Craniovertebral junction (CVJ) disorders in the Occident are usually associated with systemic disorders. In contrast, in the Orient, a greater incidence of isolated CVJ anomalies is seen. Although these are developmental anomalies, they manifest late in life, with trauma and/or infection playing a promotive role. The most significant and common of these anomalies are basilar invagination and atlantodental dislocation, which also occur together. Accurate diagnosis of these anomalies is feasible using computed tomography and magnetic resonance imaging. Greater awareness of this subset of patients is essential for greater understanding and effective management of these ailments.
The junction between the head and neck is called the occipitocervical or craniovertebral junction (CVJ). It provides a bony confine for the spinomedullary junction. It is a complex region that incorporates the occiput as well as the C1 and C2 vertebrae. This region is the most mobile part of the cervical spine and functions as a funnel that confers twin features of stability and motion. This combination of stability and flexibility is provided by the bony as well as ligamentous nature of atlantooccipital and atlantoaxial joints. These joints allow complex movements, with the ligamentous fastenings permitting these motions and the osseous elements providing stability without compromising the traversing neural elements as well as the vertebral artery.
CVJ anomaly is an important clinicopathologic condition among certain ethnic groups and is found more frequently in the Indian subcontinent than anywhere else in the world. Even in India, these anomalies are more frequently documented from northern and north-western states. However, the reason for this, and the incidence, remain elusive. In India, these are the one of the major causes of cervical cord compression. Hence, in every patient presenting with high cervical cord compression in India, CVJ anomalies must be excluded.
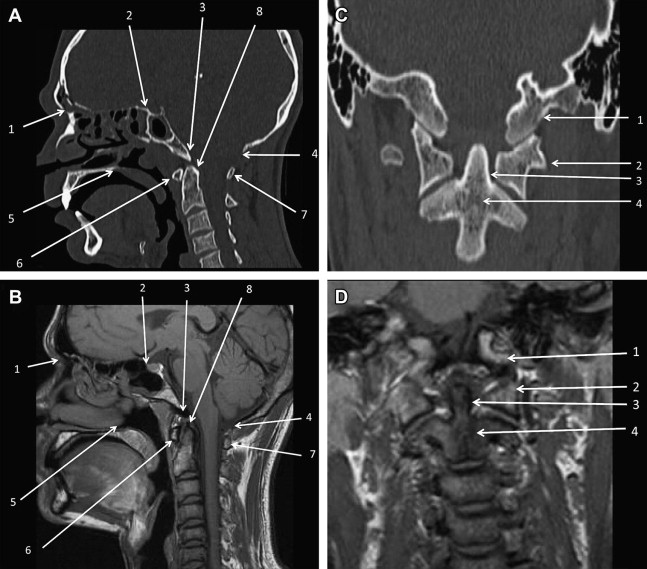
The craniovertebral complex is well visualized on midsagittal magnetic resonance (MR) imaging and reconstructed computed tomography (CT) images ( Fig. 1 ).
This article discusses the normal anatomy of the CVJ and describes the common developmental anomalies affecting it. Relevant embryologic references are also discussed.
Normal bony anatomy
The occipital bone has 3 parts. The basiocciput, which is located anteriorly in the midline, unites with the basisphenoid to form the sphenooccipital synchondrosis in the clivus. It has 2 parts on either side of the foramen magnum, comprising the exoccipital part of the occipital bone. The part of the occipital bone posterior to the foramen magnum is called the supraoccipital part.
The atlas is the first cervical vertebra that holds up the head. It is unique in that it does not have a body, the expected location of which is occupied by the dens. The atlas has 2 lateral masses that are connected by a short anterior, and a longer posterior, arch. The atlas ossifies from 3 ossification centers. The lateral masses of the atlas articulate with the occipital condyles. These articular facets are oval, with their long axes converging anteriorly. The atlantoarticular facets are concave and tilt medially. The transverse processes of the atlas are longer than those of all cervical vertebrae except C7.
The axis is the second cervical vertebra, and acts as a pivot for rotation of the atlas and head around the strong dens. The dens is conical and projects upward from the body of the axis. The posterior surface of the dens is held against the anterior arch of the atlas by the transverse ligament; in doing so, the transverse ligament divides the vertebral canal at the level of the atlas into 2 compartments. The anterior compartment is occupied by the dens, and the posterior two-thirds are occupied by the spinal cord and its covering. In the posterior part, about half is occupied by the cord itself. The axis ossifies from 5 primary and 2 secondary sides of ossification.
Craniovertebral Joints
The articulation between the cranium and the vertebral column is specialized in providing stability along with wide range of motion ( Fig. 2 ). It comprises articulations between the occipital condyles and the atlas and axis, which provides a universal joint permitting horizontal and vertical scanning movements of the head. The atlantooccipital joint articulates the occipital bone of the skull with a pair of synovial joints. The articulating surfaces consist of 2 reciprocally curved articular surfaces, with participation of the occipital condyle and the lateral masses of the atlas. This joint is stabilized by the anterior and the posterior occipital membrane. The atlantoaxial joint has 3 synovial joints; these are a pair of joints between the lateral masses and a median complex between the dens of the axis, which is held between the anterior arch and the transverse ligament of the atlas. The lateral articulating aspects of the atlantoaxial joints are planar. The transverse atlanto ligament is a broad, strong band that arches across the atlantal ring behind the dens. It is cruciate, with a horizontal component located behind the dens; from the median location of this horizontal part, fibers arise that pass upward and downward to insert into the basilar part of the occipital bone and the posterior surface of the axis, respectively.
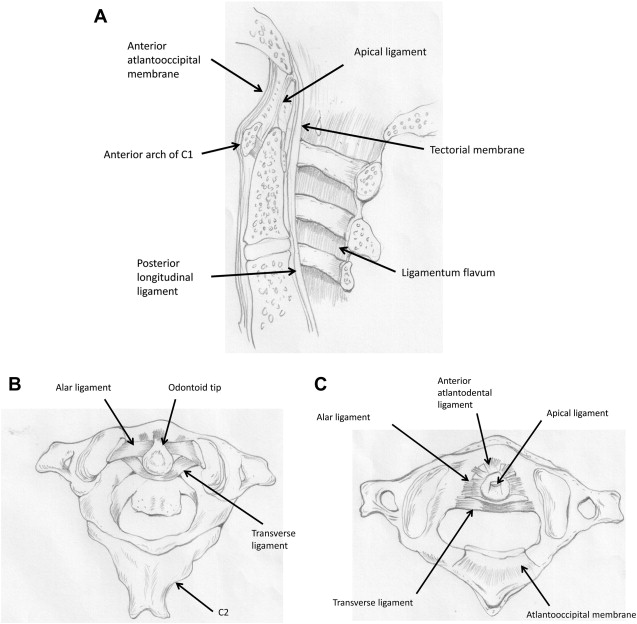
The dens and the occipital bone are connected by the membrana tectoria, the paired alar ligaments, the median apical ligament, and the longitudinal components of the cruciform ligament. The membrana tectoria is the upward continuation of the posterior longitudinal ligament. The alar ligaments are a pair of ligaments that pass horizontally and laterally from the posterolateral aspect of the apex of the dens to the occipital condyles. The apical ligament of the dens passes from the apex of the dens into the anterior margin of the foramen magnum between the alar ligaments. It represents the cranial continuation of the notochord and its sheath. The longitudinal component of the cruciform ligament also connects the axis to the occipital bone.
Movements of the CVJ
The CVJ represents a unique and complex interface responsible for more than half of the rotation and flexion-extension of the cervical spine.
The combination of the bony anatomy, joint articulations, and ligamentous fastenings of the CVJ allow a variety of movements. The atlantoaxial joint allows flexion, extension, axial rotation, and lateral bending. The atlantoaxial ligament allows flexion, extension, and lateral rotation. In axial rotation, as the head rotates in the transverse plane, the axis of motion is the odontoid process. The osseous articulations and their supporting ligaments must resist forces in all axes of motion.
Pathogenesis
Although most of the CVJ anomalies are developmental, trauma plays a role in unmasking these occult abnormalities. The type of trauma also varies; it may be a single episode of significant trauma or may be in the form of repetitive trauma. This may also be in the form of repetitively carrying heavy loads on the head or the upper back. In addition, recurrent viral throat infection, associated with fever, may cause ligamentous laxity caused by hyperemia; these, along with genetic predisposition, are believed to be the causative factors of CVJ anomalies.
Kothari and Goel speculated that basilar invagination is secondary to abnormally inclined alignment of the facets of the atlas and axis. The lateral atlantoaxial joints are planar, which permits slippage. The lack of obliquely locked facet joints also predisposes to this slippage in the presence of ligamentous laxity. The progressive slippage of the atlas over the axis secondary to this malalignment, a process similar to spondylolisthesis in the lumbosacral spine, results in invagination of the odontoid process into the craniocervical cord.
Pathogenesis
Although most of the CVJ anomalies are developmental, trauma plays a role in unmasking these occult abnormalities. The type of trauma also varies; it may be a single episode of significant trauma or may be in the form of repetitive trauma. This may also be in the form of repetitively carrying heavy loads on the head or the upper back. In addition, recurrent viral throat infection, associated with fever, may cause ligamentous laxity caused by hyperemia; these, along with genetic predisposition, are believed to be the causative factors of CVJ anomalies.
Kothari and Goel speculated that basilar invagination is secondary to abnormally inclined alignment of the facets of the atlas and axis. The lateral atlantoaxial joints are planar, which permits slippage. The lack of obliquely locked facet joints also predisposes to this slippage in the presence of ligamentous laxity. The progressive slippage of the atlas over the axis secondary to this malalignment, a process similar to spondylolisthesis in the lumbosacral spine, results in invagination of the odontoid process into the craniocervical cord.
Clinical presentations
Although these anomalies are present at birth, the onset of clinical symptoms is usually observed between 11 and 40 years of age. Male preponderance is seen, with gradual onset.
This condition may take the form of dysfunction of the brainstem, cervical spinal cord, cranial nerves, or the vascular supply to these structures. Myelopathy with pyramidal symptoms forms a dominant component. Spinothalamic dysfunction is less frequent.
Neck pain was a major presenting symptom in 77% of patients, whereas torticollis was present in 41% of patients. Lower cranial nerve dysfunction has been found to be present in 20% of children with basilar invagination. Neck pain, muscle spasms, and restriction of neck movements are frequently noted, suggesting instability of the region.
In addition, patients with atlantooccipital assimilation have a characteristic appearance with a short, broad neck, scapular elevation, low posterior hairline, and limitation of neck movements.
Craniometry
Craniometry of the CVJ uses a series of lines, planes, and angles to define the normal anatomic relationships of the CVJ. There has been renewed interest in the normal anatomy and pathology of the CVJ with the development of high-resolution CT and MR imaging. The anatomic landmarks described for plain radiographs and tomograms are well visualized on midsagittal MR and reformatted CT images (see Fig. 1 A, B). Some of these lines ( Table 1 ) have been recently reviewed and are shown in Fig. 3 . Another measurement of importance is the distance of the odontoid tip to the pontomedullary junction. This distance, as observed on MR imaging, is a useful index to define the reduction of the posterior cranial fossa bone size.
| Synonyms | Definition | Normal Measurements | Implications | |
|---|---|---|---|---|
| 1. | Chamberlain line | Joins posterior margin of hard palate to opisthion | Tip of dens should not exceed 5 mm above the line | Odontoid process bisects the line in basilar invagination |
| 2. | McGregor line | Joins posterior margin of hard plate to undersurface of occipital bone | Tip of dens should not exceed 7 mm above the line | Line position varies with flexion/extension hence has low significance |
| 3. | McRae line | Joins anterior and posterior edges of foramen magnum (basion to opisthion) | Tip of dens does not exceed this line | When sagittal diameter is <20 mm, neurologic symptoms occur (foramen magnus stenosis) |
| 4. | Wackenheim clivus line | Line drawn along clivus into cervical canal | Odontoid tip is ventral and tangential to this line | Odontoid process transects the line in basilar invagination or forward position of skull |
| 5. | Height index of Klaus | Distance between tip of dens and tuberculum-torcular line | 40–41 mm | <30 mm seen in basilar invagination |
| 6. | Welcher basal angle | Angle between the lines drawn from nasion to tuberculum sellae and tuberculum sellae to basion | 124°–142° | Widening is called platybasia |
| 7. | Clivus canal angle | Angle formed at junction of Wackenheim line and posterior vertebral body line | 180° in extension 150° in flexion <150° considered abnormal | |
| 8. | Atlantooccipital joint axis angle (Schmidt) | Angle formed at the junction of lines traversing the atlantooccipital joints | 125°–130° | Less than 124° is seen in condylar hypoplasia |
| 9. | Fishgold digastric line | Joins the fossae for digastric muscles on undersurface of skull (just medial to mastoid process) | Dens tip should not project above this line. Central axis of dens should be perpendicular to the line | Corresponds to McRae line on lateral view; may be oblique in unilateral condylar hypoplasia; oblique odontoid suggests paramedian abnormality |
| 10. | Fishgold bimastoid line | Line connecting tips of mastoid process | Runs across atlantooccipital joints, line is 10 mm below digastric line | Odontoid tip may be the line |
Imaging considerations
Multimodality imaging of the craniocervical junction is integral to the detection, classification, and surgical planning for the treatment of basilar invagination.
Conventional Radiography
Standard views of the cervical spine with minimal magnification are taken and these include lateral, open-mouth frontal, and dynamic flexion-extension views. Manipulation for flexion/extension views needs to be done gently and cautiously to minimize the risk of neurologic compression resulting from manipulating an unstable joint.
CT
High-resolution multidetector CT (MDCT) with isotropic reconstruction is an ideal modality for evaluation of complex osseous anatomy associated with CVJ anomalies. After axial images are obtained, these are isotropically reconstructed in multiple planes. In addition to multiplanar reconstructions (MPR), shaded surface displays (SSD) as well as volume-rendered techniques (VRT) are useful in the evaluation of bony anomalies. In the pediatric age group, rapid scanning with CT allows an examination to be performed even without sedation. The short scan time associated with CT is also beneficial in the evaluation of dynamic mobile atlantoaxial subluxation. The inherent risk of neurologic compression associated with manipulation of these unstable dislocations is reduced owing to the shorter scan time. In addition, CT angiography can also help in detecting the osseous abnormalities associated with an abnormal route of the vertebral artery, especially in patients with occipitalization of the atlas ( Figs. 4 and 5 ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree