Epilepsy is a major public health problem in many tropical countries. Also, some of the tropical diseases are major contributors to the higher prevalence of epilepsy in these countries. The etiologic factors responsible for epilepsy in these countries are quite different from those in the developed world. This article discusses the etiologic factors and neuroimaging of epilepsy in light of the conditions in these tropical countries.
Epilepsy is a major public health problem in many tropical countries. Also, some of the tropical diseases are major contributors to the higher prevalence of epilepsy in these countries. The tropics have a relatively uniform hot climate present throughout the year associated with heavy rainfall causing higher humidity. Higher temperatures and humidity may favor replication of pathogenic agents both inside and outside the biological system. Infectious endemic tropical diseases disproportionately affect poor and marginalized populations in developing regions of Africa, Asia, Central America, and South America, resulting in a major public health hazard. Poor socioeconomic status promotes disease through undernutrition, poor sanitation, breeding of insects and rodents, and inaccessibility to medical care. Hence, many tropical countries fall into the category of resource-poor countries. Prenatal risk factors, traumatic brain injuries (TBIs), various parasitic infestations, and infections of the central nervous system (CNS) are much more common in tropical countries. The International League against Epilepsy (ILAE) has established a separate Commission on Tropical Diseases to study the epidemiology, etiology, and prognosis and to seek solutions to the problems faced by the population in the tropics.
Epidemiology
Incidence and prevalence rates of epilepsy tend to be higher in resource-poor, tropical, and developing countries. Placencia and colleagues in 1992 reported an incidence of 122 per 100,000 per year in Ecuador, South America. In general, prevalence figures from studies in Latin America have been higher than those in the developed world. Incidence rates from 28.8 per 100,000 to 35.0 per 100,000 per year have been reported in the general population in China. The results from India are higher and have been reported as 60 per 100,000 per year. China and India, the 2 most populous nations in the world, together contribute approximately 20% of the people with epilepsy worldwide. The age-adjusted incidence of epilepsy reported from the developed countries is 24 to 53 per 100,000 per year. The annual incidence rates for epilepsy in Asia did not differ significantly from the rates in developed countries, but the incidence rates were higher in sub-Saharan Africa and Latin America (63–158 and 78–190 per 100,000 person-years, respectively).
A higher prevalence is seen in rural areas. Although there is a steady increase in epilepsy prevalence rates with advancing age in the developed countries, the rates seem to peak in the second decade in tropical and resource-poor countries.
Diagnosis
Diagnosis of epilepsy is based on clinical judgment, findings on electroencephalography (EEG), and imaging. The skill and experience of the physician and the information provided by witness are important in making the proper clinical judgment. The neurologists and physicians managing epilepsy are fewer in most of these countries. Although EEG facilities are available, there are no minimum standards and no governmental or professional authorities to ensure quality control. Imaging facilities are few, along with low affordability of imaging. In a 2006 survey of the diagnostic facilities for epilepsy care around the world, magnetic resonance imaging (MRI) facilities were available in almost all European and North American countries compared with only 26% of African, 48% of western Pacific, and 56% of Southeast Asian countries.
Moreover, most MRIs performed outside comprehensive epilepsy care facilities do not conform to the specification laid down for patients with chronic epilepsy. Repeating MRI and performing more costly investigations, such as single photon emission computed tomography and positron emission tomography, can add to the cost of diagnosis and management.
Diagnosis
Diagnosis of epilepsy is based on clinical judgment, findings on electroencephalography (EEG), and imaging. The skill and experience of the physician and the information provided by witness are important in making the proper clinical judgment. The neurologists and physicians managing epilepsy are fewer in most of these countries. Although EEG facilities are available, there are no minimum standards and no governmental or professional authorities to ensure quality control. Imaging facilities are few, along with low affordability of imaging. In a 2006 survey of the diagnostic facilities for epilepsy care around the world, magnetic resonance imaging (MRI) facilities were available in almost all European and North American countries compared with only 26% of African, 48% of western Pacific, and 56% of Southeast Asian countries.
Moreover, most MRIs performed outside comprehensive epilepsy care facilities do not conform to the specification laid down for patients with chronic epilepsy. Repeating MRI and performing more costly investigations, such as single photon emission computed tomography and positron emission tomography, can add to the cost of diagnosis and management.
Epilepsy care and treatment
There is great variability in the disease management of epilepsy among different countries, more so between tropical countries and countries in North America and Europe.
Treatment Gap
The treatment gap is defined as the number of people with active epilepsy not on treatment or on inadequate treatment expressed as a percentage of the total number of people with active epilepsy. A recent systematic analysis that investigated the magnitude of the treatment gap in resource-poor countries found an overall rate of 56%. A large proportion of patients with epilepsy discontinue the treatment despite being diagnosed and initiated on antiepileptic drug (AED) treatment. The main reasons cited for AED discontinuation were the inability to afford the treatment and a lack of information about the consequences of medication nonadherence. Similar to the medical treatment gap, surgical treatment gap also exists in many of these countries. Despite the total direct cost of presurgical evaluation and surgery in most tropical countries amounting to a small fraction of the cost incurred in North America and Europe, this expenditure is still beyond the reach of most patients.
Knowledge, Attitudes, and Practice
Numerous studies on knowledge, attitudes, and practice of epilepsy have been done in the tropical population. Misunderstanding of epilepsy is quite common. Social stigma to epilepsy often causes more distress to a person with epilepsy than the seizures themselves. Lack of awareness is one of the most important factors for this social stigma. There is an increased need for health education campaigns to rehabilitate patients with epilepsy in these communities and to improve their quality of life.
Etiology and imaging
The Commission on Epidemiology and Prognosis of the ILAE has suggested that seizures should first be classified etiologically according to the presence or absence of a presumed causative or precipitating insult. Before the computed tomography (CT) era, a large number of patients were classified to have epilepsy of unknown origin. This number has reduced after the advent of CT and MRI. There is a difference in the cause of epilepsy that is noted in studies from developed countries and tropical countries. In developed countries, the common causes are vascular, traumatic, or neoplastic, whereas studies from Latin America and Asian tropical countries have found a large number of patients in the symptomatic group with neurocysticercosis (NCC). The other causes included in the developing countries are perinatal damage, head injuries, cerebrovascular diseases, and other brain infections. Neuroinfections can present acutely with seizures as is seen in cerebral malaria or Japanese encephalitis. Neuroinfections can also present chronically as an epilepsy syndrome secondary to the presence of focal granulomatous lesions or gliosis and calcification secondary to NCC.
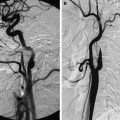
Single ring-enhancing lesion
One of the common imaging finding in a patient from tropical country presenting with seizure is a single ring-enhancing lesion (SREL). SREL may occur in several infectious and neoplastic diseases of the CNS and is the most common radiologic abnormality seen in patients with acute-onset seizures in developing tropical countries. Most common differential for single enhancing lesion on CT or single hyperintense lesion on MRI in endemic areas is NCC versus tuberculosis (TB). Clinical presentation and CT remains the mainstay of diagnosis in the developing world. The clinicoradiologic picture forms the basis of diagnostic criteria for evaluation of SREL as proposed by Rajshekhar and colleagues. These investigators made an attempt to differentiate between these 2 entities on the basis of clinical and imaging features. Rajshekhar and Chandy noted that
- 1.
Cysticerci are usually round in shape.
- 2.
Cysticerci are usually 20 mm or less in size with ring enhancement or visible scolex.
- 3.
The cerebral edema is not severe enough to produce midline shift or focal neurologic deficit.
In contrast, tuberculomas are usually irregular, solid, and larger than 20 mm in size. They are often associated with severe perifocal edema and focal neurologic deficit. These diagnostic criteria according to Rajshekhar and colleagues showed high sensitivity and specificity and high positive and negative predictive values. However, it has been noticed that even if a patient does not fulfill these diagnostic criteria, it does not exclude the possibility of a cysticercal cause and vice versa. Most of these solitary enhancing lesions disappear within weeks or months ( Fig. 1 ). These patients require only antiepileptic therapy, and medication may be withdrawn safely after the resolution of the lesion. Only a few patients, atypically, experience seizures even after disappearance of the lesion. Studies have shown that neither albendazole nor antituberculous therapy is helpful in modifying the natural course of these lesions or associated seizure disorder. If the lesion increases in size and if focal neurologic deficits manifest or seizures are uncontrolled, then brain biopsy may be required to establish final diagnosis.
Advanced imaging is well exploited to further characterize these SREL and to differentiate between NCC and TB. Magnetization transfer (MT) can help differentiate between T2 hypointense NCC and tuberculomas. Cysticercus granulomas have a significantly higher MT ratio than similar-appearing tuberculomas because of the presence of lipid-containing caseous necrosis in T2 hypointense tuberculomas. MT also helps in delineating perilesional gliosis in treated cases, which may be responsible for persistent seizures in few cases. Perilesional gliosis visible on MT spin echo MRI correlates with seizure recurrence. Three-dimensional constructive interference into steady state/3-dimensional fast imaging employing steady-state acquisition and fluid-attenuated inversion recovery are good sequences for visualizing the scolex, which is pathognomonic for NCC. Differentiation between NCC and tuberculoma is also possible on magnetic resonance spectroscopy. Tuberculomas show higher lipid peaks, more choline levels, less N -acetylaspartate levels, and less creatine levels than NCC, with choline to creatine ratio always greater than 1 in tuberculomas. T2 hyperintense tuberculomas (tuberculomas with liquid caseation) can show diffusion restriction ( Fig. 2 ) and can be differentiated from NCC, whereas T2 hypointense tuberculomas (tuberculomas with solid caseation) do not show diffusion restriction.
The other differentials for SREL are cerebral abscess, metastasis, glioma, subacute infarct, and demyelination. Thick and nodular enhancing walls with increased perfusion favor neoplasm, whereas thin regular enhancing walls, perilesional edema, low T2 signal, and diffusion restriction favor abscess. Incomplete ring with minimal perilesional edema favors demyelination. In endemic regions, differentials of fungal infection, such as cryptococcal granulomas, also need to be considered irrespective of the immune status of the patient. Magnetic resonance spectroscopy detection of alpha, alpha-trehalose, which is specific but less sensitive, could help in differentiating cryptococcoma from tuberculoma.
Febrile convulsions and mesial temporal sclerosis
Febrile seizures are defined as seizures that occur in infants and children aged between 6 months and 6 years, accompanied by fever (at least 38°C before the onset of seizure). Febrile convulsions (FC) are among the most frequent seizure disorders in children. Lifetime risk for FC is relatively high in developing countries. Lower socioeconomic status and lack of knowledge about FC are the main factors related to this risk. Retrospective studies have shown that prolonged febrile seizures are a causative factor for the later development of mesial temporal sclerosis (MTS) and temporal lobe epilepsy. Prolonged febrile seizures can produce acute hippocampal injury that evolves to hippocampal atrophy and subsequent temporal lobe epilepsy.
MTS is one of the most common causes of intractable epilepsy in tropical and developing countries. MRI shows volume loss and signal changes in the hippocampus and mesial temporal structures reflecting gliosis. In few patients with MTS, there can be associated malformation of cortical development, gliosis, or calcified granuloma ( Fig. 3 ). This association is sometimes referred to as dual pathology. The best conventional magnetic resonance sequences to show alterations in the normal cytoarchitecture within hippocampus are inversion recovery and high-resolution fast-spin echo images. The 3-dimensional spoiled gradient echo imaging provides good information regarding hippocampal volume loss on the side of sclerosis. A smaller degree of asymmetry in volume and T2 signal is best detected by volumetric quantification and T2 relaxometry, respectively. Measurement of apparent diffusion coefficient can also help lateralize the lesion side reflecting neuronal loss and gliosis. Secondary imaging criteria, such as atrophy of ipsilateral mammillary body and fornix, atrophy of collateral white matter, atrophy of ipsilateral temporal lobe/hemisphere, and prominence of temporal horn, increase diagnostic confidence.