Fig. 6.1
Scheme of the curve of enhancement in the arterial district: description of factors that influenced the different steps
Of these factors, the only one that can be modified by the radiologist is the iodine rate per second, which depends on the injection flow and the iodine concentration of the contrast media.
For example, to obtain the correct iodine rate per second inside the arterial vessels (1.8 g/s–2.0 g/s), we could use a 370-mg iodine contrast at 5 ml/s (5 × 0.37 = 1.85 g I/s) or a 400-mg I at 4.5 ml/s (4.6 × 0.4 = 1.84 g I/s); by moving these two parameters we can obtain the same arterial enhancement with different contrast media concentrations.
CT angiography for epi-aortic vessels in trauma cases constitutes a pre-contrast phase, mandatory to delineate recent bleeding, an arterial phase, and a venous phase for late venous bleeding. A pre-contrast brain scan is mandatory to better delineate the presence of parenchymatous hemorrhage.
The scout view has to delineate the aortic arch where the bolus tracking should be positioned. Minimum delay from the peak of 100 HU inside the aortic arch is preferred.
The scan could be managed in a caudo-cranial direction from the aortic arch to the brain, and next a cranio-caudal full-body scan in late arterial phase must be performed to evaluate the parenchymatous organs. The pitch parameter should be set as fast as possible; rotation time should be the lowest possible to correctly scan a narrow window time using a very high contrast administration flow.
The use of a low-kilovolt setting [100 or 80 KV, depending on body mass index (BMI)] allows a better delineation of high-density structures as the X-ray spectrum created is less penetrating and tends to stop better on high-density structures, in particular on vessels full of iodine contrast media.
The use of milliampere (mA) modulation and an iterative reconstruction algorithm are mandatory to reduce patient exposure, especially for young patients (Table 6.1). In cases of polytrauma patients and high-energy impacts, it is mandatory to comprehend the study of the neck vessels in the total body scan.
Table 6.1
Technical multi-detector computed tomography (CT) parameters
Technical parameter | |
|---|---|
Pitch | Maximum possible |
Gantry rotation | 0.5 s |
Collimation | 0.6 mm |
Trigger-scan delay | 5 s |
Bolus tracking | At the level of aortic arch |
Scan direction | Caudo-cranial |
Multi-phase scan | Pre-contrast, arterial, and venous phase |
Kv | 100 |
mA | Variable with modulation |
Use of the right scan protocol and the choice of the right concentration (g/s) of iodine contrast allow very easy diagnosis of lesions. Automatic or manual reconstruction with the multiplanar reconstruction algorithm, oblique reformation along the vessel axis, and maximum intensity projections (MIP) and volume-rendering (VR) reconstructions allow the easiest recognition of the lesions and better communication with the clinician or surgeon for the right surgical or medical choice and programming [21–23].
6.5.2.2 CT Signs of Pathology
Intraluminal dissection and hematoma of the vessel wall should be visible on unenhanced CT as a “crescent moon” hyperdensity. In many cases the carotid dissection spares the carotid bifurcation and the intracranial part.
The use of an arterial and portal phase scan after the administration of contrast media is mandatory to evaluate the false and real lumen; the real lumen is usually thinner and will be enhanced sooner.
Carotid dissection is characterized by narrowing of the lumen, the intimal flap, which is very well depicted when the right contrast enhancement is achieved (Figs. 6.2, 6.3, and 6.4).






Fig. 6.2
Axial contrast enhancement computed tomography (CT) images of aortic arch dissection after a motor vehicle accident (a). The dissection seems not to involve the origin of common carotid arteries, but there is dissection and occlusion of the internal carotid arteries bilaterally (b). (c) Tridimensional maximum intensity projection (MIP) and volume-rendering (VR) reconstructions

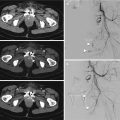
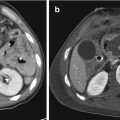
Fig. 6.3
(a) Brain parenchyma the day of the trauma (A) and 2 days after (B). Neck vessels were not included in the first examination. The scan 2 days later included the neck arterial vessels, confirming the right internal carotid dissection and occlusion (b, c)

Fig. 6.4
Bilateral dissection of internal carotid arteries. (a) Axial images demonstrate the bilateral dissection of internal carotid arteries (red arrows). (b) Tridimensional volume rendering reconstruction images of the bilateral dissection of internal carotid arteries
Vertebral arterial dissections are very well depicted with CT angiography. Chen et al. (2004) reported a sensitivity of 100% and specificity of 98%. In CT angiography of the vertebral arteries, the finding of an intimal flap is less common than in the carotid artery with a prevalence of wall hematoma. Potential artifacts in the study of vertebral arteries could be the presence of bone artifacts at the level of the skull base or dental implant artifacts.
Venous injuries are less common in blunt trauma. The most frequent evidence is the presence of a thrombus inside the jugular vein that appears as a hypodense tissue inside the hyperdense contrast (Fig. 6.5).


Fig. 6.5
Traumatic thrombosis of the right jugular vein
6.5.3 MR Angiography
Magnetic resonance (MR) imaging is very difficult to be used suitably for a trauma patient. The high magnetic field and long acquisition times make the continuous monitoring of life parameters quite impossible without the presence of nonmagnetic life support equipment. Other disadvantages of the MR exam are the impossibility of evaluating pulmonary parenchyma and of evaluating many districts in a short time as CT can do.
The advantage of MR exams are that patients are not exposed to ionizing radiation, an advantage when many follow-ups are necessary, especially in young patients (Fig. 6.6). The possibility of evaluating cellular cerebral parenchyma suffering in a very early stage with the use of diffusion-weighted imaging should be an option when clinical evaluation is not possible [24].




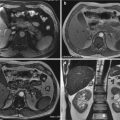
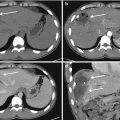
Fig. 6.6
Traumatic partial dissection of the right common carotid artery after a blow with the elbow during a sports activity. Axial CT images (a), multiplanar (MPR) curve reconstruction; magnetic resonance (MR) examination control (b, c)
6.5.3.1 Protocol of Study
The angiographic study of epi-aortic vessels with MR could be done with time-of-flight (TOF) sequences without the administration of contrast media or with phase-contrast and contrast enhancement sequences after the administration of gadolinium-based contrast media. The TOF sequences have less spatial resolution than MR angiography post-contrast sequences, but TOF sequences allow a larger scanning volume in a small scanning time. The TOF sequences for their technical characteristics could create some artifacts when blood flow is not linear. The post-contrast angiographic sequences on the other hand could suffer from some artifacts such as segmental blurring or signal intensity loss in the vertebral artery, especially in a young patient where the blood flow is particularly fast. These artifacts (feathering artifacts) are caused by rapidly changing signal intensity in small vascular structures around the vertebral artery during sampling the central part of the K-space. These artifacts could mimic stenosis or dissection of the vertebral artery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree