The myelin sheath and oligodendrocytes in the brain may be damaged by autoimmune-mediated inflammatory processes secondary to postinfectious demyelination or nutritional and vitamin deficiency. This article describes acute disseminated encephalomyelitis, acute hemorrhagic leukoencephalitis, acute necrotizing encephalopathy, and tumefactive demyelination as well as osmotic demyelination, Wernicke encephalopathy, Marchiafava–Bignami disease, and subacute combined degeneration of the spinal cord. Although some characteristic MR imaging features allow radiologists to suggest a diagnosis, these may overlap, and images should be interpreted in light of clinical symptoms and laboratory investigations.
The white matter of the brain may be damaged in a variety of conditions, including inflammatory demyelination. Apart from the leukodystrophies (also called dysmyelinating disorders), which are characterized by defective formation or maintenance of myelin in younger patients, demyelinating diseases in the central nervous system are typically classified as primary (of unknown cause, archetypically multiple sclerosis [MS]) or secondary (from other causes) ( Box 1 ). Although secondary white matter disease may have varied and sometimes doubtful causes, the underlying pathologic change seems to be damage to the myelin sheath and oligodendrocytes (the cells that form the myelin). This report focuses on postinfectious demyelination and nutritional disorders of the nervous system, and also discusses tumefactive demyelinating lesions that may mimic neoplasm on neuroimaging.
Primary demyelinating disease
- 1.
MS
- 2.
Neuromyelitis optica
Secondary demyelinating disease
- 1.
Associated with infectious agents
- a.
Acute disseminated encephalomyelitis (ADEM)
- b.
Acute hemorrhagic leukoencephalitis (AHLE)
- c.
Acute necrotizing encephalopathy (ANE)
- d.
Subacute sclerosing panencephalitis (SSPE)
- e.
HIV encephalitis and progressive multifocal leukoencephalitis
- a.
- 2.
Associated with nutritional deficiency
- a.
Osmotic demyelination (central pontine and extrapontine myelinolysis)
- b.
Wernicke encephalopathy
- c.
Marchiafava-Bignami disease (MBD)
- d.
Subacute combined degeneration of the spinal cord (SACD)
- e.
Copper deficiency myelopathy
- a.
- 3.
Associated with physical, chemical, toxic, or hypoxic/ischemic causes
- a.
Radiotherapy and chemotherapeutic agents
- b.
Chemicals (eg, toluene and mercury)
- c.
Hypertensive encephalopathy and posterior reversible encephalopathy syndrome
- d.
Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy
- a.
White matter diseases associated with infections
White matter diseases associated with infectious agents may be caused by autoimmune-mediated damage to the oligodendrocytes, myelin destruction by cross-reaction against viral antigens, or direct infection of the glial or neuronal cells of the brain. The latter group, which includes subacute sclerosing panencephalitis, progressive rubella panencephalitis, HIV encephalitis, and progressive multifocal leukoencephalitis, typically manifest months or years later and are not discussed in this report.
Acute Disseminated Encephalomyelitis
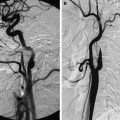
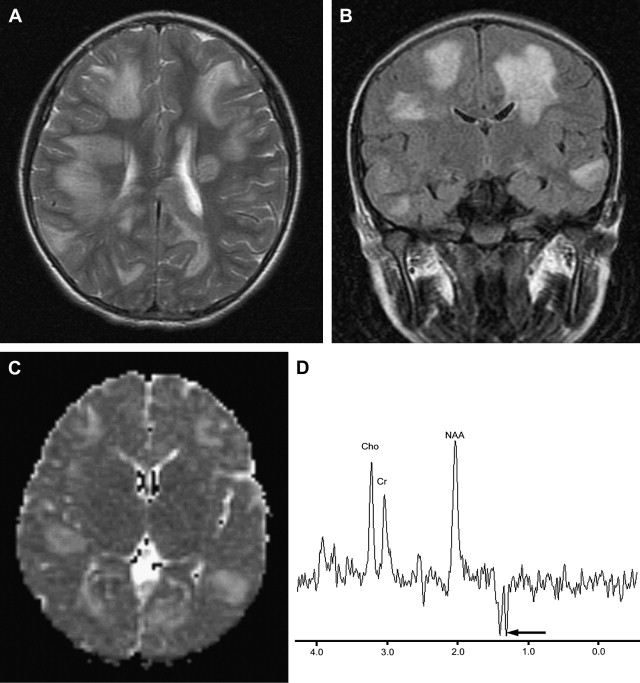
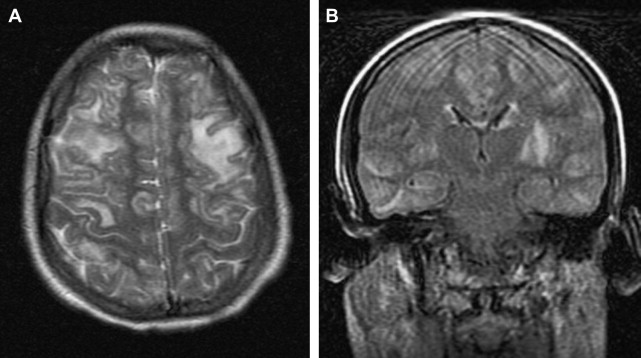
Frequently described in children ( Fig. 1 ), but also found in adult patients ( Fig. 2 ), ADEM is thought to be a monophasic self-limited, autoimmune response to central nervous system antigen triggered by viral infections. The virus is usually not recovered from the brain. Histologically, ADEM is similar to experimental allergic encephalomyelitis, with inflammatory cell (primarily lymphocytic) infiltration and demyelination. A wide range of conditions are associated with ADEM, including non-specific respiratory infection, specific viral illness (such as measles, rubella, mumps, and chickenpox), and vaccination (including diphtheria, smallpox, tetanus, and typhoid); ADEM may even arise spontaneously.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree