Introduction
The superficial location of many musculoskeletal structures makes them readily amenable to injection therapy and many unguided injections are carried out in the office or ward setting. Large superficial structures are easily targeted, although success will vary with the practitioner’s expertise. It is generally accepted that many of these unguided injections will miss their target, but, despite this, patients not infrequently report good responses. Good responses may be due to local diffusion (in a non-contained space even a small-volume injection will spread quite widely) or systemic absorption of the injected material. There is emerging evidence, however, that clinical outcome is improved by accurate injection, and image guidance, whether this is by X-ray fluoroscopy, CT ultrasound or MRI, plays an important role in ensuring that diagnostic and therapeutic injections reach their intended target. Accurate guidance of local anaesthetic into a presumed pain generator is an important part of the clinical workup in musculoskeletal practice, which cannot be replicated by systemic injection of therapeutic agents.
Guidance is important when the target is small, difficult to feel clinically or landmarks are difficult to define. Accurate localization is important when surgical decisions are based on the patient’s response to local anaesthetic, when more complex intervention is being considered or where patients have failed to respond to unguided therapy.
Setup
In most cases, a complex setup is not required and most injections can be carried out as an adjunct to the basic ultrasound examination. Syringes and needles that are found in most departments and wards are sufficient. Simple sterilization measures have kept the incidence of infection very low. The routine use of a sterile probe cover is a matter of personal preference or local policy.
More rigorous sterility is mandatory when an implanted joint is being injected, in the presence of infection, where significant bleeding is expected or when it is anticipated that the needle will lie very close to the probe and risk rubbing against it.

Treatment Rationale
Broadly speaking, abnormalities of soft tissue commonly encountered in musculoskeletal practice can be divided into two main groups: inflammatory lesions and injuries that are the consequence of overuse or misuse.

Corticosteroids and Their Side Effects
Corticosteroid Preparations
Corticosteroid preparations vary in their strength and efficacy. Some of these differences are due to solubility and composition, the latter related to chemical composition. The composition also results in different particle sizes, which in turn has an influence on side effects. Hydrocortisone is generally considered the weakest of the preparations in general use. Triamcinolone and methylprednisolone are intermediate in strength. The potency of dexamethasone and betamethasone is fivefold that of methylprednisolone or triamcinolone.
Steroid Flare
One of the most common complications occurring following steroid injection is steroid flare. This is an inflammatory type reaction that comes on relatively quickly after the injection and may last 2 to 3 days.
| The features of steroid flare are similar to infection; however, the relatively rapid onset occurring within hours usually differentiates these two conditions. |
Skin Changes
Patients also need to be warned of the possibility of subcutaneous fat atrophy or skin depigmentation, particularly dark-skinned individuals. This is more common with superficial injections. There is some weak evidence that triamcinolone is a particular culprit and it is therefore suggested that this agent is not used for superficial injections or injections where there is a risk of the injected material tracking back along the needle. The adverse effect is thought to be due to a cytotoxic effect of the corticosteroid combined with alterations of collagen and glycoaminoglycogen. Local vasoconstriction may have an additive effect. The patient complains of a palpable depression of the skin surface at the site of injection. Other local effects on skin include depigmentation and atrophy. The effect may not occur immediately and can resolve, albeit over several years.
Tendon Injury
It is well recognized that direct injection of corticosteroid into a tendon may precipitate tendon rupture. It is also suspected that injection around a damaged tendon carries a similar risk. This poses a particular challenge to ultrasound-guided injections for tenosynovitis, particularly those involving lower limb tendons. The sensitivity of modern ultrasound equipment is such that subtle abnormalities are frequently identified within the tendon in patients with predominant tenosynovitis. In such cases, it is becoming increasingly accepted that tendon sheath injections are not contraindicated, but the patient should be warned of the potential risks, should avoid heavy-impact exercise or exertion and in many cases the tendon should be immobilized in a cast or boot for several weeks to protect it.
Flushing
Facial flushing, facial redness and feelings of increased temperature are not uncommonly experienced. They tend to occur within hours of the injection and generally last for one day. It has been suggested that this is a histamine response and antihistamines may be helpful in alleviating what can sometimes be an unpleasant side effect.
Septic Arthritis
Allergic reactions to corticosteroid injections are rare but are occasionally encountered. The most significant complication is septic arthritis. Fortunately the incidence of this complication is rare. There have been various reports but it is probably less than 1/1000 injections. Symptoms of sepsis have been well described and tend to occur within several days and up to the second week following injection. This delayed onset helps to distinguish sepsis from postinjection steroid flair.
Hyperglycaemia
Corticosteroid injection may lead to hyperglycaemia and diabetics should be warned about potential changes in their blood sugar readings. This effect may last several days. Rarely ketoacidosis may be precipitated.
Local Anaesthetic Preparations
Duration of Action
Lidocaine has a rapid onset of action and a duration of action of approximately 2–4 hours. Bupivacaine has a slower onset of action of approximately 10 to 15 min but is said to have a longer duration of action, but it may be no more than 6–8 hours. The relatively short duration of action of lidocaine means that the diagnostic effect may be obscured by the pain and anxiety related to the procedure itself. As previously outlined, an important role of the local anaesthetic component of the injectate is to assist with diagnosis and confirm that the patient’s symptoms do indeed emanate from the structure being anaesthetized. A longer-acting agent has obvious advantages. It is important to ensure that the patient understands that they need to test their symptoms following the injection, particularly in the initial several hours.
A pain diary is a simple method of recording the response and should be kept for several weeks.
Chondrotoxicity
Concern has been raised regarding toxic effects of intraarticular injections on articular cartilage. These have predominantly focused on local anaesthetics, particularly bupivacaine, although corticosteroids have also been implicated in the past. It does appear that repeated corticosteroid injections can result in cartilage loss, although this occurs in a very small proportion of patients over a long period of time. In vitro tests of bupivacaine have demonstrated a cytotoxic effect on cartilage. Concern has been expressed over the use of this agent for intraarticular injections, although its use as an intraarticular infusion following joint surgery is a greater risk. Lidocaine has been shown to be less toxic, although its duration of action is less than bupivacaine and may therefore not be as useful an agent as a diagnostic test. A suggested compromise is to use isomers of bupivacaine, ropivicaine or chirocaine, which are said to be less toxic and have durations of action only slightly shorter than bupivacaine.
General Principles of Ultrasound-Guided Injection
Most ultrasound-guided procedures can be kept relatively comfortable for the majority of patients. Unfortunately some are intrinsically painful, but even in these careful attention to detail can help minimize the trauma. Patients do not like to see needles and it is important that they are not flaunted. This is particularly important for children, where even the use of the word ‘needle’ should be avoided. Communication between the sonologist and assistant can be limited to describing the colour of the needle required. Once everything is made ready, the procedure should be carried out as quickly and as efficiently as possible.
The patient should be in as comfortable a position as possible, preferably one where they do not have to observe the procedure. It is also important that the operator is comfortable and machine and couch heights should be adjusted as appropriate. It is probably better to have the side being injected closest to the operator so as not to have to stretch over the patient, though of course this cannot be avoided if both sides are being treated simultaneously. To begin, a preliminary examination is carried out and a mark is placed on the skin when the best puncture point and approach to the lesion is found. It is sometimes helpful to use the blunt end of a needle sheath to make the mark, as marking with a pen can be difficult in the presence of ultrasound gel. Alternatively two marks can be made at right angles to each other away from the injection point out of any skin gel. This is more appropriate for injection of larger structures. In addition, it is sometimes helpful to draw a line next to the mark, giving the initial direction of approach for the needle ( Fig. 29.3 ).
| Thought should be given to the choice of puncture point and needle track. In addition to the obvious desire to reach the target without transgressing important structures, particularly nerves, there is also an advantage in choosing a course that keeps the needle as parallel as possible to the ultrasound probe. |


Lidocaine is slightly acidic and may cause a stinging sensation that can be reduced by the addition of a small amount of sodium bicarbonate. If the target is very superficial, with experience, local anaesthetic is not required and can add to the discomfort of the procedure. If local anaesthetic is to be used, it is preferable to sterilize the skin and inject local anaesthetic before drawing up the other injection agents or preparing a sterile probe. This gives some time for the local anaesthetic to work before proceeding with the injection. A single puncture is recommended with local anaesthetic infiltrated using the same needle that will be used for the actual injection. Exceptions are where a large needle is to be used, such as for ganglion aspiration or in needle-phobic patients. In these cases the skin is anaesthetized with the smallest available needle.
It is important to have an agreed local policy for patients on anticoagulant therapy. For most superficial injections when small bore needles are being employed, stable international normalized ratio (INR) readings below 2.5 are often accepted. When larger needles are required, for biopsies or where the injection is in an area where occult bleeding could be problematic, alternative arrangements should be made. Generally this involves converting the patient to heparin and omitting a dose the evening before the procedure. Obviously the final decision depends on the patient’s overall medical condition and risks from stopping anticoagulation.
Needle Techniques
In most cases, needles that are in general use in the department suffice. Some manufacturers produce coated needles, which are undoubtedly easier to see; however, for most procedures the additional expense is debatable. For most procedures a 23 G needle is ample and it is useful to have a selection of lengths available. There are two approaches used to position needles under ultrasound guidance, depending on the size and depth of the target. For deeper lesions, small targets and biopsies, amongst others, the needle is kept in view at all times. This is the in-view approach. For superficial joint injections an out-of-view approach may be easier.
‘In View’ Method
For many procedures it is desirable to keep the needle in view at all times until it safely reaches its target. For an in view approach, the needle is aligned with the long axis of the probe. The skin is punctured in the middle of one of the short sides of the probe at an appropriate distance from it depending on the size and depth of the target. As the needle is advanced, it quickly comes into view on one side of the screen. The needle tip specifically must be identified and tracked until it reaches its intended target. The shape of the bevel must be visible to ensure that the tip and not another part of the needle is being followed. To protect the target, the bevel is kept upwards until the target is reached. Once within the target, the bevel is rotated to better position the opening of the needle within the target joint, bursa or sheath.
During the procedure, the probe should remain on the target with the tip of the needle kept in view. If visualization of the needle tip is lost, it should not be advanced further until it has been relocated.
‘Out of View’ Method
For superficial small joints, there is not necessarily a need to track the needle from skin to target. Instead, the probe is placed in the sagittal plane over the target joint such that its midpoint is directly over the joint or its most distended or effused part. The skin is punctured in the midpoint of the long side of the probe (as opposed to the short side for an in view approach), and directed deep and towards the probe. If the initial position of the probe is chosen carefully enough and no proximal or distal angulation is applied to the needle, its tip should suddenly appear in the ultrasound image within the joint. More recently, manufacturers have been placing marks on the midpoint of the probes to facilitate this. Short footprint probes also tend to be thinner, allowing the skin to be punctured closer to the target joint.
Soft Tissue Biopsy
Important Principles
A detailed discussion on the diagnosis of soft tissue masses will be found in Chapter 31 . The principal role of the ultrasound of masses is to confirm the presence of a significant mass, to distinguish fluid from solid lesions, to identify tissue and compartment planes and to guide biopsy. Biopsy of musculoskeletal soft tissue masses follows similar principles to the biopsy of other organs; however, there are several aspects that are important when sarcoma is suspected.
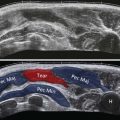
The prognosis of sarcoma is dependent on its local extent and in particular whether it is confined to a single anatomical compartment. It is therefore imperative that the biopsy approach to a soft tissue lesion takes account of the compartment within which it is located and ensures that the track does not transgress adjacent spaces.
A particular advantage of using ultrasound guidance to biopsy the soft tissues masses is that the internal structure of the lesion can be assessed ( Fig. 29.5 ). The preliminary examination should note and avoid necrotic, fibrous or other atypical areas that may result in false-negative biopsy.