Chapter Outline
Trauma, 283
General, 283
Spine, 287
Thoracic and Lumbar Fractures, 292
Face, 294
Shoulder, 297
Arm, 302
Wrist/Hand, 305
Lower Extremity, 311
Ankle, 319
Foot, 322
Orthopedic Procedures, 324
Arthrography, 326
Biopsies of the Musculoskeletal System, 328
Percutaneous Periradicular Steroid Injection, 329
Percutaneous Cementoplasty, 329
Bone Tumors, 329
General, 329
Bone-Forming Tumors, 333
Cartilage-Forming Tumors, 335
Fibrous Lesions, 336
Bone Marrow Tumors, 338
Metastases, 340
Other Bone Tumors, 341
Miscellaneous Lesions, 343
Arthritis, 345
General, 345
Degenerative Arthritis, 346
Inflammatory Arthritis, 348
Metabolic Arthritis, 353
Infectious Arthritis, 356
Metabolic Bone Disease, 357
Differential Diagnosis, 365
Focal Bone Lesions, 365
Joints, 367
Bone Density, 369
Periosteum, 370
Skull, 370
Spine, 370
Pelvis, 373
Lower Extremity, 373
Upper Extremity, 374
Soft Tissues, 376
Trauma
General
Fracture
| Fracture | Finding |
|---|---|
| Spine | |
| Jefferson | Ring fracture of C1 |
| Hangman’s | Bilateral pedicle or pars fractures of C2 |
| Teardrop (flexion) | Unstable flexion fracture |
| Clay-shoveler’s | Avulsion fracture of spinous process lower cervical, high thoracic spine |
| Chance | Horizontal fracture through soft tissues and/or bone of thoracolumbar spine |
| Burst | Compression fracture with disruption of the posterior vertebral body with retropulsion into the spinal canal |
| Face | |
| All Le Fort fractures involve the pterygoid plates | |
| Le Fort I | Floating palate |
| Le Fort II | Floating maxilla |
| Le Fort III | Floating face |
| Upper Extremity | |
| Hill-Sachs lesion (anterior dislocation) | Impaction fracture of posterolateral humeral head |
| Bankart lesion (anterior dislocation) | Fracture of anterior glenoid rim |
| Trough sign (posterior dislocation) | Linear impaction fracture of anterior humeral head |
| Reverse Bankart lesion (posterior dislocation) | Fracture of posterior glenoid rim |
| Monteggia fracture-dislocation | Ulnar fracture, proximal radial dislocation |
| Galeazzi fracture-dislocation | Radial fracture, distal radioulnar dislocation |
| Essex-Lopresti | Radial head fracture and distal radioulnar subluxation |
| Colles | Distal radius fracture, dorsal angulation |
| Smith | Distal radius fracture, volar angulation |
| Barton | Intraarticular distal radial fracture/dislocation through dorsal articular surface |
| Reverse Barton intraarticular distal radial fracture through volar articular surface | |
| Bennett | Fracture-dislocation of base of first metacarpal |
| Rolando | Comminuted Bennett fracture |
| Boxer’s | 5th MCP shaft or neck fracture |
| Gamekeeper’s thumb (skiers) | Ulnar collateral ligament injury of 1st MCP joint |
| Chauffeur’s | Intraarticular fracture of radial styloid |
| Pelvis | |
| Duverney | Iliac wing fracture |
| Malgaigne | SI joint or sacrum and both ipsilateral pubic rami |
| Bucket-handle | SI joint or sacrum and contralateral pubic rami |
| Straddle | Fracture of both obturator rings (all four pubic rami) |
| Lower Extremity | |
| Segond | Avulsion fracture of lateral tibial condyle; associated with ACL injury |
| Bumper | Intraarticular fracture of tibial condyle |
| Pilon | Intraarticular comminuted distal tibia fracture |
| Tillaux | Salter-Harris III of lateral distal tibia (because of later epiphyseal fusion) |
| Triplane | Salter III/IV fracture of distal tibia |
| Wagstaffe-Le Fort | Avulsion of the medial margin distal fibula |
| Dupuytren | Fracture of fibula above tibiofibular ligament |
| Maisonneuve | Proximal fibular fracture and disrupted ankle mortise or medial malleolar fracture |
| Lover’s | Calcaneal fracture |
| Jones (dancer’s) | Fracture of proximal 5th metatarsal shaft |
| Lisfranc | Tarsometatarsal fracture-dislocation |
| March | Stress fracture of metatarsal neck |
Fracture Healing ( Fig. 5.1 )
Phases of healing:
Inflammatory phase
- •
Torn periosteum
- •
Blood clots in fracture line
- •
Inflammatory reaction
- •
Reparative phase
- •
Granulation tissue replaces clot.
- •
Periosteum forms immature callus.
- •
Internal callus forms within granulation tissue.
- •
Cartilage forms around fracture.
- •
Remodeling phase
- •
Woven bone in callus is replaced by compact bone (cortex) and cancellous bone (medullary cavity).
- •

Terminology for Description of Fractures
Anatomic site of fracture
- •
In long bones, divide the shaft into thirds (e.g., fracture distal third of femur).
- •
Use anatomic landmarks for description (e.g., fracture near greater tuberosity).
- •
Pattern of fracture
- •
Simple fracture: no fragments. Describe the direction of the fracture line: transverse, oblique, spiral, longitudinal
- •
Comminuted fracture (more than two fragments): T-, V-, Y-shaped patterns, butterfly fragments, segmental
- •
Complete or incomplete fractures
- •
Apposition and alignment: defined in relation to distal fragments
- •
Displacement (e.g., medial, lateral, posterior, anterior)
- •
Angulation (e.g., medial, lateral, posterior, anterior)
- •
Rotation (internal, external)
- •
Overriding: overlap of fragments (bayonet apposition)
- •
Distracted: separated fragments
- •
Adjacent joints
- •
Normal
- •
Dislocation
- •
Subluxation
- •
Intraarticular extension of fracture line
- •
Specific Fractures
- •
Stress fractures:
Fatigue fracture: abnormal muscular stress applied to normal bone (e.g., march fracture)
Insufficiency fracture: normal muscular stress applied to abnormal bone (e.g., osteoporotic vertebral fracture)
- •
Pathologic fracture: fracture superimposed on underlying bone disease
- •
Intraarticular fracture: fracture line extends into joint
- •
Salter-Harris fracture: fractures involving growth plate
- •
Pseudofracture: fissure like defects in osteomalacia (Looser zones)
- •
Occult fracture: suspected but nonvisualized fracture on plain radiograph; demonstrated by 99m technetium (Tc) methylene diphosphonate (MDP) scintigraphy or magnetic resonance imaging (MRI)
- •
Hairline fracture: nondisplaced fracture with minimal separation
- •
Avulsion fracture: fragment pulled away from bone at tendinous and ligament insertion (commonly at tuberosity)
- •
Apophyseal fracture: at growth centers such as ischial tuberosity and medial epicondyle; commonly avulsion fractures
Relevant Anatomy ( Fig. 5.2 )
Bone is composed of calcium hydroxyapatite on a matrix of collagen and other proteins. Thick outer cortex surrounds cancellous (or trabecular) bone, and both contribute to bone strength. Bone is covered by periosteum, except at the joints, where it is covered with cartilage. Normal bone undergoes constant balanced turnover, bone resorption is facilitated by osteoclasts, bone production by osteoblasts. As per Wolff law, an increase in bone stress shifts the balance toward bone production. Vice versa, decreased bone loading leads to decreased bone mass.

Long Bones
- •
Epiphysis
- •
Metaphysis
- •
Diaphysis
Types of Joints
Synovial joint (diarthrosis)
- •
Appendicular skeleton
- •
Facet joints of spine
- •
Atlantoaxial joints
- •
Lower two-thirds of sacroiliac (SI) joints
- •
Acromioclavicular (AC) joint
- •
Uncovertebral joints
- •
Cartilaginous joint (amphiarthrosis)
- •
Synchondroses (temporary: physis; permanent: ribs, first sternocostal joint)
- •
Pubic symphysis
- •
Intervertebral disks
- •
Fibrous joint (synarthrosis)
- •
Tibiofibular and radioulnar syndesmosis
- •
Cranial sutures
- •
Gomphoses (dentoalveolar joints)
- •
Superior portions of SI joints
- •
Synovial Joint ( Fig. 5.3 )
In contradistinction to fibrous and cartilaginous joints, synovial joints allow wide ranges of motion and are classified according to axes of movement. The articular cartilage is hyaline. The most superficial layer has collagen fibrils parallel to the surface with microscopic pores to allow passage of electrolytes. This is also referred to as the armor plate. Deeper in the cartilage, collagen fibrils are arranged in arcades to give flexibility and allow for compression. Proteoglycans within the cartilage bind water to give a cushion effect.

Cartilaginous Joint
Cartilaginous joints are covered with fibrocartilage, and allow for limited range of motion. There is no synovial lining and there is often a central disk.
Fibrous Joint
Fibrous joints are the strongest joints, allowing almost no motion. Fibrous tissue is between bones.
Fracture Complications
Immediate
- •
Hemorrhage, shock
- •
Fat embolism
- •
Acute ischemia (5 Ps : p ulselessness, p ain, p allor, p aresthesia, p aralysis)
- •
Spinal cord injury, epidural hematoma
- •
Delayed
- •
Nonunion
- •
Osteoporosis caused by disuse
- •
Secondary osteoarthritis (OA)
- •
Myositis ossificans
- •
Osteomyelitis
- •
Osteonecrosis
- •
Sudeck atrophy
- •
Volkmann ischemic contracture
- •
Orthopedic Procedures
Types of Repair
Reduction
- •
Closed: skin intact; may be performed in surgery under general anesthesia
- •
Open: requires exposing the fracture site in surgery
- •
Fixation
- •
Internal: using fixation devices such as plates, screws, rods; a subsequent operation is usually necessary to remove hardware.
- •
External: cast or external fixator
- •
Orthopedic Hardware
- •
Intramedullary rods: most of the intramedullary rods are hollow, closed nails; proximal and distal interlocking screws prevent rotation and shortening of bone fragments.
- •
Kirschner wires (K-wires): unthreaded segments of wires drilled into cancellous bone; if more than one wire is placed, rotational stability can be achieved; the protruding ends of the K-wire are bent to prevent injury; K-wires are most frequently used for:
Provisional fixation
Fixation of small fragments
Pediatric metaphyseal fractures
- •
Cerclage wires are used to contain bone fragments.
- •
Staples are commonly used for osteotomies.
- •
Plates
- •
Nails
- •
Screws
Spine
Classification of Cervical Spine (C-Spine) Injuries
| Type of Injury | Condition | Stability a |
|---|---|---|
| Flexion | Anterior subluxation | Stable b |
| Unilateral facet dislocation | Stable | |
| Bilateral facet dislocation | Unstable | |
| Wedge compression fracture | Stable b | |
| Flexion teardrop fracture | Unstable | |
| Clay-shoveler’s fracture | Stable | |
| Extension | Posterior arch of C1 fracture | Stable |
| Hangman’s fracture | Unstable | |
| Laminar fracture | Stable | |
| Pillar fracture | Stable | |
| Extension teardrop fracture | Stable | |
| Hyperextension dislocation-fracture | Unstable | |
| Compression | Jefferson fracture | Unstable |
| Burst fracture | Stable | |
| Complex | Odontoid fractures | Unstable |
| Atlantooccipital disassociation | Unstable |
a Stability is a function of ligamentous injury. Plain radiographs in neutral position allow one to infer instability when certain fractures or dislocations are present. However, stability may not be inferred with 100% accuracy. The anterior subluxation injury in which radiographs may appear within normal limits is an example. Clinical judgment is necessary to decide whether to do nothing, obtain flexion/extension radiographs, or obtain a magnetic resonance imaging (MRI) scan.
Biomechanics ( Figs. 5.4–5.5 )

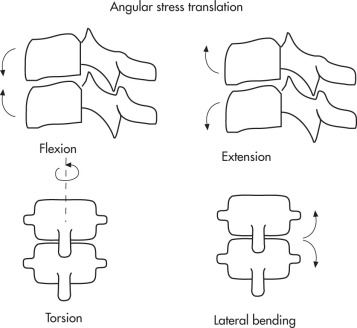
Pearls
- •
20% of spinal fractures are multiple.
- •
5% of spinal fractures are at discontinuous levels.
- •
Spinal cord injury occurs:
At time of trauma, 85%
As a late complication, 15%
- •
Cause of spinal fractures
Motor vehicle accident (MVA), 50%
Falls, 25%
Sports related, 10%
- •
Most spinal fractures occur in upper (C1–C2) or lower (C5–C7) cervical spine and thoracolumbar (T10–L2) region.
Approach to C-Spine Plain Radiograph ( Figs. 5.6–5.7 )
- 1.
Are all seven cervical vertebrae well seen? If not, obtain additional views such as swimmer’s view, computed tomography (CT), etc.
- 2.
Is cervical lordosis maintained? If not, consider:
- •
Positional
- •
Spasm
- •
Fracture/injury
- •
- 3.
Evaluate five parallel lines for stepoffs and/or discontinuity.
- •
Prevertebral soft tissues
C3–C4: 5 mm from vertebral body is normal (nonportable radiograph)
C4–C7: 20 mm from vertebral body is normal (not as reliable)
Contour of soft tissues is as important as absolute measurements; a localized bulging anterior convex border usually indicates pathology.
- •
Anterior longitudinal line
- •
Posterior longitudinal line
- •
Spinolaminar line
- •
Posterior spinous process line
- •
- 4.
Inspect C1–C2 area.
- •
Atlantodental distance (normal distance indicates intact transverse atlantal and alar ligaments)
- •
Adults: <3 mm is normal.
- •
Children: <5 mm is normal.
- •
Base of odontoid may not be calcified in children (subdental synchondrosis).
- •
- 5.
Inspect disk spaces.
- •
Narrowing of disk spaces?
- •
- 6.
Transverse processes: C7 points downward, T1 points upward.
- 7.
Pearls for C-spine plain radiographs in children:
- •
Atlantoaxial distance <5 mm is normal (ligamentous laxity, compare with <3 mm in adults).
- •
Pseudo-Jefferson fracture: up to 6 mm displacement of the lateral masses of C2 can be seen on open-mouth view up to 7 years age.
- •
On flexion views, widening of the interspinous distance between C1 and C2 is normal.
- •
Lateral pseudoluxation of C2–C3 and to a lesser extent C3–C4. If posterior cervical line is within 1 mm in both flexion and extension, then no true injury is present.
- •
Absence of normal cervical lordosis can be seen up to 16 years age.
- •
Wedging of cervical vertebral bodies up to 3 mm, especially C3, can be normal.
- •
Do not confuse ossification centers with open synchondroses (smooth, regular structures with subchondral sclerotic lines) with fractures (irregular, not sclerotic acutely). Synchondroses at C2 may simulate type 3 dense fracture.
- •
Apparent prevertebral soft tissue swelling may be due to expiration and/or flexion, repeat image in inspiration and slight extension.
- •


Approach to Cervical Spine Injuries
- 1.
Most suspected C-spine fractures are followed with thin-section CT with reformation for most accurate evaluation.
- 2.
Patients with history/examination highly suggestive of cervical spine injury (high-speed accident) proceed directly to CT, followed by an out-of-collar lateral to clear cervical spine.
- 3.
All individuals with signs/symptoms of cord injury require MRI.
- 4.
It is also prudent to obtain CT in patients with unexplained prevertebral soft tissue swelling.
Jefferson Fractures ( Fig. 5.8 )
Compression force to C1 that usually results from blow to the vertex of the head (diving injury).

Consists of unilateral or bilateral fractures of both the anterior and posterior arches of Cl. Treatment is halo placement for 3 months.
Radiographic Features
- •
Key radiographic view: anteroposterior (AP) open-mouth
- •
Displacement of C1 lateral masses
<2 mm bilateral is always abnormal in adults.
<1–2 mm or unilateral displacement can be due to head tilt/rotation.
- •
CT required for:
Defining full extent of fracture
Detecting fragments in spinal cord
Fractures of the Odontoid Process (Dens) ( Fig. 5.9 )
Various mechanisms: Anderson/D’Alonzo classification:
- •
Type I: fracture in the upper part of the odontoid (potentially unstable; rare fracture).
- •
Type II: fracture at base of the odontoid (unstable); highest rate of nonunion because fracture is above the accessory ligament and vascular supply.
- •
Type III: fracture through base of odontoid into body of axis; best prognosis for healing because of larger surface area (unstable).

Radiographic Features
- •
Anterior tilt of odontoid on lateral view is highly suggestive of fracture.
- •
Plain radiograph tomograms or CT with reformations are helpful to delineate fracture line.
- •
Prevertebral soft tissue swelling (may be the only sign)
- •
Os odontoideum (type II)
Congenital or posttraumatic
May be mechanically unstable
- •
Os terminale (type I)
- •
Ossification center that normally fuses by age 12, but may remain persist unfused simulating a type I dens fracture.
Hangman’s Fracture ( Fig. 5.10 )
Hyperextension and traction injury of C2.

Causes
- •
Hanging
- •
MVA (chin hits dashboard)
Radiographic Features
- •
Best demonstrated on lateral view
- •
Bilateral C2 pars (common) or pedicle (less common) fractures
- •
Anterior dislocation or subluxation of C2 vertebral body
- •
Avulsion of anterior inferior corner of C2 (ruptured anterior longitudinal ligament)
- •
Prevertebral soft tissue swelling
Burst (Compression) Fracture
Same mechanism as in Jefferson fracture but located at C3–C7. Injury to spinal cord (displacement of posterior fragments) is common. All patients require CT to evaluate full extent of injury, to detect associated fractures, and to identify fragments in relation to spinal canal.
Flexion Teardrop Fracture (Flexion Fracture-Dislocation)
The most severe C-spine injury. Results from severe flexion force and presents as clinical “acute anterior cord syndrome” (quadriplegia, loss of anterior column senses, retention of posterior column senses). Completely unstable.
Radiographic Features ( Fig. 5.11 )
- •
Teardrop fragment is major shear fragment from anteroinferior vertebral body.
- •
All ligaments are disrupted.
- •
Posterior subluxation of vertebral body
- •
Bilateral subluxated or dislocated facets
- •
Severe compromise of spinal canal secondary to subluxation of body and facets
- •
Not to be confused with:
Extension teardrop fracture (stable avulsive injury)
Burst fracture (stable comminuted fracture of centrum with variable neurologic involvement)

Clay-Shoveler’s Fracture ( Fig. 5.12 )
Oblique avulsive fracture of a lower spinous process, most commonly at C6–T1 levels (C7 > C6 > T1). Caused by powerful hyperflexion (shoveling).

Radiographic Features
- •
Fracture through spinous process, best seen on lateral view
- •
If C6–C7 is not demonstrated on lateral view, obtain swimmer’s view and/or CT.
- •
AP view: ghost sign (double-spinous process on C6–C7 caused by caudal displacement of the fractured tip of the spinous process)
Wedge Fracture
Compression fracture resulting from flexion. Most fractures are stable.
Radiographic Features
- •
Loss of height of anterior vertebral body
- •
Buckled anterior cortex
- •
Anterosuperior fracture of vertebral body
- •
Differentiate from burst fracture
Lack of vertical fracture component
Posterior cortex intact
Extension Teardrop Fracture ( Fig. 5.13 )
Avulsion fracture of anteroinferior corner of the axis resulting from hyperextension.

Radiographic Features
- •
Teardrop fragment: avulsion by the anterior longitudinal ligament
- •
Vertical height of fragment ≥ horizontal width
Do not confuse with limbus vertebra, which are a result of herniation of the nucleus pulposus through the endplate beneath the ring apophysis. Appear well corticated.
Bilateral Facet Dislocation (Unstable) ( Fig. 5.14 )
Results from extreme flexion of head and neck without axial compression.

Radiographic Features
- •
Complete anterior dislocation of the affected vertebral body by half or more of the vertebral body AP diameter
- •
Batwing or bowtie configuration of locked facets
- •
Disruption of posterior ligament complex, intervertebral disk, and anterior longitudinal ligament
Unilateral Facet Dislocation (Stable)
Results from simultaneous flexion and rotation.
Radiographic Features
- •
Anterior dislocation of vertebral body less than half the AP diameter of the vertebral body
- •
Evidence of discordant rotation above and below involved level
- •
Disrupted “shingles-on-a-roof” on oblique view
- •
Facet within intervertebral foramen on oblique view
- •
Disrupted posterior ligament complex
- •
Best demonstrated on lateral and oblique views
Anterior Subluxation (Hyperflexion Sprain) ( Fig. 5.15 )
Anterior subluxation occurs when the posterior ligament complex is disrupted. Radiographic diagnosis can be difficult because muscle spasm may cause similar findings. Initially stable. Delayed instability occurs in 20%–50%.

Radiographic Features
- •
Localized kyphotic angulation
- •
Widened interspinous/interlaminar distance (fanning)
- •
Posterior widening of disk space
- •
Subluxation at facet joints
- •
Anterior vertebral body may be displaced.
- •
In equivocal findings, voluntary flexion/extension views are helpful.
Hyperextension Fracture-Dislocation ( Fig. 5.16 )
Results from severe circular hyperextending force (e.g., impact on forehead). Characteristically results in anterior vertebral displacement, a finding more commonly seen in flexion injuries. Unstable.

Radiographic Features
- •
Mild anterior vertebral displacement
- •
Comminuted articular mass fracture
- •
Contralateral facet subluxation
- •
Disrupted anterior longitudinal ligament and partial posterior ligamentous disruption
Atlantooccipital Dissociation ( Fig. 5.17 )
Complex mechanism of injury. Complete dislocation is usually fatal.

Radiographic Features
- •
Prevertebral soft tissue swelling; a gap of more than 5 mm between the occipital condyles and the condylar surface of the atlas is highly suggestive of craniocervical injury.
- •
Wackenheim clivus line: a line drawn along the posterior aspect of the clivus toward the odontoid process. An abnormality is suspected when this line does not intersect or is tangential to the odontoid process.
- •
The traditional methods used to identify occipitoatlantal articulation injury included the power ratio (X/Y, see Fig. 5.17 ) and the “X” line of Lee. Each is dependent on identifying the opisthion and the spinolaminar line of C1. Anatomic variation and inconsistent visualization preclude consistent use of these methods.
- •
The current method uses the basion-axial interval (BAI) and is an easy and reliable method for assessing the occipitoatlantal relationship in patients of all ages. BAI is the distance between the basion and upward extension of the posterior axial line. Normally the BAI should not exceed 12 mm as determined on a lateral radiograph of the cervicocranium obtained at a target radiograph distance of 1 meter.
- •
The vertical basion-dens distance should also be <12 mm.
- •
Anterior dissociation is more common.
- •
Posterior dissociation (subluxation) can be very subtle, especially if partial.
In atlantoaxial fixation ( Fig. 5.18 ), the normal rotation of C1 on C2 cannot occur and the abnormal relationship between the atlas and the axis becomes fixed. Fielding and Hawkins have classified atlantoaxial rotatory subluxation into four categories:
- •
Type I, the most common type, demonstrates no displacement of C1.
- •
Type II demonstrates 3–5 mm of anterior displacement of C1 and is associated with abnormality of the transverse ligament.
- •
Type III demonstrates over 5 mm of anterior displacement of C1 on C2 and is associated with deficiency of the transverse and alar ligaments.
- •
Type IV, a rare entity, demonstrates C1 displacement posteriorly.
Occipital condyle fracture ( Fig. 5.19 )
- •
Often requires CT for diagnosis (coronal views). May involve the hypoglossal canal or jugular foramen.
- •
Unstable if avulsion of the alar ligament attachment site.

FIG. 5.19
- •
Longus colli muscle calcific tendinopathy ( Fig. 5.20 )
- •
Calcium hydroxyapatite deposition leads to an inflammatory response.
- •
Lateral C-spine view or CT shows amorphous calcification of the longus colli muscle tendons at the level C1–C2, often with small retropharyneal/prevertebral effusion.
- •
Do not mistake for retropharyngeal abscess or trauma.

FIG. 5.20
- •

Thoracic and Lumbar Fractures
General
Most fractures occur at thoracolumbar junction (90% at T11–L4). All patients should have CT except for patients with:
- •
Stable compression fractures
- •
Isolated spinous or transverse process fractures
- •
Spondylolysis
Radiographic Features
- •
Widened interpedicular distance
- •
Paraspinal hematoma
- •
Unstable fractures:
Compression fracture >50%
Widened interlaminar space
Disrupted posterior elements
All fracture-dislocations
Types of Fractures
Classified by mechanism or injury:
Compression or wedge fractures: anterior or lateral flexion
- •
Wedge-shaped deformity of vertebral body
- •
Decreased vertebral body height
- •
Burst fracture: axial compression
- •
Comminution of vertebral body
- •
Bone fragments in spinal canal are common.
- •
Chance fractures (lap seatbelt fracture, usually at L2 or L3 [ Fig. 5.21 ]): distraction from anterior hyperflexion across a restraining lap seatbelt
- •
Horizontal splitting of vertebra
- •
Horizontal disruption of intervertebral disk
- •
Rupture of ligaments
- •
More than 50% of patients have associated small bowel and colon injuries (obtain abdominal CT).

FIG. 5.21
- •
Fracture-dislocations: combined shearing and flexion forces
- •
Spinal cord injury is common. Minor fractures
- •
Transverse process fractures
- •
Spinous process fractures
- •
Pars interarticularis fractures
- •
Spondylolysis
Defect in the pars interarticularis (neck of the “Scottie dog”). Chronic stress fracture with nonunion. Typically in adolescents involved in sports. Most commonly at the L4 or L5 level.
Radiographic Features ( Fig. 5.22 )
- •
Separation of pars interarticularis
- •
Spondylolisthesis common in bilateral spondylolysis
- •
If patient looks to right, the left pars is visualized by X-ray.
- •
Oblique view is usually diagnostic.
- •
CT or single photon emission computed tomography (SPECT) may be helpful in confirming diagnosis.

Spondylolisthesis ( Fig. 5.23 )
Ventral subluxation of a vertebral body as a result of bilateral pars defects.
- •
Four grades based on degree of anterior displacement
- •
95% of spondylolisthesis occurs at L4–L5 and L5–S1.

Pseudospondylolisthesis ( Fig. 5.24 )
Secondary to degenerative disk disease and/or apophyseal degenerative joint disease (DJD). Use spinous process sign to differentiate from true spondylolisthesis. In true spondylolisthesis, the spinous process stepoff is above the level of vertebral slip; whereas in pseudospondylolisthesis, the stepoff is below the level of the slip.

Face
| General Category | Types | Need for CT |
|---|---|---|
| Orbital | Pure blow-out | Yes |
| Impure blow-out | Yes | |
| Blow-in | Yes | |
| Zygoma | Tripod fracture | Yes |
| Isolated zygomatic arch | No | |
| Nasal | Nondisplaced | No |
| Comminuted | Variable | |
| Nasal-orbital-ethmoid | Yes | |
| Septal fracture/dislocation | Yes | |
| Maxillary | Dentoalveolar | Yes |
| Sagittal | Yes | |
| Le Fort fractures | Yes | |
| Craniofacial (smash fractures) | Central craniofacial | Yes |
| Lateral craniofacial | Yes | |
| Frontal sinus | Yes | |
| Mandibular | Defined by site | Variable |
| Flail mandible | Variable |
Approach to Facial Fractures ( Fig. 5.25 )
Facial radiographs are rarely obtained for facial fractures. Thin-section CT with reformation is the preferred method of evaluation.
- 1.
Incidence: nasal fractures > zygoma > other fractures
- 2.
Facial series:
- •
Waters view: three lines of the “elephant” should be traceable.
Maxillary sinuses
Orbital floor and rim
Nasal septum zygoma
- •
Caldwell view
Orbital rim
Medial orbital wall
Sphenoid wings
- •
Lateral view
Paranasal sinuses
Pterygoid plates
- •
Towne view
Mandible
- •
Base view (C-spine must be cleared first)
Zygoma
Mandible
- •
- 3.
Facial series is not adequate for nasal fractures:
- •
Lateral (coned and soft tissue technique) views
- •
Waters view
- •
Occlusal view
- •
- 4.
Mandibular fractures require specific mandibular series:
- •
Lateral, Towne, bilateral oblique views
- •
- 5.
Direct signs of fracture:
- •
Cortical disruption, overlap, displacement
- •
- 6.
Indirect signs of fracture:
- •
Asymmetry
- •
Soft tissue swelling
- •
Sinus abnormality (opacification, polypoid mass, air-fluid levels)
- •
Orbital emphysema
- •

Orbital Fractures
Pure Orbital Blow-Out Fracture ( Fig. 5.26 )
Isolated fracture of the orbital floor or less commonly the medial wall; the orbital rim is intact. Mechanism: sudden increase in intraorbital pressure (e.g., baseball, fist).

Clinical Findings
- •
Diplopia on upward gaze (inferior rectus muscle entrapment)
- •
Enophthalmos (may be masked by edema)
Radiographic Features ( Figs. 5.27–5.28 )
- •
Displacement of bone fragments into maxillary sinus (trap door sign)
- •
Opacification of maxillary sinus (hematoma)
- •
Orbital emphysema
- •
Caldwell and Waters views best demonstrate fractures.
- •
Using CT, evaluate for muscle entrapment and orbital content herniation.


Impure Orbital Blow-Out Fracture
Associated with fracture of orbital rim and other facial fractures.
Orbital Blow-In Fracture
Impact to frontal bone causes blow-in of orbital roof. Associated with craniofacial fractures and frontal lobe contusion.
Nasal Fractures ( Fig. 5.29 )
Isolated nasal fractures are linear and transverse, result from a direct frontal impact, and usually occur in the lower one-third of the nasal bone. More complex fractures result from lateral blows or more severe trauma and are often accompanied by other facial fractures.

Radiographic Features
- •
Most fractures are transverse and are depressed or displaced.
- •
Dislocation of septal cartilage is diagnosed by occlusal view or CT.
- •
Anterior nasal spine fracture is best evaluated by occlusal view.
- •
Do not mistake sutures and nasociliary grooves for fractures.
Mandibular Fractures ( Fig. 5.30 )
The type of fracture depends on the site of impact. Most fractures are multiple and bilateral. The most common type of mandibular fracture is an ipsilateral fracture through the body of the mandible with a contralateral angle subcondylar fracture. Fractures typically occur in:
- •
Body (areas of weakness include mental or incisive foramen)
- •
Angle
- •
Subcondylar region (condylar neck)

Flail Mandible ( Fig. 5.31 A–B )
Symphysis fracture with bilateral subcondylar, angle, or ramus fracture. Tongue may prolapse and obstruct airway.


Zygoma Fractures ( Figs. 5.32–5.33 )
Best view to demonstrate zygoma fracture is the base view to demonstrate the “jug handle.”


Simple Arch Fractures
Simple fractures of the zygomatic arch are less common than complex fractures. Fracture lines occur most commonly:
- •
Anteriorly at temporal process
- •
In midportion near zygomaticotemporal suture
- •
Posterior and anterior to condylar eminence
Complex Arch Fractures (Tripod Fracture)
- •
Diastasis of zygomaticofrontal suture
- •
Posterior zygomatic arch fracture
- •
Fracture of inferior orbital rim and lateral maxillary wall
Maxillary Fractures ( Fig. 5.34 )
Dentoalveolar Fracture
Fracture of the alveolar process of maxilla secondary to direct blow. May present clinically as loose teeth; managed as open fracture.

Sagittal Maxillary Fracture
Usually occurs with other injuries such as Le Fort fracture.
Le Fort Fractures ( Figs. 5.35–5.36 )
Fracture patterns that occur along lines of weakness in the face. Mechanism: severe force to face as would occur in MVA. All Le Fort fractures involve the pterygoid plates of the sphenoid.


Le Fort Type I
This fracture produces a floating palate; fracture lines extend through:
- •
Nasal septum (vomer and septal cartilage)
- •
Medial, anterior, lateral, posterior walls of maxillary sinus
- •
Pterygoid plates of sphenoid
Le Fort Type II
This fracture produces a floating maxilla; zygomatic arches are not included in this fracture; fracture line extends through:
- •
Nasal bone and nasal septum
- •
Frontal process of maxilla
- •
Medial orbital wall (ethmoid, lacrimal, palatine)
- •
Floor of orbit (inferior orbital fissure and canal)
- •
Infraorbital rim
- •
Anterior, lateral, posterior wall of maxillary sinus
- •
Pterygoid plates of sphenoid
Le Fort Type III
This fracture separates face from cranial vault and produces a floating face; the fracture line extends through:
- •
Nasal bone and septum
- •
Frontal process of maxilla
- •
Medial wall of orbit (lacrimal, ethmoid, palatine)
- •
Infraorbital fissure
- •
Lateral wall of orbit
- •
Zygomaticofrontal suture
- •
Zygomatic arch
- •
Pterygoid plates of sphenoid
Shoulder
Fracture of the Clavicle ( Fig. 5.37 A–B )
Common in children. Medial fragment is displaced superiorly (pull from sternocleidomastoid). Lateral fragment is displaced inferior and medial (weight of arm, pull from pectoralis major). Sites of fracture include:
- •
Lateral third: 15%
- •
Middle third: 80%
- •
Medial third: 5%


Complications
- •
Laceration of vessels
- •
Nerve injuries
- •
Other associated fractures
Do not mistake rhomboid fossa (irregular concavity at the undersurface of the medial clavicle), a normal anatomic variant, for a fracture or lytic lesion.
Fracture of the Scapula
Uncommon. Causes: MVA, fall from height (direct impact injuries). Best radiographic view: transscapular view (Y-view), CT often helpful. Do not mistake ossification centers for fractures.
Fracture of Ribs
- •
Fractures usually occur in lower 10 ribs.
- •
First and second rib fractures can occur after high energy trauma to chest and may be associated with severe mediastinal and vascular injury.
- •
Flail chest occurs when three or more ribs fracture and each rib fractures in two places (segmental fractures). Commonly associated with pulmonary contusion, laceration, pneumothorax, hemothorax, etc.
Normal MRI Anatomy of Shoulder Joint ( Fig. 5.38 )
- •
The glenoid labrum is a fibrocartilaginous structure that attaches to the glenoid rim and is about 4 mm wide. Anteriorly, the glenoid labrum blends with the anterior band of the inferior glenohumeral ligament. Superiorly, it blends with the biceps tendon and the superior glenohumeral ligament. It is usually rounded or triangular on cross-sectional images.
- •
The tendon of the long head of the biceps muscle attaches to the anterosuperior aspect of the glenoid rim. From its site of attachment, the biceps tendon courses laterally and exits the glenohumeral joint through the intertubercular groove where it is secured by the transverse ligament. In Fig. 5.38 the biceps tendon attaches at the level of the superior labrum and glenoid. Note attachments to the (1) superior glenoid rim, (2) the posterior labrum, (3) the anterior labrum, and (4) the base of the coracoid process.
- •
The labral-bicipital complex is well visualized on transverse CT or MR arthrograms, as well as on coronal MR arthrograms and reconstructed images from coronal CT arthrograms.
- •
The glenohumeral ligaments play a role as shoulder stabilizers and consist of thickened bands of the joint capsule. The superior glenohumeral ligament is the most consistently identified capsular ligament. It can arise from the anterosuperior labrum, the attachment of the tendon of the long head of the biceps muscle, or the middle glenohumeral ligament.
- •
The middle glenohumeral ligament varies most in size and site of attachment to the glenoid. It typically has an oblique orientation from superomedial to inferolateral. It may attach to the superior portion of the anterior glenoid but more frequently attaches medially on the glenoid neck.
- •
The middle glenohumeral ligament may be absent or may appear thick and cord like (e.g., Buford complex).
- •
The inferior glenohumeral ligament is an important stabilizer of the anterior shoulder joint and consists of the axillary pouch and anterior and posterior bands. The anterior band inserts along the inferior two-thirds of the anterior glenoid labrum.

Shoulder Ultrasound (US)
Using a high-frequency linear transducer, US can be used to examine the rotator cuff, as well as biceps tendon, AC joint, and bursae.
- •
Normal rotator cuff is hyperechoic and fibrillary (important to insonate perpendicular to tendon plane to avoid anisotropy), is not compressible, and demonstrates an outer convex contour.
- •
Complete tear: nonvisualization of the tendon.
- •
Full-thickness tear: focal tendon defect/fluid; concave contour of bursal side of tendon; compressible tendon; cartilage interface sign (two parallel hyperechoic lines over humeral head)
- •
Partial-thickness tear: bursal side or articular side flattening with hypoechoic defect or heterogeneous echogenicity.
- •
Calcific hydroxyapatite deposits may manifest as dense or tiny calcifications with or without posterior acoustic shadowing. In calcific tendinitis, US may be used to guide fine needle aspiration and lavage.
Dislocations of the Glenohumeral Joint
Dislocation: separation of articular surface of glenoid fossa and humeral head that will not reduce spontaneously. Subluxation: transient incomplete separation that reduces spontaneously.
Anterior Dislocation ( Fig. 5.39 )
Most common type (95%) of dislocation. Usually caused by indirect force from abduction, external rotation, and extension.

Radiographic Features
- •
Humeral head lies inferior and medial to glenoid.
- •
Two lesions can occur as humeral head strikes the glenoid:
Hill-Sachs lesion (posterosuperior and lateral) of humeral head (best seen on AP view with internal rotation) and bony Bankart lesion (anteroinferior) of glenoid (may require CT)
- •
Bulbous distortion of the scapulohumeral arch (Moloney arch)
- •
Tear of the inferior glenohumeral ligament (IGHL) from its humeral attachment = humeral avulsion of the glenohumeral ligament (HAGL) lesion
- •
Associated labral tears ( Fig. 5.40 ):
Abduction and external rotation (ABER) view: stretches the IGHL, improves detection of anterior-inferior labral tears.
Bankart lesion: complete detachment of anterior inferior labrum and often IGHL or middle glenohumeral ligament (MGHL)
Perthes lesion: labral tear with periosteal stripping, labrum remains attached to periosteum
Anterior labral periosteal sleeve avulsion (ALPSA): basically a medially displaced Perthes lesion, labrum remains attached to periosteum
Glenolabral articular disruption (GLAD), superficial labral tear with glenoid cartilage injury. In contrast to the above labral tears, it is not associated with shoulder instability.

FIG. 5.40
Posterior Dislocation ( Fig. 5.41 )
Less common (5%); usually caused by direct or indirect force (fall on flexed and abducted arm). Associated with seizures or electrical shock (bilateral).
Lightbulb sign: appearance of the internally rotated humeral head on AP radiograph
Bennett lesion: rim of calcification along posterior glenoid, associated with posterior capsule avulsive injury (baseball pitchers or other overhead throwing athletes)

Radiographic Features
- •
Humeral head lies superior to glenoid.
- •
Trough sign: compression fracture of the anterior humeral surface, 15% (best seen on AP view with external rotation or axillary view)
- •
Sharp angle of the scapulohumeral arch (Moloney arch)
- •
Posterior displacement is best seen on axillary view.
- •
40-degree posterior oblique (Grashey view) may be needed: loss of glenohumeral space is diagnostic.
- •
Fixed in internal rotation
Inferior Dislocation
Also called luxatio erecta: the humeral head is located below the glenoid and the shaft of the humerus is fixed in extreme abduction. Complications of luxatio erecta include injuries to the brachial plexus and axillary artery.
Pseudodislocation of Glenohumeral Joint
Inferior and lateral displacement of humeral head because of hemarthrosis that often occurs in fractures of humeral head or neck. Not a true inferior dislocation.
Rotator Cuff Tear ( Figs. 5.42–5.43 )
The rotator cuff (inserts into anatomic neck and tuberosities of humerus) consists of four muscles. Mnemonic: SITS :
- •
S upraspinatus
- •
I nfraspinatus
- •
T eres minor
- •
S ubscapularis


Causes
- •
Degeneration
- •
Trauma
- •
Impingement
Radiographic Features
- •
Narrowing of acromiohumeral space to <6 mm (chronic rupture)
- •
Eroded inferior aspect of acromion (chronic rupture)
- •
Flattening and atrophy of the greater tuberosity of the humeral head (chronic rupture)
Acromial undersurface contour, Bigliani classification (assessed on sagittal oblique MR, type 3 strongly associated with rotator cuff impingement) ( Fig. 5.44 ):
- •
Type 1: flat
- •
Type 2: concave, without subacromial space narrowing
- •
Type 3: acute inferior downslope (hooked) with narrowing.
- •
Type 4: convex

FIG. 5.44
- •
- •
Arthrogram
Opacification of subacromial-subdeltoid bursa
Contrast may leak into the cuff in partial tears
- •
MRI features:
MR arthrography is most accurate diagnostic study
MR can distinguish full thickness (perforating tear, part of the tendon is intact) from complete (complete tendon interruption) tears.
Full-thickness tears are often associated with fluid in the subacromial/subdeltoid bursa.
Partial-thickness tears may be articular surface, bursal surface, or intrasubstance tears.
High-grade partial thickness tears >50%
Tendon retraction should be reported because retraction >3–4 cm reduces potential for surgical repair.
Fatty atrophy of a rotator cuff muscle indicates chronic tear.
Medial dislocation/subluxation of the biceps from the intertubercular groove indicates subscapularis tear
Labral Tears
- •
Normal labral variants:
Sublabral foramen between one and three o’clock
Buford complex: absent labrum from one to three o’clock, with thickened medial glenohumeral ligament
Sublabral sulcus in superior labrum
- •
Anterior-to-posterior lesions of the superior labrum (superior labral tear from anterior to posterior [SLAP] lesions)
SLAP tears are usually oriented from superior-lateral to inferior-medial
Type I: fraying or tear of the superior labrum
Type II: detachment of the labral-bicipital complex from the superior glenoid
Type III: bucket-handle tear of the superior labrum
Type IV: bucket-handle tear with extension into the biceps tendon
Muscle Atrophy
- •
Supraspinatus/infraspinatus: suprascapular nerve impingement in the suprascapular notch (e.g., by a paralabral cyst caused by a labral tear)
- •
Parsonage-Turner syndrome: acute brachial neuritis. Early edema and thickening of supraspinatus and infraspinatus; later, atrophy
- •
Infraspinatus: suprascapular nerve impingement after branch to supraspinatus in the spinoglenoid notch
- •
Teres minor (quadrilateral space syndrome): axillary nerve impingement in the quadrilateral space (bounded by teres minor superiorly, teres major inferiorly, humerus laterally, long head of triceps medially) secondary to fibrous band, fracture, mass lesion, etc.
Adhesive Capsulitis (Frozen Shoulder)
Pain, stiffness, and limited range of motion from posttraumatic adhesive inflammation of the joint capsule.
Radiographic Features
- •
Decreased size of joint capsule
- •
Obliteration of axillary and subscapular recesses
- •
Disuse osteoporosis
- •
Arthrogram if persistent
AC Separation ( Fig. 5.45 )
Most commonly results from athletic injury to AC joint
- •
Direct blow to AC joint (e.g., football)
- •
Severe arm traction
- •
Fall on hand or elbow with arm flexed 90 degrees
- •

Radiographic Features
Technique
- •
AP view with 15 degree cephalad angulation is the preferred view for diagnosis.
- •
May need opposite shoulder for comparison
- •
May need stress views (2- to 10-kg weights)
- •
Normal
- •
AC distance ≤8 mm
- •
Coracoclavicular distance ≤13 mm
- •
Inferior margin of clavicle lines up with inferior acromion.
- •
AC joint injury
- •
Downward displacement of scapula/extremity
- •
Downward displacement and AC separation worsen with stress weights.
- •
AC widening = disrupted AC ligament
- •
Craniocaudad (CC) widening because of disrupted AC ligament
- •
Six grade classifications (Rockwood):
- •
Grade I (mild sprain): normal radiograph
- •
Grade II (moderate sprain): increased AC distance; normal CC distance
- •
Grade III (severe sprain): increased AC and CC distance
- •
Grade IV: total dislocation; clavicle displaced superoposteriorly into the trapezius
- •
Grade V: total dislocation; clavicle displaced superiorly into neck
- •
Grade VI: total dislocation; clavicle displaced interiorly to subacromial or subcoracoid position
- •
Sternoclavicular Joint Injury ( Fig. 5.46 )
Most injuries of the sternoclavicular joint are dislocations resulting from a direct forceful impact. Although anterior dislocations are more common, posterior dislocations are more serious because the great vessels or trachea may be injured.

Radiographic Features
- •
Superior displacement of clavicle
- •
Many injuries occur as Salter fractures of medial clavicular epiphysis.
- •
CT is the examination of choice: thin section with coronal reformation.
- •
Angled AP plain radiograph (serendipity view) is not as helpful.
Arm
Fractures of Proximal Humerus
These fractures are common in osteoporotic older adult patients secondary to a fall on outstretched hand. 85% are nondisplaced; 4-segment Neer classification aids in treatment and prognosis.
Four-Segment Neer Classification ( Fig. 5.47 )
Based on number and type of displaced segments. 4 segments: anatomic neck, surgical neck, greater tuberosity, lesser tuberosity. Displacement defined as (1) >1 cm separation of fragments or (2) >45-degree angulation.
- •
1-part: no displacement (regardless of comminution); treated with sling
- •
2-part: displacement of 1 segment; closed reduction
- •
3-part: displacement of 2 segments, 1 tuberosity remains in continuity with the head; closed reduction
- •
4-part: displacement of 3 segments; open reduction and internal fixation or humeral head replacement
- •
2-, 3-, and 4-part fractures may have anterior or posterior dislocation.

Radiographic Features
- •
Fracture lines according to Neer classification
- •
Pseudosubluxation: inferior displacement of humeral head because of hemarthrosis
- •
Subacromial fat-fluid level: lipohemarthrosis
- •
Transthoracic or transscapular views useful to accurately determine angulation
Fractures of Distal Humerus ( Figs. 5.48–5.49 )
Classification
Supracondylar-extraarticular fracture (three types)
- •
Type I: nondisplaced
- •
Type II: displaced with posterior cortical continuity
- •
Type III: totally displaced
- •
Transcondylar-intraarticular fracture
Intercondylar (bicondylar)-intraarticular fracture (four types)
- •
Type I: nondisplaced
- •
Type II: displaced
- •
Type III: displaced and rotated
- •
Type IV: displaced and rotated and comminuted
- •


Complications
- •
Volkmann ischemic contracture (usually secondary to supracondylar fracture)
- •
Malunion (results in “cubitus varus” deformity)
Radial Head Fractures
Common fracture that results from a fall on outstretched hand.
Treatment
- •
No displacement: splint, cast
- •
>3-mm displacement on lateral view: open reduction and internal fixation (ORIF)
- •
Comminuted: excision of radial head
Radiographic Features ( Fig. 5.50 )
- •
Positive fat pad sign
Anterior fat pad has the appearance of a sail (sail sign).
A positive posterior fat pad is a good indicator of a fracture that is not normally seen.
- •
Fracture line may be difficult to see on standard projections. If in doubt, obtain radial head view, oblique views, or tomograms.

Ulnar Fractures
Isolated ulnar fractures are uncommon. Most fractures of the ulna also involve the radius (see below).
Olecranon Fracture
Result from direct fall on flexed elbow. Treated conservatively if nondisplaced. ORIF if displaced (by pull of triceps). Best view: lateral.
Coronoid Fracture
Usually in association with posterior elbow dislocations. Best view: radial head or oblique views.
Elbow Dislocations
Different types of dislocations are defined by the relation of radius/ulna to distal humerus. Posterior dislocations of both the radius and ulna are the most common type (90%). Often associated with coronoid process or radial head fractures. Complication: myositis ossificans. Three types include:
- •
Ulna and radius dislocation (most common)
- •
Ulna dislocation only
- •
Radial dislocation only (rare in adults)
Combined Radius-Ulna Fractures and Dislocations
Most (60%) forearm fractures involve both the radius and ulna.
Monteggia Fracture-Dislocation
Ulnar shaft fracture and radial head dislocation
Galeazzi Fracture-Dislocation
Distal radial shaft fracture and distal radioulnar dislocation
Essex-Lopresti Fracture-Dislocation
Comminuted radial head fracture and distal radioulnar subluxation/dislocation
Colles Fracture ( Fig. 5.51 )
Mechanism of injury: fall on the outstretched hand with the forearm pronated in dorsiflexion. Most common injury to distal forearm, especially in osteoporotic females.

Radiographic Features
- •
Extraarticular fracture (in contradistinction to Barton fracture)
- •
Distal radius is dorsally displaced/angulated.
- •
Ulnar styloid fracture, 50%
- •
Foreshortening of radius
- •
Impaction
Complications
- •
Median, ulnar nerve injury
- •
Posttraumatic radiocarpal arthritis
Other Radial Fractures ( Figs. 5.52–5.53 )
Barton Fracture
Intraarticular fracture of the dorsal margin of the distal radius. The carpus usually follows the distal fragment. Unstable fracture requiring ORIF and/or external fixation.


Smith Fracture
- •
Same as a Colles fracture except there is volar displacement and angulation of the distal fragment
- •
Three types
Type 1: horizontal fracture line
Type 2: oblique fracture line
Type 3: intraarticular oblique fracture = reverse Barton fracture
Reverse Barton Fracture (see Fig. 5.53 )
Intraarticular fracture of the volar aspect of the articular surface.

Chauffeur’s (or Hutchinson) Fracture ( Fig. 5.54 )
Fracture of the styloid process. Either by direct blow to back of wrist (hand crank of old cars started by hand) or forced dorsiflexion and abduction. Often associated with scapholunate disassociation and ulnar styloid process fracture.
Carpal Instability
Most commonly because of ligamentous injury of the proximal carpal row (trauma or arthritis). Best diagnosed by stress fluoroscopy and/or plain radiograph evaluation of the scapholunate and capitolunate relationships.
Elbow MRI Pearls
- •
Ulnar collateral ligament (UCL)
Three components: anterior (most important), posterior, and transverse bands
UCL tear = baseball pitcher injury. Anterior band attaches to sublime tubercle of medial epicondyle and lies deep to common flexor tendon of elbow. Posterior band attaches to lateral aspect of ulna at supinator crest. MRI: T1 globular signal, increased T2 signal.
- •
Radial collateral ligament complex
Four components: annular (torn with elbow dislocation), radial collateral, lateral ulnar collateral ligament (LUCL, most important), and accessory collateral ligaments
- •
Common extensor tendon originates from lateral epicondyle (repetitive varus stress leads to lateral epicondylitis or tennis elbow, often associated with LUCL injury)
- •
Common flexor tendon originates from medial epicondyle (repetitive valgus stress leads to medial epicondylitis or golfer’s elbow)
- •
Avascular necrosis (AVN) of capitellum: Panner disease, occurs in boys 7–12 years of age before complete capitellar ossification.
- •
Osteochondral defect (OCD) of capitellum: caused by repetitive valgus stress in young competitive athletes (12–16 years), most often involves anterior capitellum (do not mistake for normal “pseudodefect” that is caused by sharp angulation of posterior capitellum)
Nerve Entrapment Syndromes
- •
Ulnar nerve in cubital tunnel most commonly affected
Cubital tunnel floor = posterior and transverse bands of UCL
Roof = arcuate ligament. Replaced with anconeus epitrochlearis muscle in 10%–20%, which causes ulnar nerve compression. Cubital tunnel narrows during elbow flexion, ulnar nerve compression common in overhead-throwing athletes.
- •
Radial nerve: injured by humeral shaft fracture. Other causes: supinator syndrome.
- •
Median nerve
Avian (supracondylar) spur ( Fig. 5.55 ): present in 1%, located at anteromedial humerus around 5 cm from medial epicondyle

FIG. 5.55
Ligament of Struthers (present in 3%) connects avian spur to medial epicondyle forming supracondylar canal, which contains median nerve and brachial artery.
Pronator syndrome: compression between superficial and deep heads of pronator teres muscle.
Wrist/Hand
Wrist Anatomy ( Fig. 5.56 )
- •
Lunate
- •
Scaphoid
- •
Trapezium
- •
Trapezoid
- •
Capitate
- •
Hamate
- •
Triquetrum
- •
Pisiform

Lines of Articulations ( Fig. 5.57 )
Ulnar Variance
- •
Neutral ulnar variance (normal) 80% load by radius, 20% by ulna
- •
Negative ulnar variance (abnormal). Associated with Kienböck disease
- •
Positive ulnar variance (abnormal). Associated with:
Scapholunate instability
Ulnar impaction syndrome
Triangular fibrocartilage tear
Previous radial head excision
Aging

Standard radiographic assessment to quantify deformities associated with distal radius fractures should also consist of three radiographic measurements, which correlate with patient outcome:
- •
Radial length (radial height): on posteroanterior (PA) view, distance between line perpendicular to the long axis of the radius passing through the distal tip of the sigmoid notch at the distal ulnar articular surface of the radius and a second line at the distal tip of the radial styloid. This measurement is normally 10–13 mm. A shortening of >3 mm is usually symptomatic and leads to positive ulnar variance.
- •
Radial inclination (radial angle): on PA view, angle between line connecting the radial styloid tip and the ulnar aspect of the distal radius and a second line perpendicular to the longitudinal axis of the radius. The normal radial inclination ranges between 21 and 25 degrees. Loss of radial inclination increases load across the lunate.
- •
Volar tilt of the distal radius (palmar tilt): on lateral view, the angle between a line along the distal radial articular surface and the line perpendicular to the longitudinal axis of the radius at the joint margin. The normal volar tilt averages 11 degrees and has a range of 2 to 20 degrees. Dorsal intercalated segment instability (DISI) (see later) may result from an angle >25 degrees.
Scaphoid Fracture
Most common fracture of carpus. Mechanism: fall on outstretched hand in young adults. Locations:
- •
Waist, 70%
- •
Proximal pole, 20%
- •
Distal pole, 10%
Blood supply to the proximal pole enters at the waist; therefore the proximal pole is at high risk for nonunion and osteonecrosis.
Radiographic Features
- •
Fracture may be difficult to detect on plain radiograph.
- •
Scaphoid views (PA view in ulnar deviation) may be useful to demonstrate fracture.
- •
Loss of navicular fat stripe on PA view.
- •
If a fracture is clinically suspected but not radiographically detected, use multidetector CT. In the absence of multidetector CT and high-quality reformations, thin-section CT may be performed along the coronal and sagittal axes of the scaphoid:
Coronal position is obtained by placing the patient prone, with elbow flexed 90 degrees and hand placed ulnar side down above the patient’s head; images are acquired parallel to the dorsum of the wrist. Alternatively, with the palm side down, the hand and wrist are elevated 30–45 degrees and images acquired parallel to the dorsal aspect of the scaphoid.
Long sagittal position can be obtained by placing wrist palm down with hand, wrist, and forearm at 45-degree angle to the long axis of the CT table. Anatomically, this alignment can be recognized by identifying the base of the thumb and the hard bone prominence on the middle portion of the distal radius (Lister tubercle).
- •
Bone scan: highly sensitive; increased uptake may represent fracture, and decreased uptake proximally may represent possible AVN. Does not offer anatomic detail or distinguish marrow edema/bone bruise from fracture.
- •
MRI: highly sensitive to fractures and allows imaging of planes along the long and short axes of the scaphoid
- •
Cast and repeat plain radiographs in 1 week.
Prognosis
- •
Waist fracture: 90% heal eventually; 10% nonunion or proximal AVN
- •
Proximal fracture: high incidence of nonunion or AVN
- •
Distal fracture: usually heals without complications
Fractures of Other Carpal Bones
Triquetrum
- •
Dorsal avulsion at attachment of radiocarpal ligament (most common type of fracture)
- •
Best seen on lateral view
Hamate
- •
Hook of hamate fracture: diagnosis requires tomography, carpal tunnel view, or CT
- •
Other fractures are usually part of complex fracture-dislocations.
Kienböck disease (lunatomalacia)
- •
AVN of lunate secondary to (usually trivial) trauma
- •
Associated with ulnar minus variant
- •
Acute lunate fractures are rare.
Stahl classification (radiographs):
- •
Stage 1: normal radiograph
- •
Stage 2: increased lunar radiodensity
- •
Stage 3: lunate collapse
- •
Stage 4: degenerative changes around lunate
Preiser disease (scaphomalacia)
- •
AVN of scaphoid secondary to (usually trivial) trauma without fracture, or drugs (e.g., steroids)
Type 1: complete, indicates poor outcome.
Type 2: partial, associated with better outcome.
Greater arc injury
- •
Greater arc injuries extend through radial styloid and scaphoid across hamate, capitate, triquetrum, and ulnar styloid.
- •
Lesser Arc Injury (Perilunate Injuries) ( Fig. 5.58 )
The continuum of perilunate injuries ranges from disassociation to dislocation. Mechanism: backward fall on extended hand. Each of the four successive stages progresses from radial to ulnar side with ligamentous injury around the lunate, and indicates increased carpal instability.

Scapholunate Dissociation (Stage 1) ( Fig. 5.59 )
- •
Rupture of scapholunate ligaments
- •
>3-mm gap between lunate and scaphoid (Terry-Thomas sign)
- •
Ring sign on PA view secondary to rotary subluxation of scaphoid

Perilunate Dislocation (Stage 2)
- •
Capitate dislocated dorsally, while the lunate maintains normal articulation with radius.
- •
Disruption of the capitolunate joint (often the radiocapitate ligament)
- •
May be accompanied by transscaphoid fracture, triquetrum fracture, capitate fracture, and radial styloid process fracture
Midcarpal Dislocation (Stage 3)
- •
Rupture of triquetrolunate ligament (or triquetrum fracture)
- •
Capitate and carpus are dislocated dorsally.
Lunate Dislocation (Stage 4)
- •
Lunate dislocates volarly.
- •
Disruption of the dorsal radiolunate ligament.
- •
Capitate appears aligned with the radius.
Carpal Instability ( Figs. 5.60–5.61 )
Most commonly caused by ligamentous injury of the proximal carpal row (trauma or arthritis). Best diagnosed by stress fluoroscopy and/or plain radiograph evaluation of the scapholunate and capitolunate relationships.


Scapholunate Dissociation
- •
Scapholunate angle >60 degrees
Volar Intercalated Segment Instability (VISI)
- •
Increased capitolunate angle
- •
Volar tilt of lunate
- •
Scapholunate angle sometimes decreased
- •
Much less common than DISI
Dorsal Intercalated Segment Instability
- •
Increased scapholunate and capitolunate angles
- •
Dorsal tilt of lunate
Scapholunate Advanced Collapse (SLAC)
Specific pattern of OA associated with chronic scapholunate dissociation and chronic scaphoid nonunion. Calcium pyrophosphate dihydrate (CPPD) is the most common cause.
- •
Radial-scaphoid joint is initially involved, followed by degeneration in the unstable lunatocapitate joint as capitate subluxates dorsally on lunate.
- •
Radioscaphoid joint is first to be involved; capitolunate and scaphotrapeziotrapezoid (STT) joints follow.
- •
Capitate migrates proximally into space created by scapholunate dissociation.
- •
Radiolunate joint is spared.
- •
In end-stage SLAC, the midcarpal joint collapses under compression, and the lunate assumes an extended or dorsiflexed position DISI.
CT of the Wrist
Multidetector CT has revolutionized evaluation of the wrist. Special patient positions are no longer necessary because high-quality reformatted images can be obtained along any plane from a multidetector CT dataset. However, for historical purposes, dedicated CT of the distal radius, ulna, and carpus can also be performed in several planes.
- •
CT in the transverse plane has been used to evaluate the distal radioulnar joint and the carpal bones or to further assess a longitudinal fracture. The coronal plane provides an image similar to the standard PA radiograph but will provide better soft tissue and bone detail than will a routine radiograph.
- •
Coronal CT also demonstrates the radiocarpal joint well.
- •
In general, 2-mm thick sections at 2-mm intervals will be satisfactory to show the anatomic detail of distal radius and ulnar fractures along articular surfaces. When evaluating carpal bone fractures and displacements, it is sometimes of value to add 2-mm thick sections at 1-mm intervals in one plane for more anatomic detail, as for a scaphoid fracture.
Evaluation of Distal Radial Fractures ( Fig. 5.62 )
Fernandez and Jupiter, or mechanistic, classification system for distal radial fractures. This classification system closely mirrors prognosis. Fracture forces and comminution progressively increase from type I to type V:
- •
Type I: bending fractures; include metaphyseal Colles and Smith fractures. These are caused by tensile volar or dorsal loading, respectively, with subsequent comminution of the opposite cortex.
- •
Type II: shear fractures of the joint surface; includes volar and dorsal Barton injuries.
- •
Type III: compression fractures of the articular surface; includes die-punch fractures.
- •
Type IV: avulsion fractures and associated with radiocarpal fracture-dislocations; includes radial and ulnar styloid injuries.
- •
Type V: high-velocity injuries with comminution and often with bone loss; related to a complex interaction of multiple forces.

Hand Anatomy ( Fig. 5.63 )
- •
Metacarpals
- •
Phalanges: distal, medial, proximal
- •
Joints: distal interphalangeal (DIP), proximal interphalangeal (PIP), metacarpophalangeal (MCP)

First Metacarpal Fractures ( Fig. 5.64 )
Bennett and Rolando fractures are intraarticular MCP fracture-dislocations of the thumb. These fractures must be distinguished from extraarticular fractures located distal to the carpometacarpal (CMC) joint because the former may require open reduction.

Bennett Fracture
- •
Dorsal and radial dislocation (force from abductor pollicis longus)
- •
Small fragment maintains articulation with trapezium.
Rolando Fracture
- •
Comminuted Bennett fracture; the fracture line may have a Y, V, or T configuration.
Boxer’s Fracture ( Fig. 5.65 )
Fracture of the MCP neck (most commonly fifth MCP) with volar angulation and often external rotation of the distal fragment. Simple fractures are reduced externally, whereas volar comminution usually requires ORIF.

Gamekeeper’s Thumb (Skier’s Thumb) ( Fig. 5.66 )
Results from disruption of UCL. Often associated with a fracture of the base of the proximal phalanx. Common injury in downhill skiing (thumb gets hung up in ski pole). Stress views are required if no fracture is identified on routine plain radiographs but is clinically suspected.

Stener Lesion
Occurs in a subset of patients with gamekeeper’s thumb, when the UCL is completely torn and displaced superficial and proximal to the adductor pollicis aponeurosis, preventing the UCL from returning to its normal position. Detect with US or MR (yo-yo sign). Surgical lesion.
Phalangeal Avulsion Injuries ( Fig. 5.67 )
Results from forceful pull at tendinous and ligamentous insertions.

Baseball (Mallet) Finger
- •
Avulsion of extensor mechanism
- •
DIP flexion with or without avulsion fragment
Boutonnière (Buttonhole) Finger
- •
Avulsion of middle extensor slip at base of middle phalanx
- •
PIP flexion and DIP extension with or without avulsion fragment
Avulsion of Flexor Digitorum Profundus
- •
Avulsion at volar distal phalanx
- •
DIP cannot be flexed.
- •
Fragment may retract to PIP joint.
Volar Plate Fracture
- •
Avulsion at base of middle phalanx
- •
PIP hyperextension
- •
Nerve entrapment syndromes:
- •
Carpal tunnel syndrome: most common nerve entrapment in the body, median nerve is compressed in the carpal tunnel. On US and MRI, enlargement of the median nerve >2 mm 2 is seen in the carpal tunnel compared with at the level of the pronator quadratus. Contrast enhancement may be seen on MRI.
- •
Guyon canal syndrome: rare, compression of ulnar nerve by space-occupying lesion in canal. Other causes: extrinsic compression (cyclist’s arm), or thrombosis/aneurysm of superficial palmar branch of ulnar artery (hypothenar hammar syndrome)
- •
Lower Extremity
Hip Anatomy ( Figs. 5.68 – 5.69 )
Acetabular lines and anatomy:
- •
Anterior column includes anterior aspect of the iliac wing, pelvic brim, superior pubic ramus, anterior wall of acetabulum, and teardrop. The column marker on plain radiographs are the iliopubic (iliopectineal line) and pelvic brim.
- •
Posterior column consists of posterior ilium, posterior wall of acetabulum, ischium, medial acetabular wall (quadrilateral plate). The marker on plain radiographs is the ilioischial line: posterior portion of quadrilateral plate of iliac bone.
- •
Teardrop: medial acetabular wall + acetabular notch + anterior portion of quadrilateral plate
- •
Roof of acetabulum
- •
Anterior rim of acetabulum
- •
Posterior rim of acetabulum


Pelvic Fractures ( Fig. 5.70 A–B )
Classification
Stable fractures (single break of pelvic ring or peripheral fractures); more common
Avulsion fractures
- •
Anterior superior iliac spine: sartorius avulsion
- •
Anterior inferior iliac spine: rectus femoris avulsion
- •
Ischial tuberosity: hamstring avulsion
- •
Pubis: adductor avulsion
- •
Other fractures
- •
Duverney fracture of iliac wing
- •
Sacral fractures
- •
Fracture of ischiopubic rami: unilateral or bilateral
- •
Wide-swept pelvis: external rotation (anterior compression) injury to one side and an internal rotation (lateral compression) injury to contralateral side
- •
Unstable fractures (pelvic ring interrupted in two places); less common. Significant risks of pelvic organ injury and hemorrhage. All unstable fractures require CT before fixation for more accurate evaluation; the extent of posterior ring disruption is often underestimated by plain radiograph.
- •
Malgaigne fracture: SI joint (or paraarticular fracture) and ipsilateral ischiopubic ramus fracture. Clinically evident by shortening of the lower extremity.
- •
Straddle: involves both obturator rings
- •
Bucket-handle: SI fracture and contralateral ischiopubic ramus fracture
- •
Dislocations
- •
Pelvic ring disruptions and arterial injury
Sources of pelvic hemorrhage include arteries, veins, and osseous structures.
Arterial bleeding is usually from internal iliac artery branches. Frequency in descending order: gluteal, internal pudendal, lateral sacral, and obturator arteries.
- •


Fracture of the Acetabulum ( Fig. 5.71 A–C )
Classification (Letournel)
- •
Fracture of the anterior (iliopubic) column
- •
Fracture of the posterior (ilioischial) column
- •
Transverse fracture involving both columns
- •
Complex fracture: T-shaped, stellate


Sacral Fractures ( Fig. 5.71 D–E )
- •
Transverse fracture: direct trauma
- •
Vertical fracture: part of complex pelvic fracture
- •
Stress fractures: usually juxtaarticular and vertical
- •
One useful classification is the Denis classification:
Zone I: lateral to foramina—50% of cases; 6% with neurologic deficit
Zone II: transforaminal—34% of cases; 28% with neurologic deficit
Zone III: central canal involvement—8% of cases; 57% with neurologic deficit
Soft Tissue Injury ( Fig. 5.72 )
| Origin | Insertion | Nerve | |
|---|---|---|---|
| Flexors (Anterior) | |||
| Iliopsoas | Vertebra/ilium | Lesser trochanter | Femoral, lumbar ventral rami |
| Rectus femoris | Anterior inferior iliac spine | Patellar ligament | Femoral |
| Vagh group | Femur | Patellar ligament | Femoral |
| Sartorius | Anterior superior iliac spine | Medial tibial head | Femoral |
| Pectineus (adducts) | Iliopectineal line | Lesser trochanter | Femoral (obturator occasionally) |
| Extensors (Posterior) | |||
| Adductors | Ischial tuberosity | Femur (adductor tubercle) | Obturator |
| Hamstrings | |||
| Semitendinosus | Ischial tuberosity | Anteromedial tibial shaft | Tibial |
| Semimembranosus | Ischial tuberosity | Posteromedial tibial condyle | Tibial |
| Long head biceps | Ischial tuberosity | Fibular head | Tibial |
| Gluteus | Ilium, sacrum, ligaments | Femur (gluteal tuberosity) | Gluteal |

Fractures of the Proximal Femur ( Figs. 5.73–5.74 )
Incidence: 200,000/year in the United States. Fracture incidence increases with age. In the older adult group, mortality is nearly 20%.


Classification
Intracapsular fracture involving femoral head or neck
- •
Capital: uncommon
- •
Subcapital: common
- •
Transcervical: uncommon
- •
Basicervical: uncommon
- •
Extracapsular fracture involving the trochanters
- •
Intertrochanteric
- •
Subtrochanteric
- •
Femoral Neck Fractures
Associated with postmenopausal osteoporosis. Patients often have distal radius and/or proximal humeral fractures.
- •
Garden classification: based on displacement of femoral head; this classification best predicts risk of AVN and nonunion ( Fig. 5.75 )

FIG. 5.75
- •
MRI or bone scan helpful if plain radiographs are equivocal
Treatment
- •
Bed rest: incomplete fractures
- •
Knowles pin
- •
Endoprosthesis if high risk of AVN or nonunion
Complications
- •
AVN (in 10%–30% of subcapital fractures) occurs secondary to disruption of femoral circumflex arteries.
- •
Nonunion: obliquity of fracture influences prognosis (steep fractures have higher incidence of nonunion).
Intertrochanteric Femoral Fractures
Less common than subcapital fractures. Associated with senile osteoporosis.
- •
Simple classification: 2-, 3-, 4-, or multipart fracture, depending on number of fragments and involvement of trochanters
- •
Posteromedial comminution is common
Treatment
- •
Internal fixation with dynamic compression screw
- •
Valgus osteotomy
Complications
- •
AVN is rare.
- •
Coxa vara deformity from failure of internal fixation
- •
Penetration of femoral head hardware as fragments collapse
- •
Arthritis
- •
Lesser trochanter avulsion fracture
Avulsion of iliopsoas in children and adolescents
In adults, isolated less trochanter fracture should raise suspicion for a pathologic fracture (metastatic disease)
Dislocation of the Hip Joint
Classification ( Fig. 5.76 )
Posterior dislocation, 90%
- •
Femoral head lateral and superior to the acetabulum
- •
Femur internally rotated, greater trochanter in profile and lesser trochanter obscured on AP view
- •
Posterior rim of acetabulum is usually fractured
- •
Sciatic nerve injury, 10%
- •
Anterior dislocation, 10%
- •
Femoral head displaced into the obturator, pubic, or iliac region
- •
Internal dislocation
- •
Always associated with acetabular fracture
- •
Femoral head protrudes into pelvic cavity
- •
Femoral stress fracture
- •
Medial femoral neck proximal to lesser trochanter, linear sclerosis or periosteal bone formation can be seen radiographically. MRI is more sensitive and should be obtained if clinical suspicion is high.
- •
Bisphosphonate therapy is associated with stress fractures of the lateral humeral shaft, look for linear sclerosis on radiographs.
- •
Femoroacetabular impingement ( Fig. 5.77 )
- •
Impingement of acetabular labrum and cartilage between femoral head-neck junction and acetabular rim
- •
Cam-type : more common, dysmorphic bulge/overgrowth at the anterolateral femoral head-neck junction
- •
Pincer-type: less common, excessively deep acetabulum, look for cross-over sign (anterior acetabular margin projects lateral to posterior acetabular margin)
- •
Associated with old developmental dysplasia of the hip (DDH) or Legg-calvé-perthes disease

FIG. 5.77
- •
Morel-Lavallée lesion
- •
Degloving injury commonly seen in the lateral proximal thigh and lower back
- •
Subcutaneous fat is detached from muscle fascia
- •
Potentially large, chronic, collections can develop
- •

Athletic Pubalgia
- •
Chronic groin pain in athletes
- •
On MRI, proximal adductor and/or distal rectus abdominis tears, pubic symphisitis/osteitis pubis, medial pubic bone stress injury, or fascia tears of transverse or oblique abdominal muscles, among other causes can be seen.
- •
Osteitis Condensans Ilii
- •
Dense sclerosis in the medial iliac bones adjacent to SI joints
- •
Typically in young multiparous women (postpartum laxity of pubic symphysis)
Fracture of the Distal Femur
Classification
Supracondylar
- •
Nondisplaced
- •
Displaced
- •
Impacted
- •
Comminute
- •
Condylar intercondylar
Fracture of the Proximal Tibia
Fender or bumper fracture: knee is struck by moving vehicle. Lateral (80%) plateau fracture is more common because most trauma results from valgus force; medial plateau fractures (10%); 10% combined medial and lateral fractures.
Classification (Müller) ( Fig. 5.78 )
- •
Type 1: split fracture of tibial condyle and proximal fibula (rare)
- •
Type 2: pure depression fracture of either plateau
- •
Type 3: combined types 1 and 2
- •
Type 4: comminuted fracture of both tibial condyles; lateral plateau is usually more severely damaged.

Radiographic Features
- •
Fractures of tibial plateau may not be obvious; plain radiographs often underestimate the true extent of fractures; therefore CT or tomography in AP and lateral projection is often necessary.
- •
Fat (marrow)-fluid (blood) interface sign (hemarthrosis) on cross-table lateral view
- •
Description of fractures:
Type of fracture: split, depression, etc.
Location: medial, lateral
Number of fragments
Displacement of fragments
Degree of depression
Complications
- •
Malunion (common)
- •
Secondary OA (common)
- •
Concomitant ligament and meniscus injuries (i.e., medial collateral ligament [MCL])
- •
Peroneal nerve injury
Tibial Stress Fracture
Classic runner’s fracture is most commonly in proximal tibia.
- •
Zone of sclerosis with periosteal reaction
- •
Cortical thickening in posteromedial aspect of proximal tibia
Fracture of the Patella
Classification (Hohl and Larson):
- •
Vertical fracture
- •
Transverse (most common)
- •
Comminuted
- •
Avulsed
- •
Differentiation of multipartite patella from fractured patella:
- •
Bipartite or multipartite patella is typically located at the superolateral margin of the patella.
- •
Individual bones of a bipartite or multipartite patella do not fit together as do the fragments of a patellar fracture.
- •
The edges of bipartite or multipartite patella are well corticated.
- •
Osteochondral and Chondral Fracture
Shearing, rotary, and tangential impaction forces may result in acute fracture of cartilage (chondral fracture) or cartilage and bone (osteochondral fracture).
Radiographic Features
- •
Chondral fracture requires arthrography or MRI for visualization.
- •
Osteochondral fracture may be seen by plain radiograph.
Osteochondritis Dissecans (Chronic Osteochondral Fracture)
Painful, usually unilateral, disease in children and young adults. Results from chronic trauma: a segment of articular cartilage and subchondral bone becomes partially or totally separated. Locations: lateral aspect of medial femoral condyle (75%), medial aspect of medial femoral condyle (10%), lateral aspect of lateral condyle (15%), anterior femoral condyle. Do not confuse osteochondritis dissecans with dorsal defect of patella, which is a benign subchondral lesion of unclear cause, appears as rounded focus of radiolucency with surrounding sclerotic margin at the superolateral aspect of the patella.
Radiographic Features
- •
Earliest finding: joint effusion
- •
Radiolucent line separating osteochondral body from condyle (advanced stage)
- •
Normal ossification irregularity of posterior condyle may mimic osteochondritis dissecans.
- •
Best evaluated by MRI
Patellar Dislocation
The patella normally sits in the trochlear sulcus of the distal femur. The mechanism of dislocation is usually an internal rotation of the femur on a fixed foot. Almost always lateral with disruption of medial retinaculum. Medial facet of patella impacts on anterior lateral femoral condyle.
Radiographic Features
- •
Plain radiographs can be unremarkable except for joint effusion.
- •
MRI is the imaging modality of choice and shows:
Hemarthrosis
Disruption or sprain of medial retinaculum
Lateral patellar tilt or subluxation
Bone contusions in lateral femoral condyle anteriorly and in medial facet of patella
Osteochondral injuries of patella
Associated injuries to ligaments and menisci in 30%
Patellar Tendinitis (Jumper’s Knee)
Overuse syndrome occurring in athletes involved in sports that require kicking, jumping, and running. These activities can place a tremendous stress on the patellofemoral joint, with eventual necrosis, fibrosis, and degeneration of patellar tendon leading to rupture.
- •
MRI is the imaging modality of choice.
- •
Enlarged proximal patellar tendon with areas of increased signal intensity on T1-weighted (T1W) and T2-weighted (T2W) images.
Meniscal Injury ( Fig. 5.79 )
The most commonly injured meniscus is the medial one. The lateral meniscus is less commonly injured because it has greater mobility. Injuries to the lateral meniscus are associated with discoid meniscus.

Types
- •
Vertical (longitudinal) tears; most commonly from acute trauma
- •
Horizontal tears (cleavage tears) in older patients: degenerative
- •
Oblique tears
- •
Bucket-handle: may become displaced or detached. There are characteristic signs by MRI: double posterior cruciate ligament (PCL) sign and flipped meniscus sign. The displaced fragment is typically seen within the intercondylar notch.
- •
Peripheral tear: meniscocapsular separation
- •
Truncated meniscus: resorbed or displaced fragment
MRI Grading of Tears ( Fig. 5.80 )
- •
Type 1: globular increased signal intensity, which does not communicate with articular surface. Pathology: mucinous, hyaline, or myxoid degeneration
- •
Type 2: linear increased signal intensity, which does not extend to articular surface. Pathology: collagen fragmentation with cleft formation
- •
Type 3: tapered apex of meniscus
- •
Type 4: blunted apex of meniscus
- •
Type 5: linear increased signal intensity, which extends to the articular surface. Pathology: tear
- •
Type 6: linear increased signal intensity, which extends to both articular surfaces
- •
Type 7: fragmented, comminuted meniscus

Pitfalls of Diagnosing Meniscal Tears by MRI ( Fig. 5.81 )
- •
Fibrillatory degeneration of the free concave edge of the meniscal surface is often missed by MRI because of volume averaging.
- •
Normal transverse ligament courses through Hoffa fat pad and may be mistaken for an anterior horn tear. The ligament connects the anterior horns of medial and lateral menisci.
- •
Postmeniscectomy meniscus may have linear signal extending to articular surface as a result of intrameniscal signal.
- •
Pseudotears
Lateral aspect of posterior horn of lateral meniscus (popliteus tendon); medial lateral meniscus (ligament)

Discoid Meniscus
Morphologically enlarged meniscus (normal variant). Clinically presents as clicking of knee on flexion and extension. Diagnosed by MRI if three or more sagittal images show bridging between anterior and posterior horns. Prone to tears; almost always lateral.
Meniscal Calcifications
Common finding in many diseases (CPPD, hydroxyapatite, hyperparathyroidism [HPT], hemochromatosis, Wilson disease, gout, collagen vascular disease, idiopathic). Meniscal calcification is usually not detectable by MRI.
Meniscal Cysts
Formed by insinuation of joint fluid through a meniscal tear into adjacent tissues; therefore meniscal cysts always occur with meniscal tears. Most common in lateral meniscus. Patient presents with knee pain and lateral joint swelling.
Cruciate Ligament Tears ( Fig. 5.82 )
The cruciate ligaments are intracapsular and extrasynovial. The anterior cruciate ligament (ACL) limits anterior translation of the tibia and hyperextension. The PCL limits anterior translation of the femur and hyperflexion. ACL tears are far more common than PCL tears and are often associated with other injuries.

Radiographic Features
- •
Plain radiographs may show avulsion fragment of intercondylar eminence.
- •
MRI is the study of choice for diagnosing ligamentous injury.
- •
PCL is larger than ACL and better seen by MRI.
- •
MRI is useful for the assessment of complications after ACL reconstruction, including the Cyclops lesion (focal fibrotic nodule in the intercondylar notch).
| Degree of Injury | Direct Signs | Indirect Signs | |
|---|---|---|---|
| Mild sprain | Ligament edema | T2W hyperintensity | |
| Moderate sprain | Partial tear | ACL edema/hemorrhage | Buckling of PCL |
| Some fibers intact | ACL angulation | ||
| Anterior tibial subluxation | |||
| Rupture | Complete tear | Wavy contour | Lateral bone bruise |
| No ACL identified | MCL injury | ||
| ACL discontinuity | Medial meniscal injury | ||
| Edema/hemorrhagic mass | |||
| Chronic injury | Old mild/moderate sprains | Thickened ACL | Anterior tibial subluxation |
| Thinned ACL | |||
| Abnormal proton density signal | |||
| No acute edema on T2W images |
Segond Fracture ( Fig. 5.83 )
Small avulsion fracture involving the superolateral surface of the proximal tibia. Frequently associated with tears of lateral capsular ligament, ACL, and menisci. Segond fracture is in the midcoronal plane and must be differentiated from less common iliotibial band (ITB) avulsion of Gerdy tubercle seen more anteriorly on the tibia. MRI should be performed in all cases of Segond fracture to evaluate associated ligamentous injury.

Reverse Segond Fracture
Similar to Segond fracture but the fragment is located on the medial surface of the proximal tibia. Represents avulsion of the deep capsular component of the MCL. Associated with tears of the PCL, avulsions of the PCL from the posterior tibial plateau, and tear of the medial meniscus. MRI should also be performed to evaluate associated injuries.
Collateral Ligaments
The MCL (injury common) is attached to the medial meniscus, so both are frequently injured together. The lateral collateral ligament (LCL) complex (injury less common) consists of the fibular collateral ligament, the biceps femoris tendon, and the ITB.
Radiographic Features ( Fig. 5.84 )
- •
MRI criteria of injury are similar to those used for ACL and PCL tears
- •
O’Donoghue triad (the “unhappy triad”) results from valgus stress with rotation:
ACL tear
MCL injury
Medial meniscal tear (lateral compartment bone bruise)
- •
Pelligrini-Steida lesion: curvilinear calcification or ossification at site of femoral attachment of MCL indicates old MCL injury.

Tendon Injury
Commonly occurs from acute trauma or overuse injury in athletes or degenerative tendinopathy in older adults.
Radiographic Features
Acute tendinitis
- •
Tendon enlargement
- •
Fluid in synovial sheath (in tenosynovitis)
- •
Abnormal MRI signal within tendon may indicate partial tear.
- •
Chronic tendinitis
- •
Tendon thinning or thickening
- •
Intratendon signal does not increase on T2W images.
- •
Knee Dislocation
- •
Posterior, 75%
- •
Anterior, 50%
- •
Serious vascular injury to popliteal vessels occurs in 35% and to peroneal vessels in 25%.
Avulsion Injury Sites
- •
ACL at tibial intercondylar eminence
- •
PCL at posterior tibia
- •
ITB at Gerdy tubercle
- •
LCL/biceps femoris at proximal fibula
- •
MCL at femoral or tibial condyles
- •
Patellar tendon at tibial tubercle (chronic avulsion injury in children/adolescents = Osgood-Schlatter disease)
Friction Syndromes at the Knee
- •
ITB friction syndrome:
Common cause of lateral knee pain in young runners/cyclists
ITB rubs against femoral epicondyle causing irritation and synovial proliferation, MRI demonstrates abnormal signal between these structures and/or superficial to ITB
- •
Posteromedial knee friction syndrome:
Medial knee pain, abnormal MR signal between posteromedial femoral condyle, sartorius and/or gracilis tendons.
Ankle
Ankle Anatomy ( Fig. 5.85 )