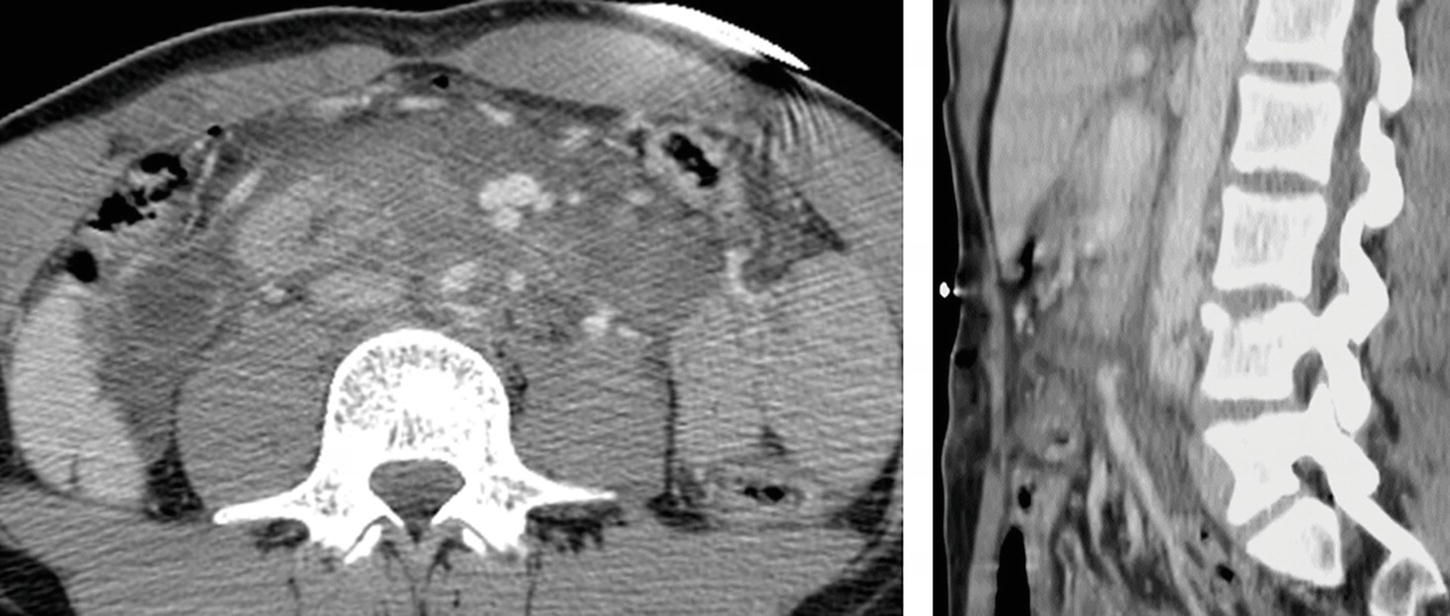
Patient 2: Axial, coronal, and sagittal contrast-enhanced CT images.
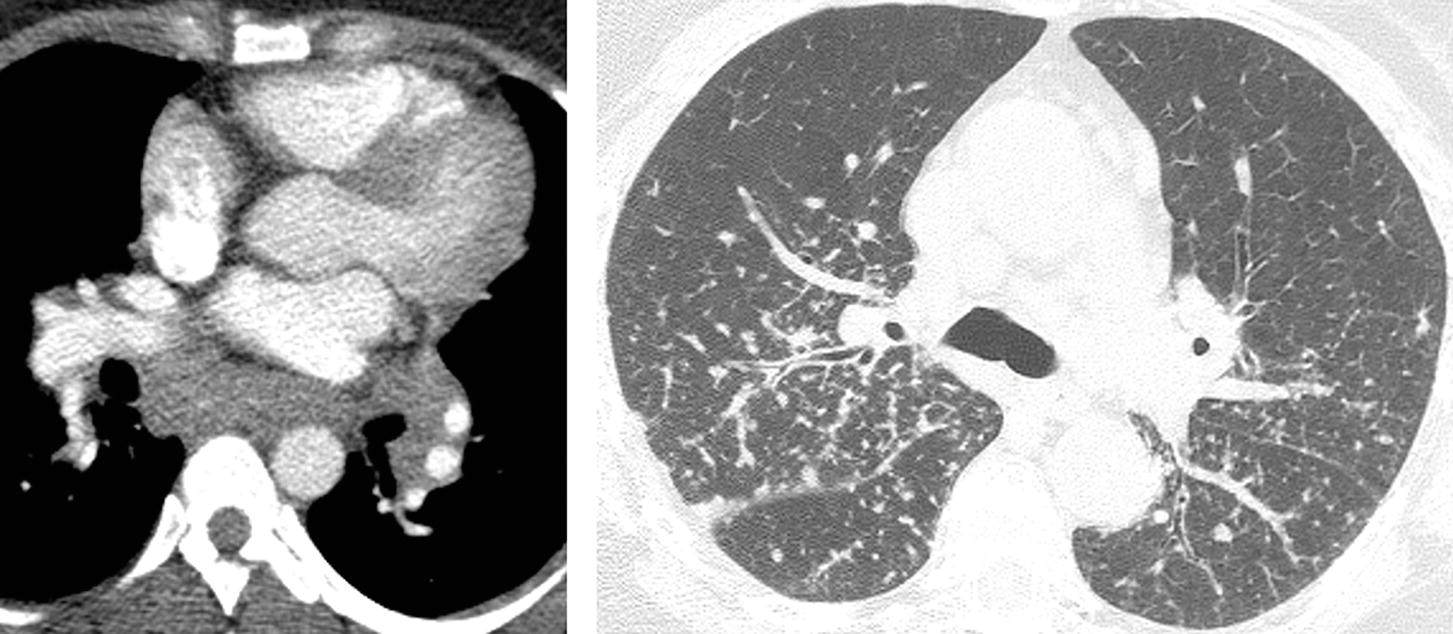
Patient 3:

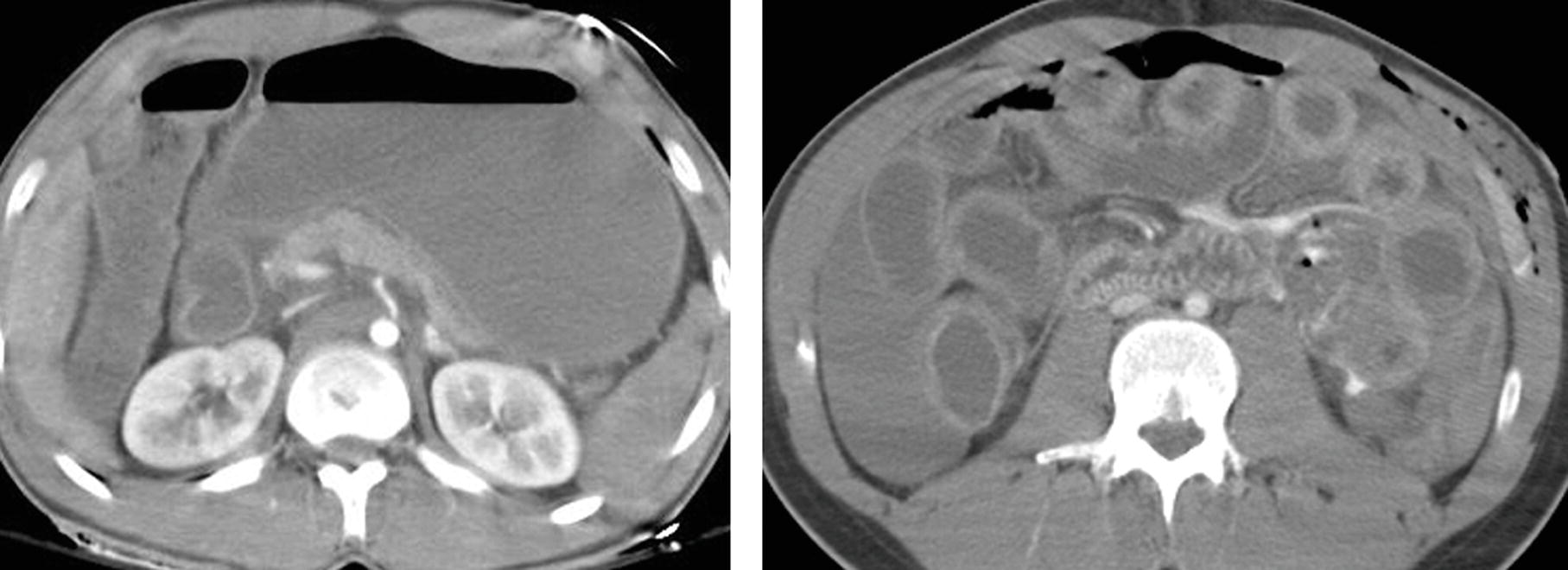
Patient 4:
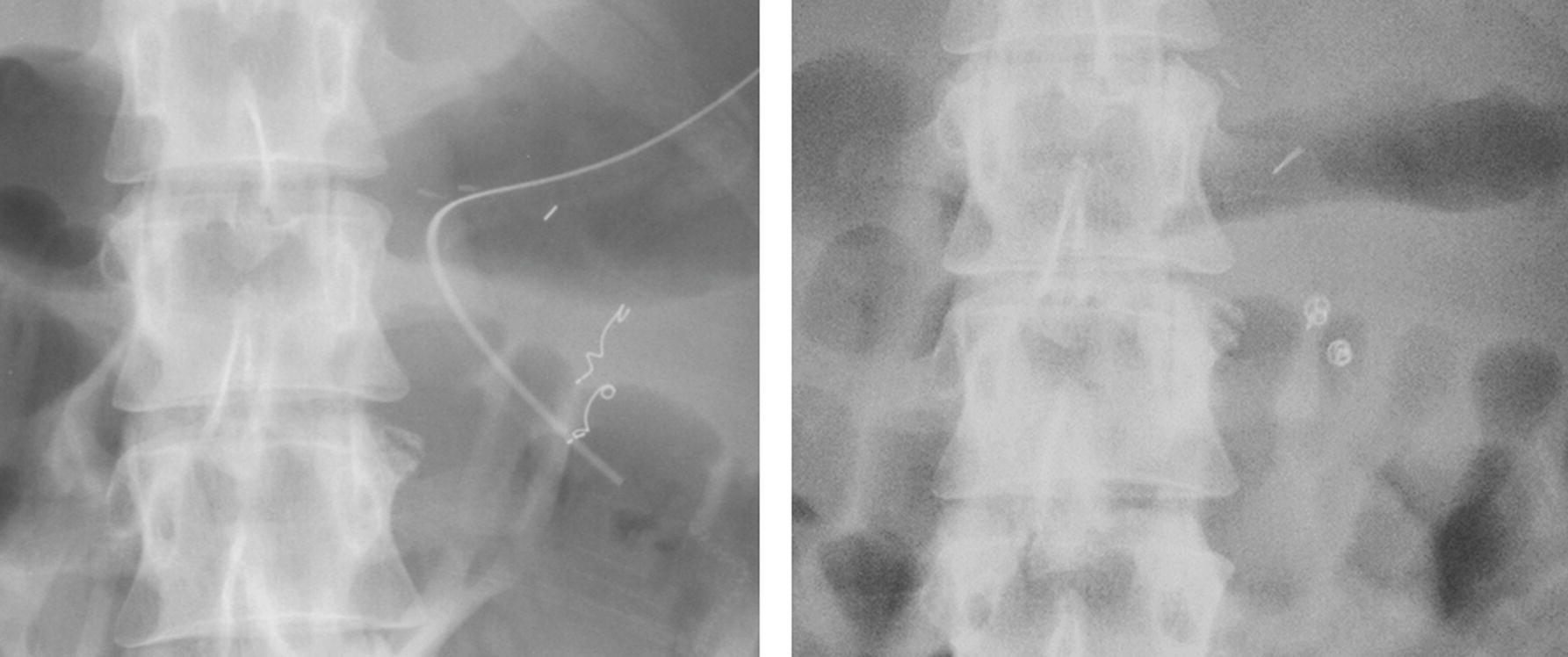
Patient 5: Initial radiograph on the left, radiograph 2 months later on the right.
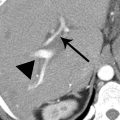
2 A 45-year-old man was imaged with contrast-enhanced CT after high-speed motor vehicle crash. What is the most likely diagnosis?
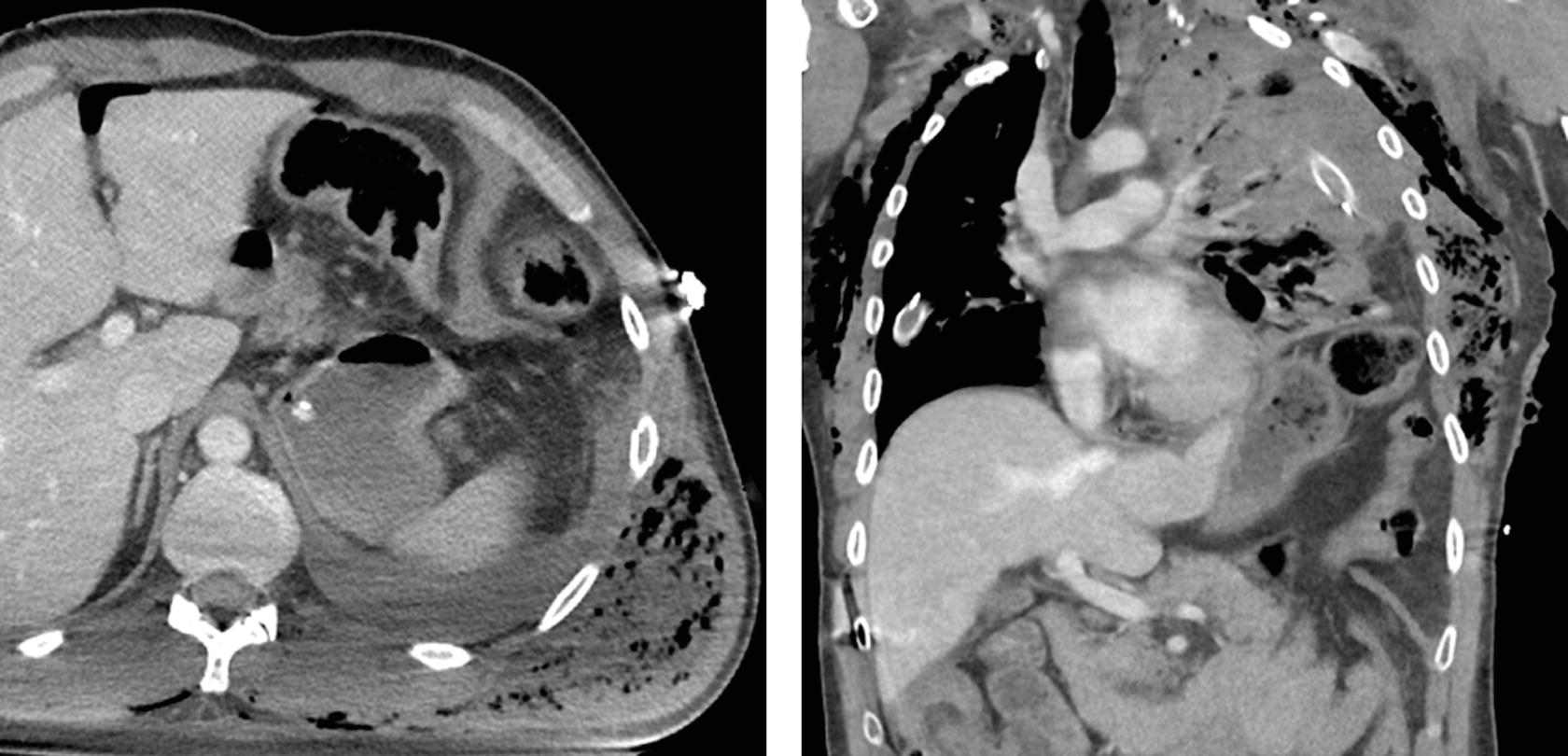
A. Traumatic diaphragmatic rupture
B. Morgagni hernia
C. Phrenic nerve dysfunction
D. Tension pneumothorax
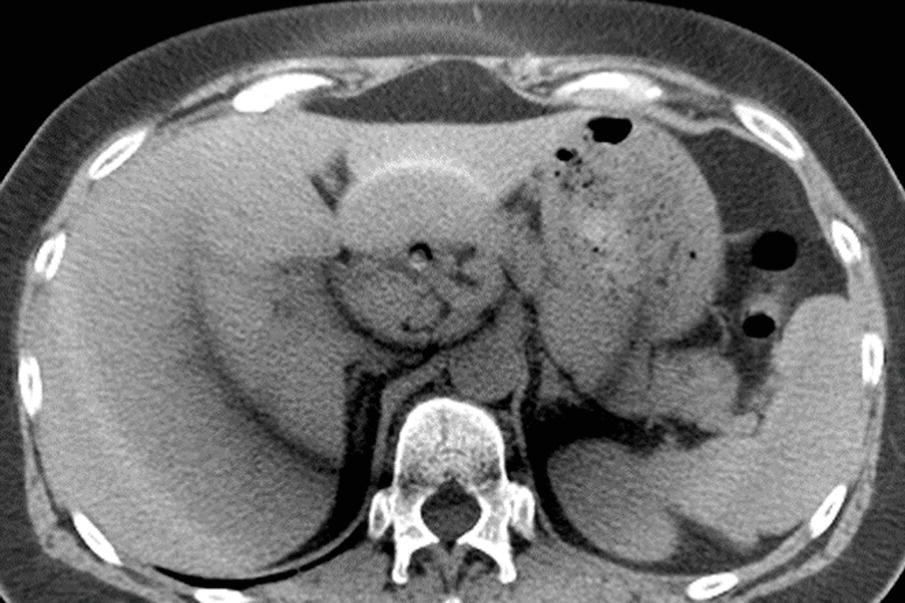
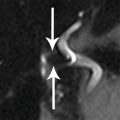
3a A 35-year-old woman presents with abdominal fullness. What is the most likely diagnosis based on the CT findings?
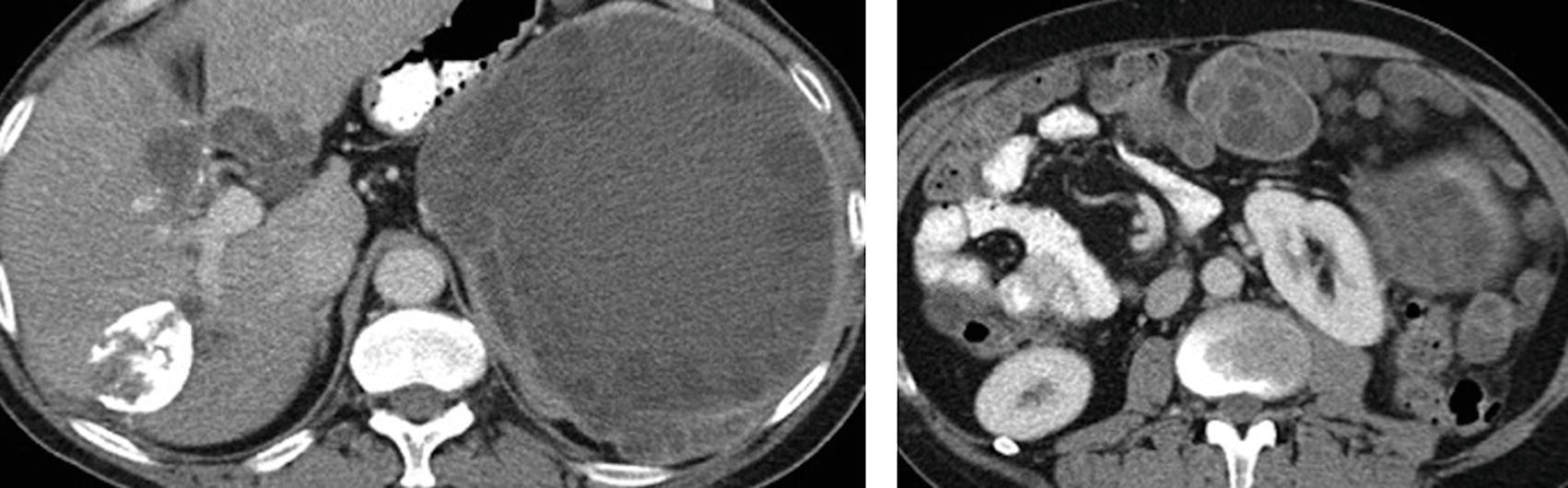
A. Amebic abscesses
B. Peritoneal carcinomatosis
C. Desmoid tumors
D. Echinococcal cysts
3b What imaging feature is demonstrated on the images in the previous question?
A. Water lily sign
B. Hydatid sand
C. Daughter cysts
D. Central dot sign
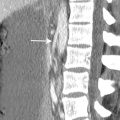
4 Axial image and sagittal image from a contrast-enhanced CT in a 20-year-old woman are shown. Her injuries are classic for which mechanism of trauma?
A. Nonaccidental abuse
B. Lap-belt compression
C. Fall from extreme height
D. Hyperextension injury
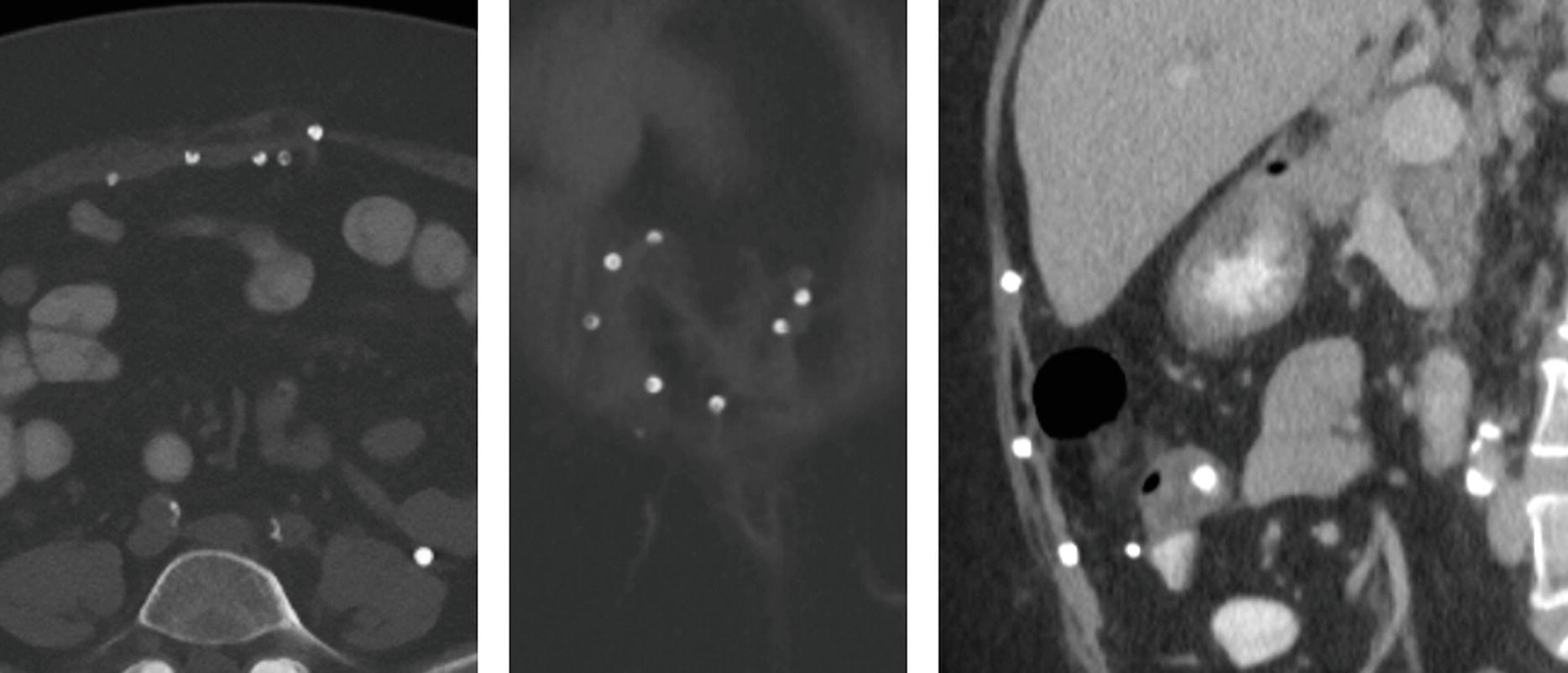
5 A patient presents with the following CT images. Serum angiotensin-converting enzyme (ACE) levels may be markedly elevated in this disease. Which of the following statements is TRUE about this disease?

A. The most common radiologic finding is lung involvement.
B. Involvement of the liver and spleen is symptomatic in most cases.
C. The disease is characterized histologically by noncaseating granulomas.
D. The most common cause of death from this disease is central nervous system involvement.
6 The findings on the following contrast-enhanced CT indicate that the patient presented with which condition?
A. Diabetic ketoacidosis
B. Small bowel obstruction
C. Sepsis
D. Trauma
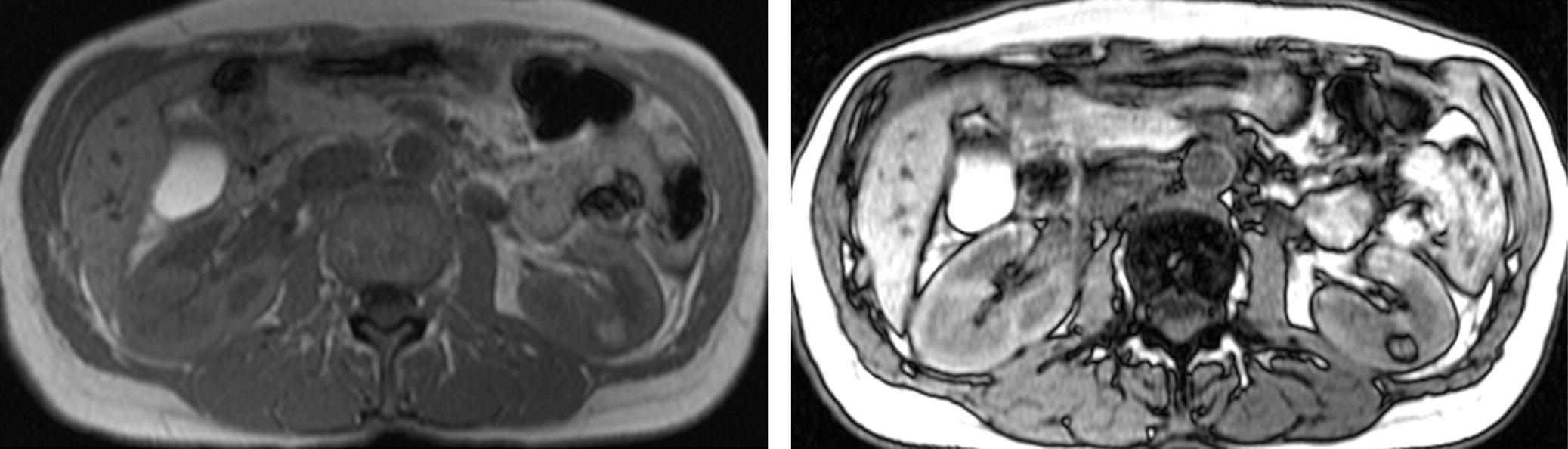
7 A 40-year-old man undergoes an abdominal CT scan. Which neoplasm is the most common cause of death in patients with the syndrome indicated by the CT finding?

A. Pheochromocytoma
B. Pancreatic ductal adenocarcinoma
C. Renal cell carcinoma
D. Pancreatic neuroendocrine tumor
8 A 51-year-old woman presents with abdominal distention, nausea, vomiting, and abdominal pain. An abdominal CT and chest radiograph are shown. Among the following malignancies, what is the most likely diagnosis of the abdominal mass?
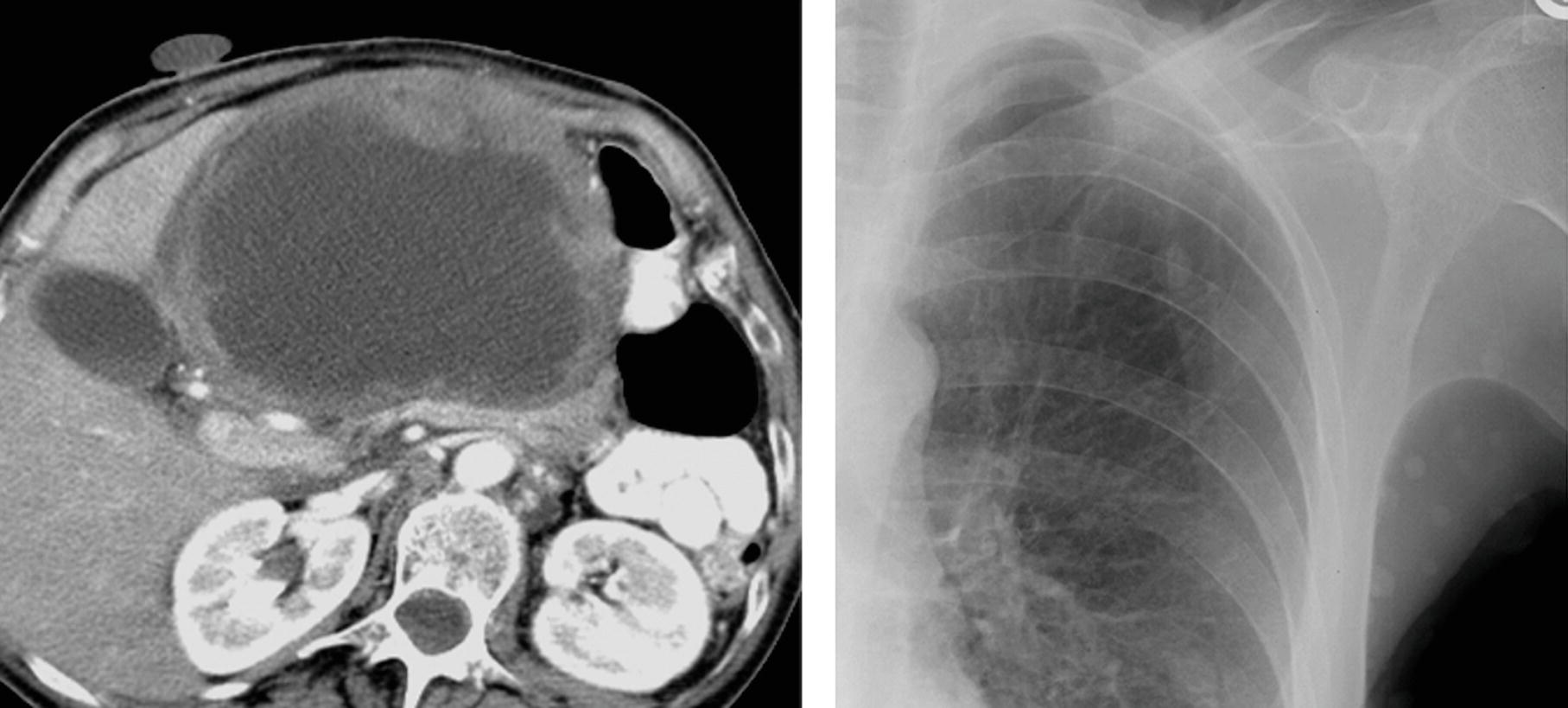
A. Angiosarcoma
B. Malignant peripheral nerve sheath tumor
C. Ovarian mucinous cystadenocarcinoma
D. Lymphoma
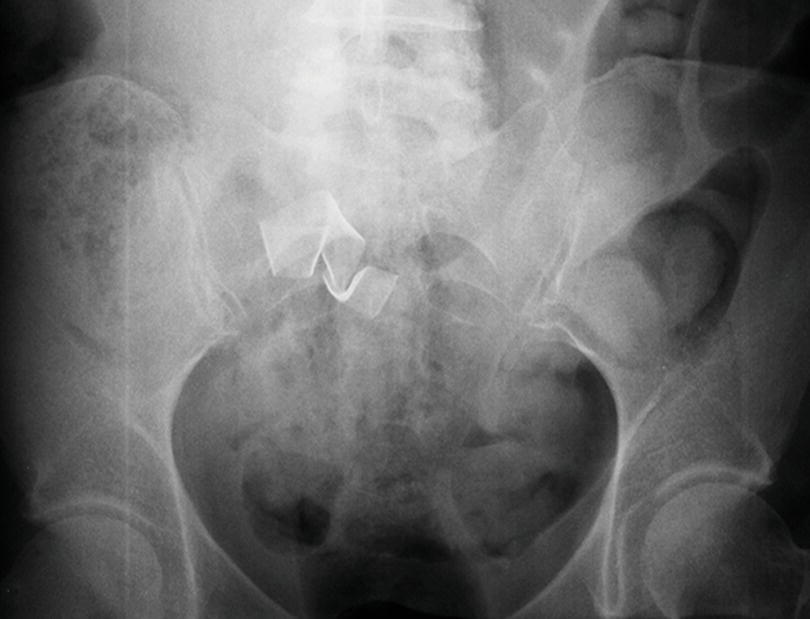
9 Match the images for Patients 1 to 4 with the correct clinical history (A to D) based on the findings shown. Each option may be used only once.
A. 93-year-old patient hospitalized for pneumonia and acute renal failure requiring dialysis, now with acute abdominal pain and decrease in hematocrit level.
B. 15-year-old patient with abnormal finding of the external genitalia at physical exam.
C. 31-year-old patient with numerous colonic polyps.
D. 42-year-old patient with cyclical abdominal wall pain.
Patient 1: Axial image from a CT without IV contrast.

Patient 2: Axial and coronal FS T1W postcontrast MR images.
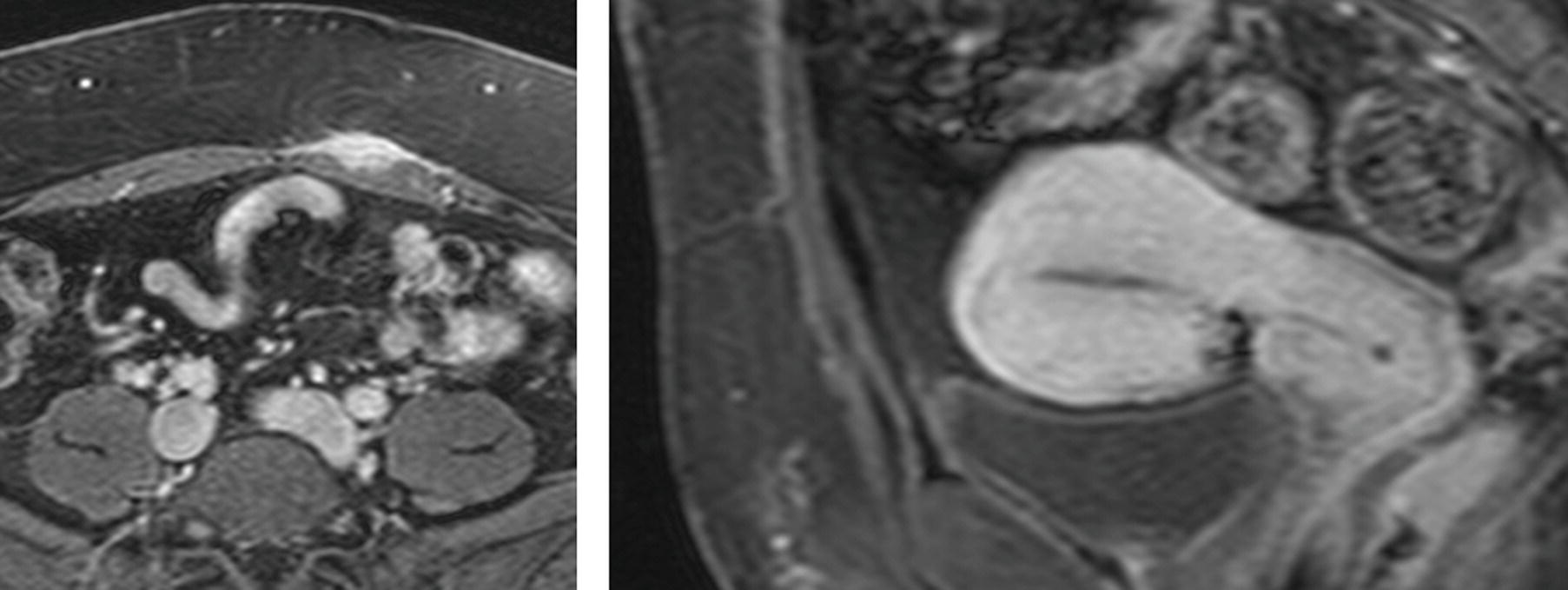
Patient 3: Axial and coronal noncontrast CT images.
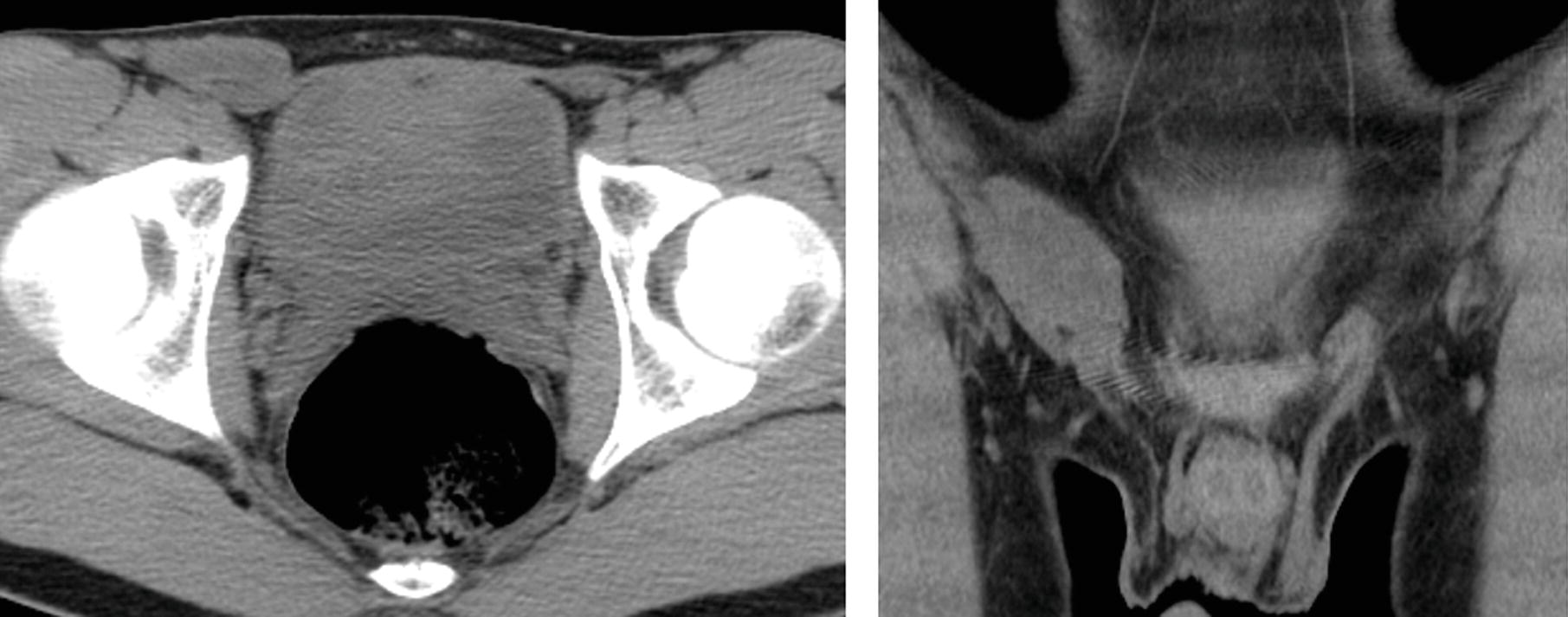
Patient 4: Axial images from contrast-enhanced CT.
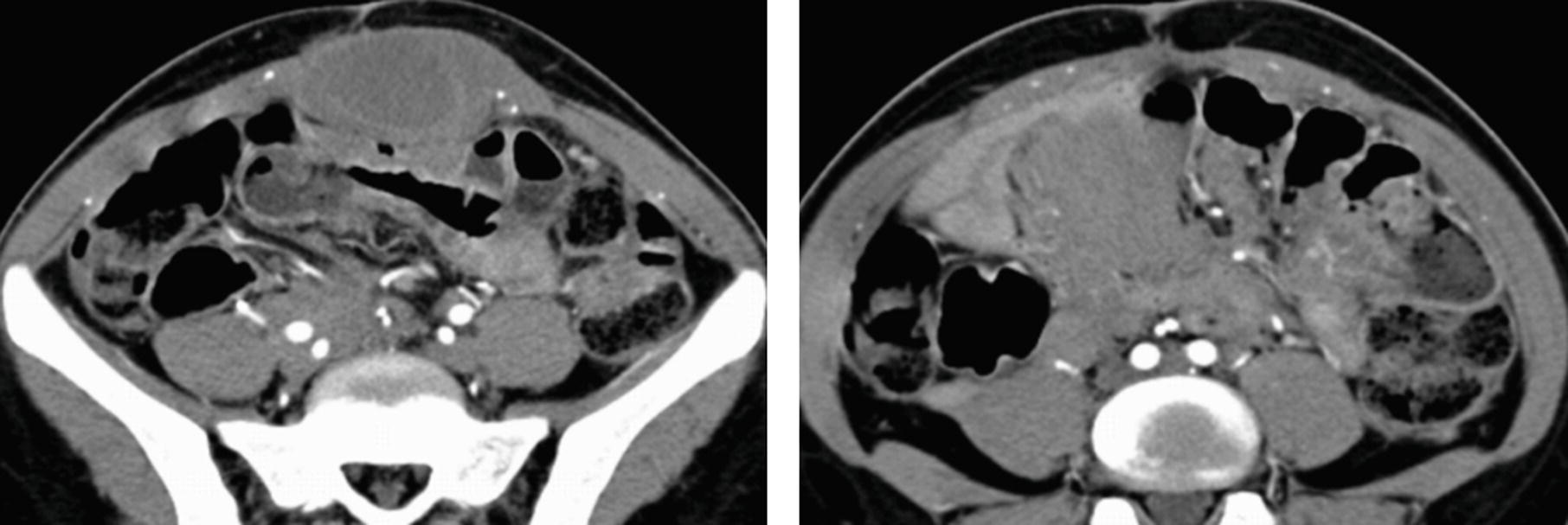
A. Beam hardening.
B. Slip ring malfunction.
C. X-ray tube arcing.
D. Detector element miscalibration or defect.
11 Which of the following techniques might decrease the conspicuity of the type of artifacts shown on the following CT images from two different patients?
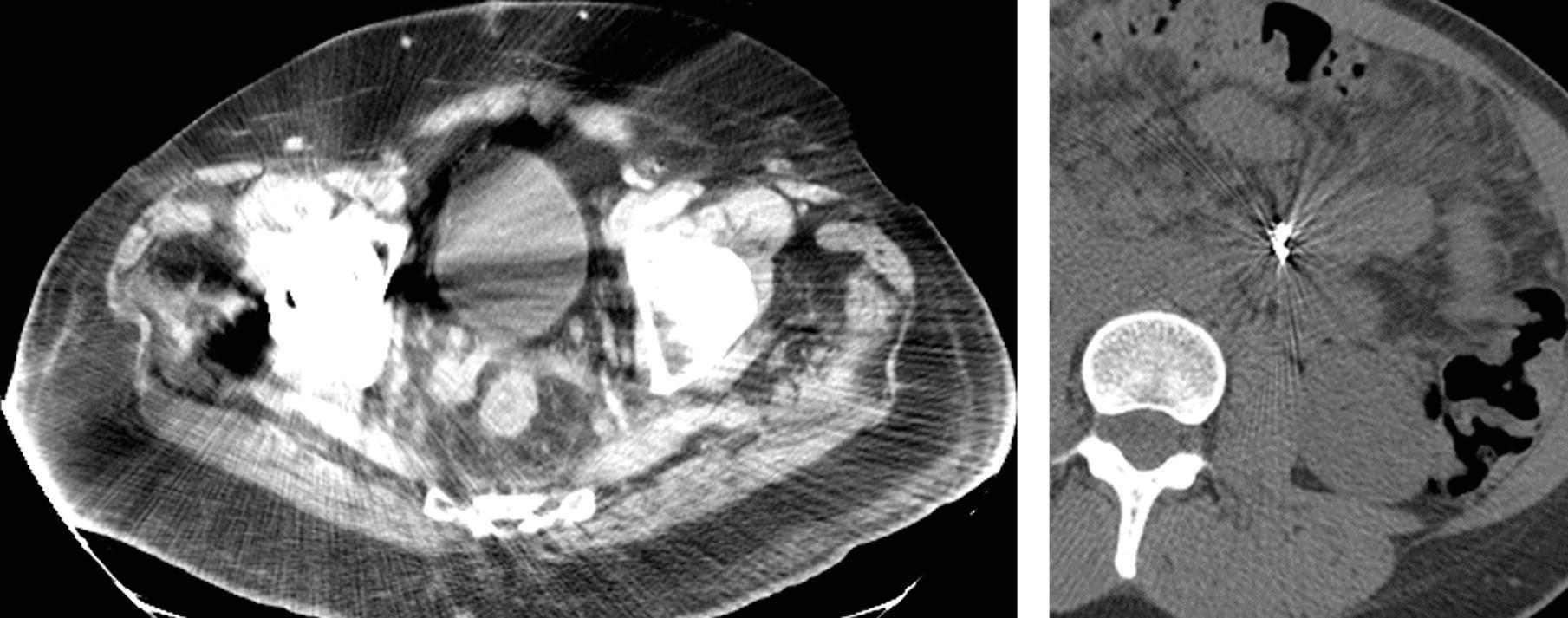
A. Increasing kVp
B. Decreasing the reconstruction slice thickness
C. Decreasing mAs
D. Decreasing the maximum window of the CT scale
12 What is TRUE about the phenomenon accounting for the signal intensity (arrows) at the margins of the kidneys on this MR image?
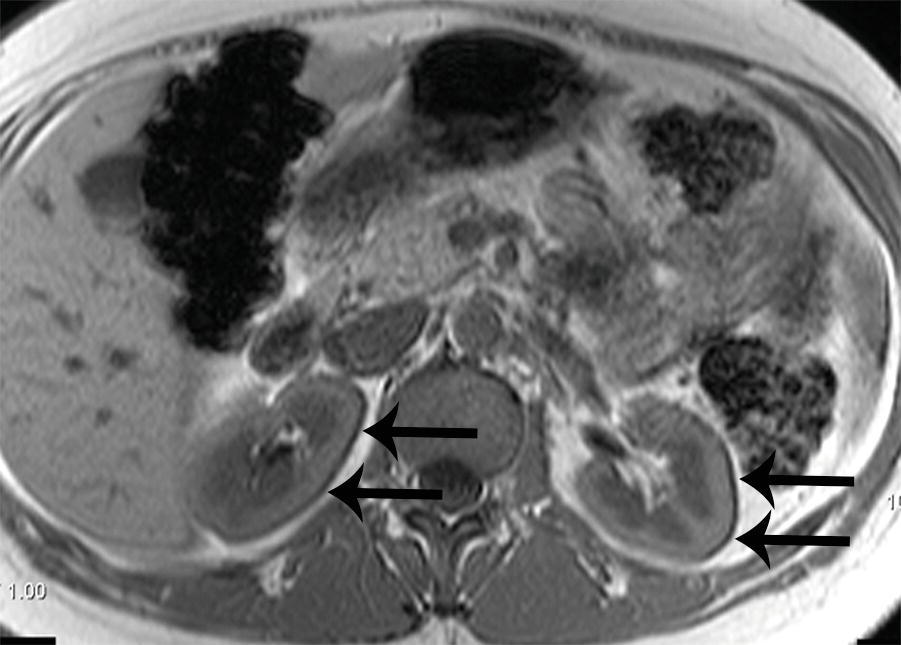
A. It occurs in the frequency- but not the phase-encoding direction.
B. It is caused by out-of-phase protons within the pixels.
C. It can be reduced by shimming.
D. It is more prominent when imaging at 1.5 tesla compared to 3 tesla.
A. Radiofrequency spike
B. Patient breathing
C. Pulsatile flow
D. Patient body habitus
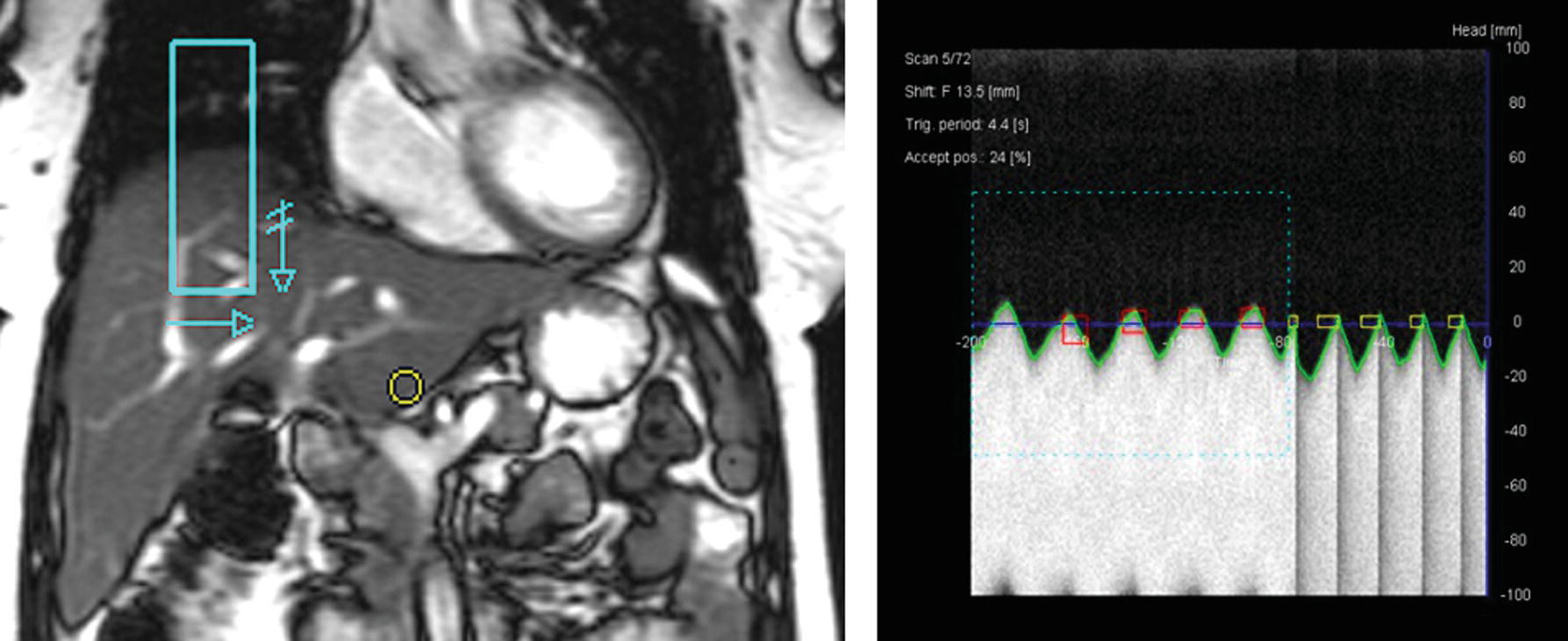
14 An abdominal MRI was performed for the evaluation of the liver. Which technique will decrease the type of artifact demonstrated?
3D gradient-echo FS T1W+gad image above the liver and image below the liver.
A. Respiratory gating
B. Frequency oversampling
C. Cardiac gating
D. Slice oversampling
A. Wraparound artifact
B. Herringbone artifact
C. Moiré fringe artifact
D. Susceptibility artifact
A. To improve frequency-selective fat saturation
B. To decrease respiratory motion artifact
C. To improve spatial resolution
D. To decrease wraparound artifact
17 Two images from the same MRI exam are presented below. What accounts for the large area of signal loss in the midabdomen?
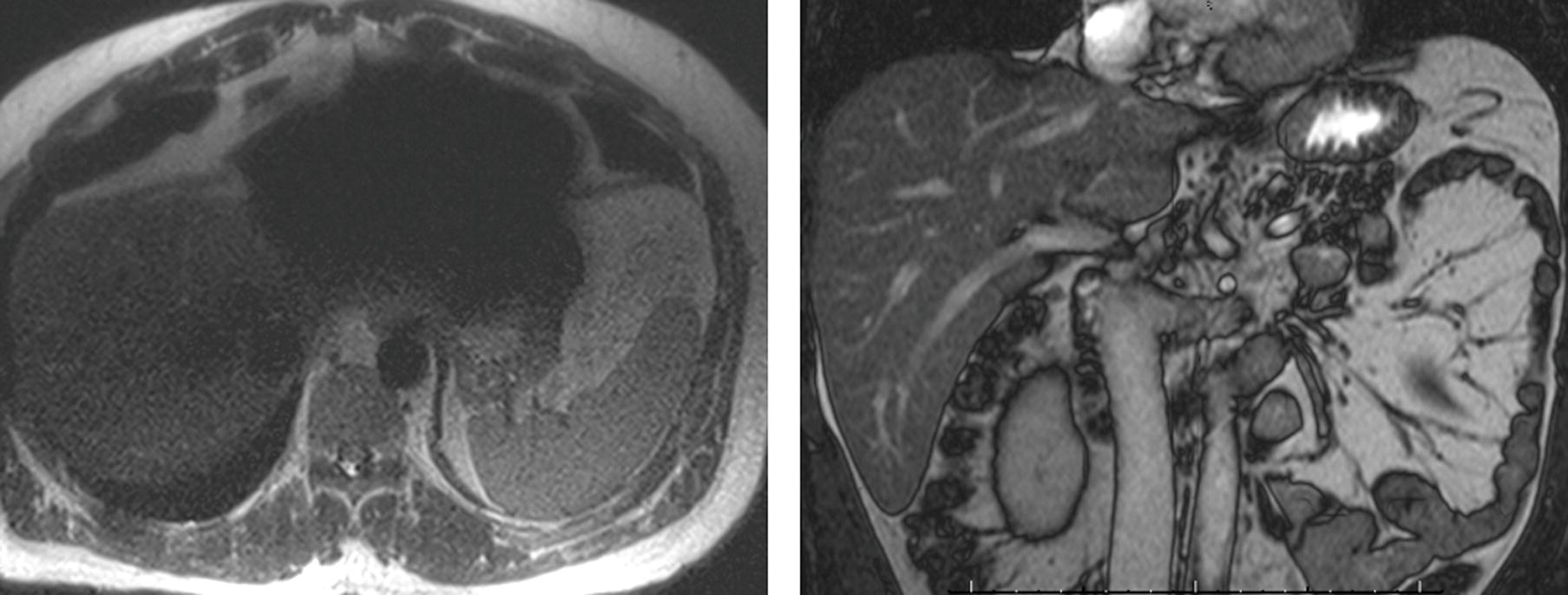
A. Dielectric effect
B. Cardiac motion
C. Flow void
D. Metallic foreign body
18 A 51-year-old woman is evaluated with an MRI for a pancreatic lesion. What is the finding incidentally noted in the left kidney?
A. Renal cyst
B. Renal angiomyolipoma
C. Clear cell renal cell carcinoma
D. Renal stone
ANSWERS AND EXPLANATIONS
1 Answers:
Patient 1: C. Suture needle
Patient 2: E. Hernia repair mesh
Patient 3: D. Brachytherapy radiation seed
Patient 4: B. Laparotomy pad
Patient 5: A. Vascular embolization microcoil
This series of patients demonstrates expected and unexpected radiopaque foreign bodies that can be seen in the abdomen and pelvis. Patients 1 and 4 have unexpected retained foreign bodies (arrows on the following images) after surgery. Patient 1 has a retained suture needle, and patient 4 has a retained surgical laparotomy pad. These items were identified by x-ray and retrieved before the patients left the operating room.
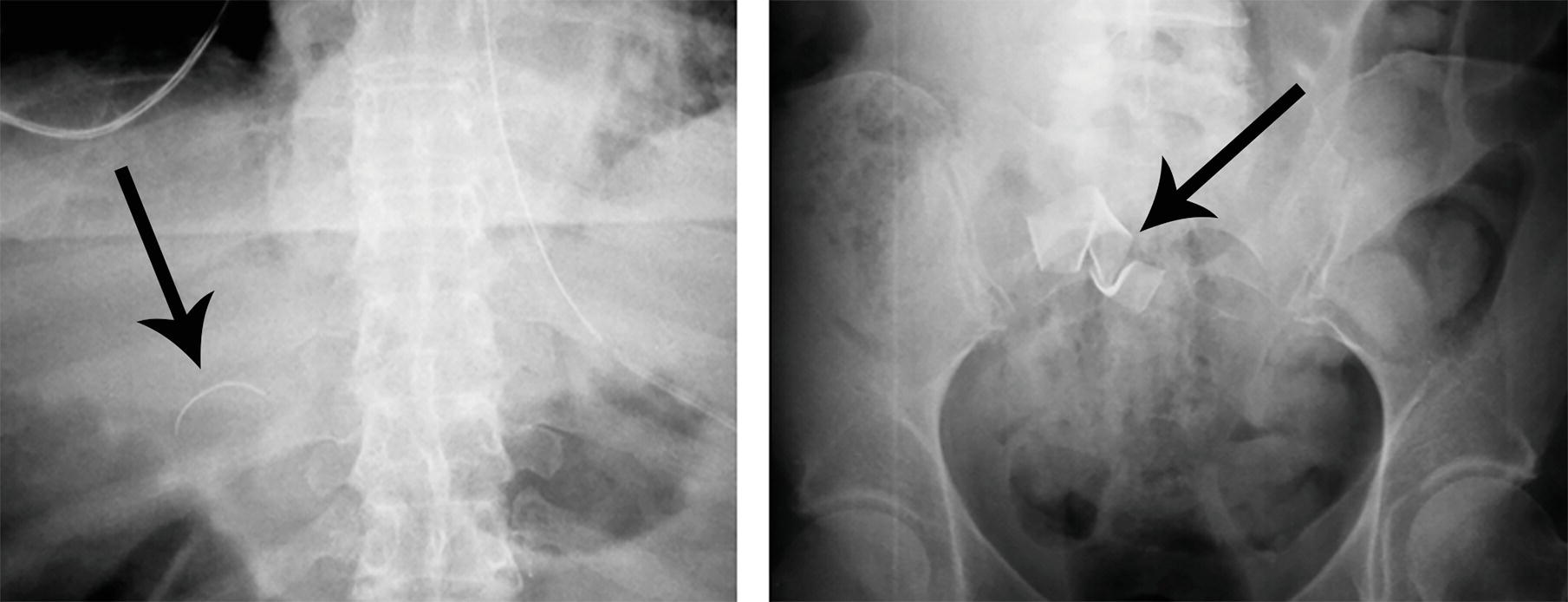
The following image shows the radiographic appearance of radiopaque surgical items, such as surgical sponges and laparotomy pads, which have thin metallic strips that allow them to be identified radiographically. Complications including infection, granulomatous reaction, bowel obstruction, or fistulae may develop immediately or years after surgery. The term “gossypiboma” is reserved for a retained mass of cotton or woven fabric. Gossypibomas classically have a spongiform appearance on CT with foci of gas and wavy layers of fabric internally. An associated radiopaque marker strip may be identified, and chronic gossypibomas may be surrounded by an enhancing fibrous capsule mimicking abscess or neoplasm.
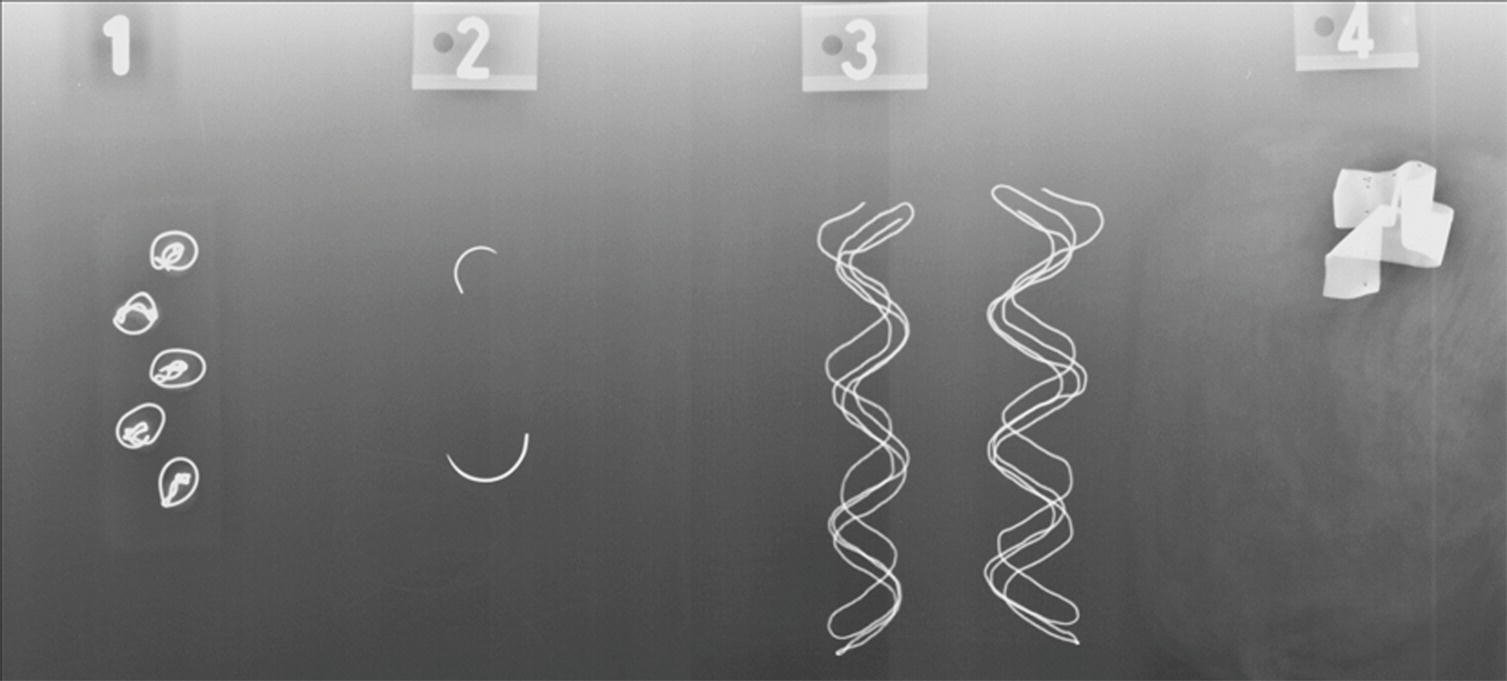
X-ray detectable surgical objects. 1—peanut sponges; 2—suture needles; 3—gauze sponges; 4—laparatomy pad (note the mass of wavy fabric faintly seen around the radiopaque tag).
Patient 2 has an abdominal wall hernia repair with mesh. This type of mesh has small round titanium anchors that are visible on radiographs or CT, but other types may not have visible anchors. The anchors are typically arranged in an ovoid configuration (short arrows on the following coronal image) at the margins of the mesh. Among the anchors, a layer representing the mesh (long arrows on the following sagittal image) is visible.
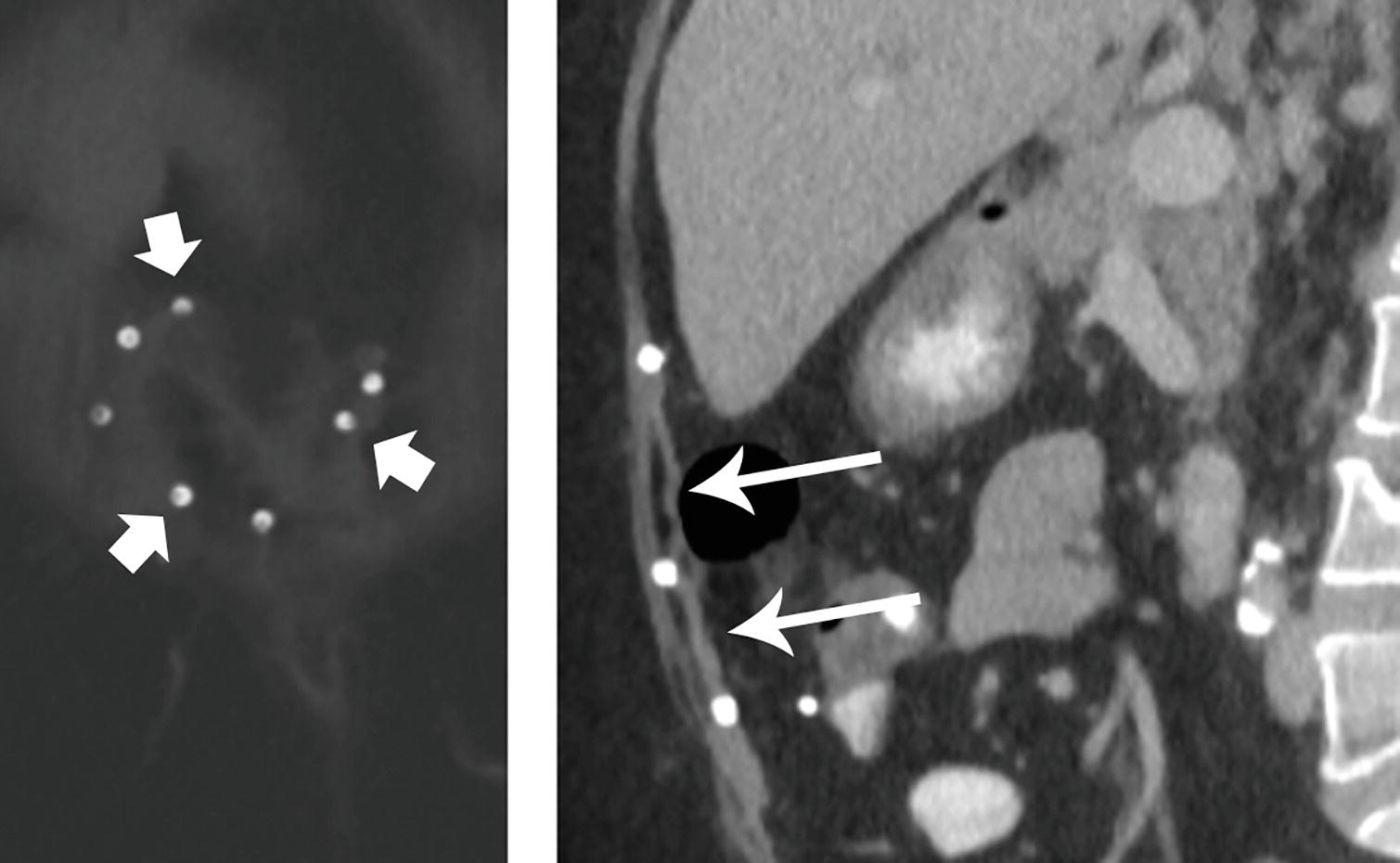
Hernia mesh with anchors.
Patient 3 has undergone brachytherapy with multiple radiation seed sources implanted in the prostate gland. These are seen as group of short linear metallic foci near the symphysis pubis.
Patient 5 has two vascular embolization microcoils in the left upper quadrant (arrows on the following images). These are initially seen as metallic wavy lines and later appear to be coiled more tightly. The patient had selective embolization of two branches of the superior mesenteric artery to treat postoperative GI bleeding. A few surgical clips are seen above the coils, and on the first image, a surgical drain is also visible.
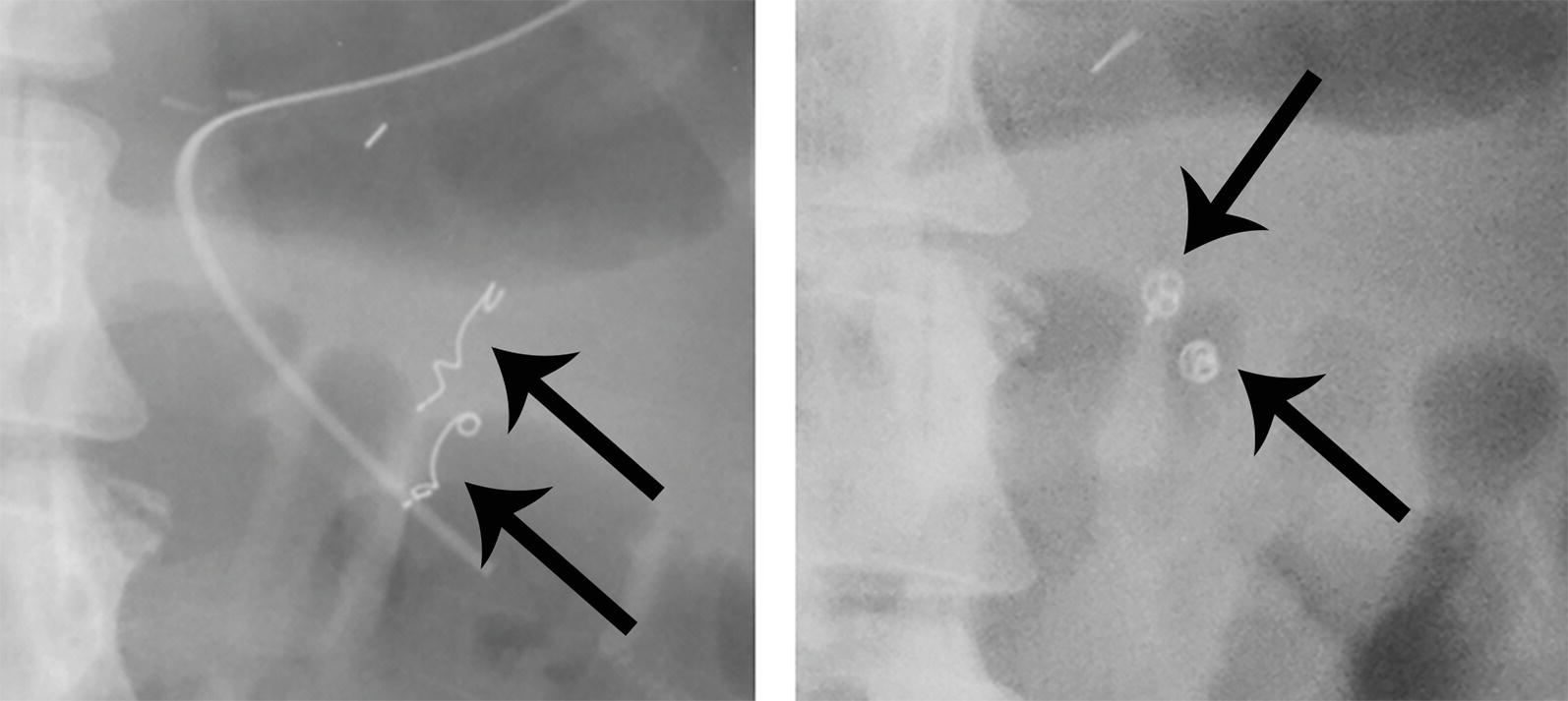
Vascular microcoils.
References: Hunter TB, Taljanovic MS. Medical devices of the abdomen and pelvis. Radiographics 2005;25(2):503–523.
Manzella A, Filho PB, Albuquerque E, et al. Imaging of gossypibomas: pictorial review. AJR Am J Roentgenol 2009;193(6 Suppl):S94–S101.
Taljanovic MS, Hunter TB, O’Brien MJ, et al. Gallery of medical devices: part 2: devices of the head, neck, spine, chest, and abdomen. Radiographics 2005;25(4):1119–1132.
2 Answer A.Axial and coronal CT images show discontinuity (arrows) of the left hemidiaphragm consistent with diaphragmatic rupture, complicated by herniation of the stomach, transverse colon, spleen, and a small portion of the left hepatic lobe into the left thorax. The left lung is compressed by the herniation and is opacified due to contusion and hemorrhage. The mediastinum is slightly shifted to the right, and no pneumothorax is identified.
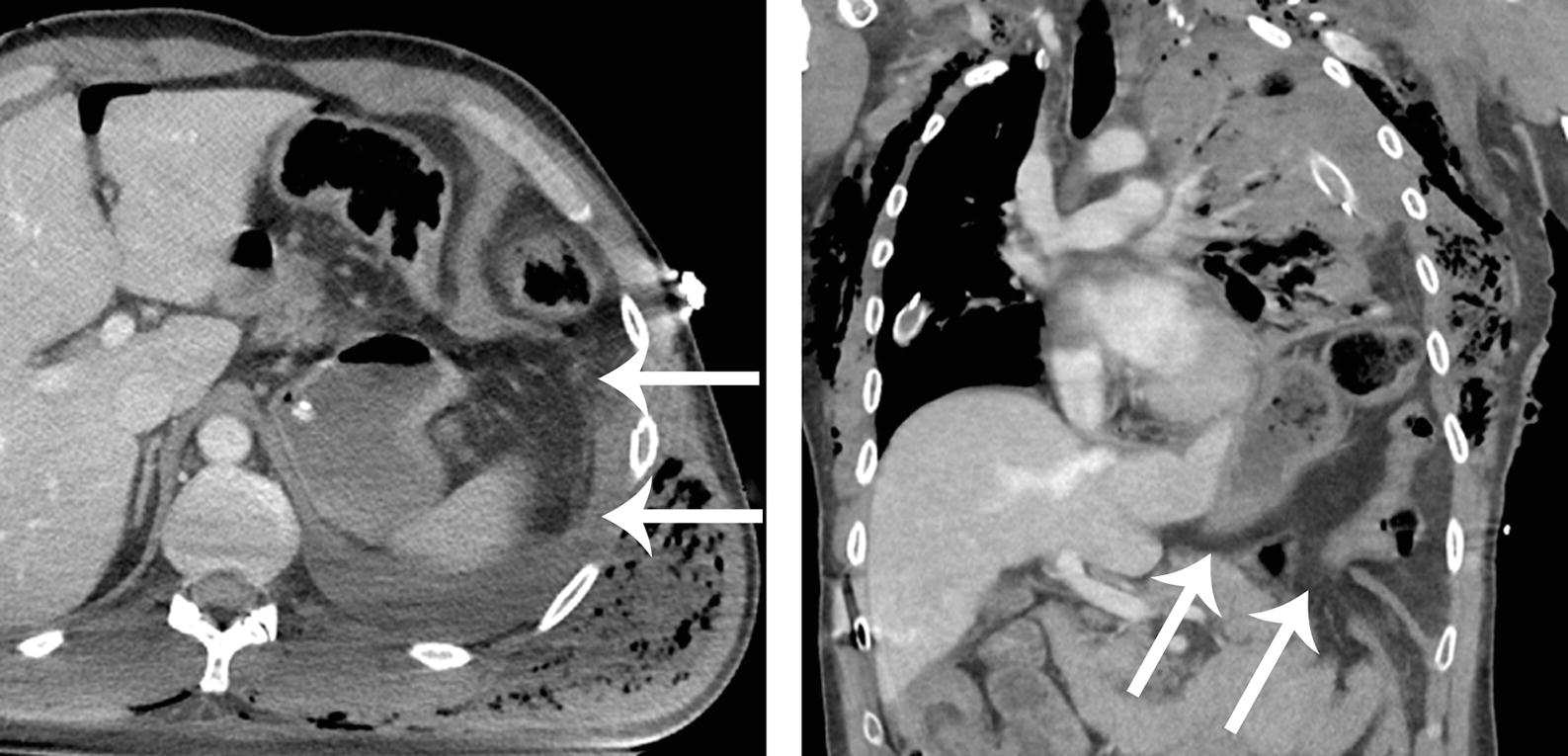
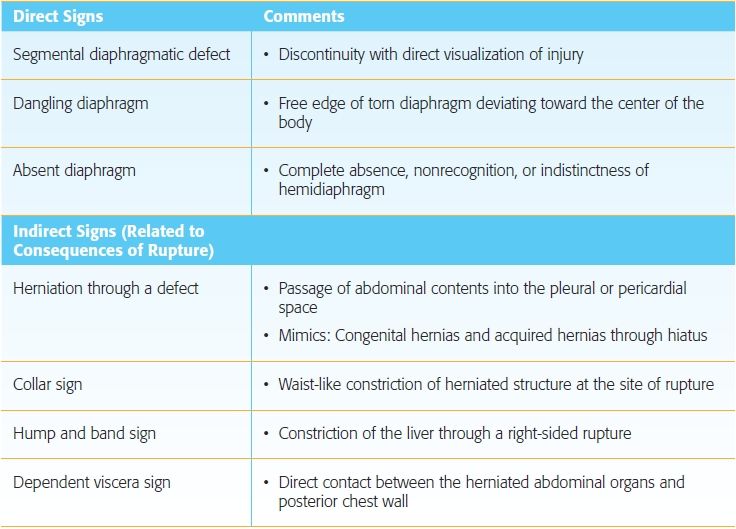
Diaphragmatic injuries are almost always associated with other injuries. The left diaphragm is ruptured more often than the right. Evaluation of the integrity of the diaphragm may be challenging, and correlation of the axial images with CT multiplanar reconstructions in the coronal and sagittal planes may be helpful. A number of direct and indirect signs of diaphragmatic rupture have variable sensitivity but excellent specificity > 90%. A few of these signs are listed in the table below. Complications of diaphragmatic rupture include bowel incarceration, obstruction, and strangulation, respiratory insufficiency, pneumonia, pleural effusion/empyema, and tension physiology from mediastinal shift. Diaphragmatic rupture requires surgical repair.
Signs of Diaphragmatic Rupture
References: Desir A, Ghaye B. CT of blunt diaphragmatic rupture. Radiographics 2012;32(2):477–498.
Iochum S, Ludig T, Walter F, et al. Imaging of diaphragmatic injury: a diagnostic challenge? Radiographics 2002;22(Spec No):S103–S116; discussion S116–S108.
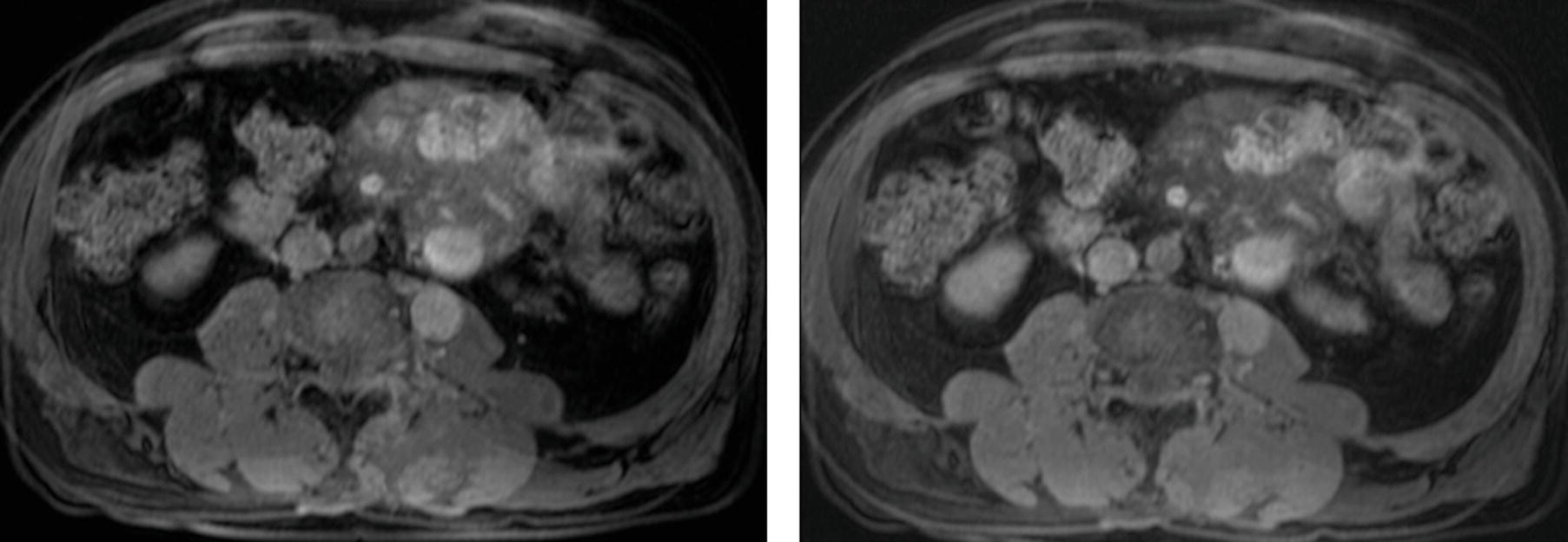
3a Answer D.
3b Answer C.This patient has disseminated echinococcal infection. There are multiple complex cystic masses with appearance pathognomonic for echinococcal (hydatid) cysts. The dominant mass replacing the spleen represents an encapsulated “mother cyst” with multiple peripheral “daughter cysts” (short white arrows) arranged in a spoke wheel, or rosette, pattern. The daughter cysts typically demonstrate lower density on CT than the mother cyst. Other similar complex cysts are seen scattered in the liver and peritoneal cavity (long white arrows).
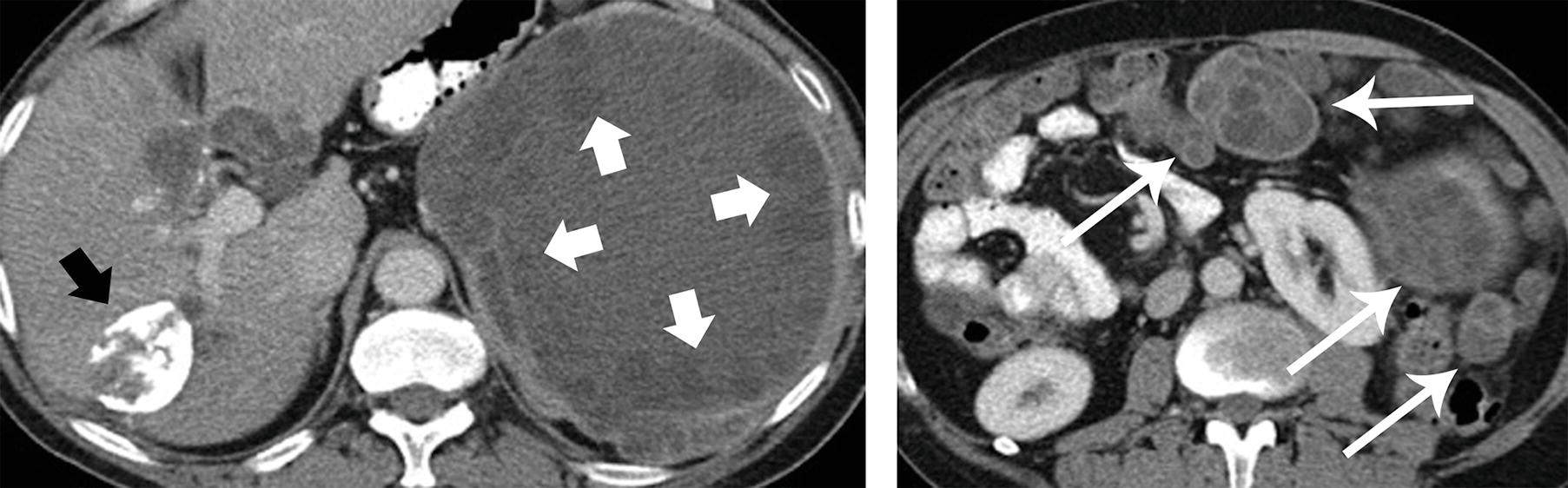
Echinococcal cysts have variable appearance, ranging from simple cysts to complex solid and cystic masses. Lesions may show calcification, and those with extensive calcification such as the one in the right lobe of the liver (short black arrow) are more likely to represent involuted inactive cysts. The “water lily sign” is also highly specific for echinococcal cysts, referring to sloughing and collapse of the internal membrane within a cyst. “Hydatid sand” represents mobile debris that can be seen in the cysts on ultrasound. When imaging features are less specific, the differential diagnosis may include cystic lesions such abscess or biliary cystadenoma/cystadenocarcinoma. Cystic or necrotic metastases may be considered if there are enhancing soft tissue components. Amebic abscesses are usually unilocular and thick walled, with appearance similar to pyogenic (bacterial) abscesses.
Hydatid disease is a parasitic infection caused by tapeworms endemic in underdeveloped parts of the world, particularly where sheep are raised. Humans are infected by ingesting water contaminated with dog feces harboring Echinococcus granulosus (more common) or Echinococcus multilocularis eggs. The liver is the most common site of involvement, seen in 75% to 80% of cases, followed by the lung. Echinococcal cysts may be complicated by peritoneal rupture, portal obstruction, biliary obstruction, and superinfection. Treatment options include surgery, percutaneous aspiration, and antiparasitic agents such as albendazole. The antiparasitic agents also prevent anaphylaxis during the procedure.
The “central dot” sign is unrelated to echinococcal cysts and is an enhancing focus associated with the cystic lesions of Caroli disease.
References: Marrone G, Crino’ F, Caruso S, et al. Multidisciplinary imaging of liver hydatidosis. World J Gastroenterol 2012;18(13):1438–1447.
Nunnari G, Pinzone MR, Gruttadauria S, et al. Hepatic echinococcosis: clinical and therapeutic aspects. World J Gastroenterol 2012;18(13):1448–1458.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree