ACUTE HYPERTENSIVE HEMORRHAGES
KEY FACTS
 The most common etiologies for all intracerebral hemorrhage include hypertension, ruptured aneurysm or vascular malformation, venous thrombosis, amyloidosis (in patients over 60 years of age), collagen vascular disorders, anticoagulation therapies, vasculitis (including moyamoya) neoplasias (primary and métastases), and cocaine use.
The most common etiologies for all intracerebral hemorrhage include hypertension, ruptured aneurysm or vascular malformation, venous thrombosis, amyloidosis (in patients over 60 years of age), collagen vascular disorders, anticoagulation therapies, vasculitis (including moyamoya) neoplasias (primary and métastases), and cocaine use.
 Hypertensive bleeds account for 10% of all “strokes” and have a 50% mortality.
Hypertensive bleeds account for 10% of all “strokes” and have a 50% mortality.
 Hypertension bleeds are more common in males 60 to 80 years old; common locations include basal ganglia (60% to 70%, particularly the putamen), thalamus (10% to 20%), pons (5% to 10%), dentate nuclei (1% to 5%), and hemispheric (1% to 2%).
Hypertension bleeds are more common in males 60 to 80 years old; common locations include basal ganglia (60% to 70%, particularly the putamen), thalamus (10% to 20%), pons (5% to 10%), dentate nuclei (1% to 5%), and hemispheric (1% to 2%).
 Hemorrhages associated with anticoagulation are large and have a complex appearance (due to rebleeds).
Hemorrhages associated with anticoagulation are large and have a complex appearance (due to rebleeds).
 Main differential diagnosis when hemorrhage occurs at an atypical location or age: rule out underlying lesion (arteriovenous malformation, aneurysm, tumor, amyloidosis).
Main differential diagnosis when hemorrhage occurs at an atypical location or age: rule out underlying lesion (arteriovenous malformation, aneurysm, tumor, amyloidosis).
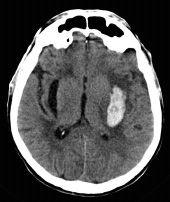
FIGURE 10-1. Axial computed tomography (CT) shows acute dense hemorrhage in left basal ganglia with surrounding edema and cerebrospina fluid-filled cleft in right putamen from a prior hemorrhage.
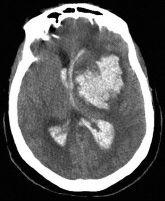
FIGURE 10-2. Axial CT, in a different patient, shows large left basal ganglia with ventricular extension.

FIGURE 10-3. Axial CT, in a different patient, shows a right thalamic hemorrhage with ventricular extension.
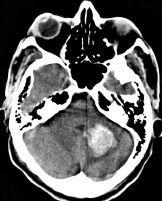
FIGURE 10-4. Axial CT, in a different patient, shows a left medial cerebellar hemorrhage.
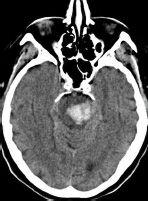
FIGURE 10-5. Axial CT, in a different patient, shows a pontine bleed.

FIGURE 10-6. Axial CT, in different patient, shows a massive brain stem acute hematoma.
SUGGESTED READING
Gokaslan ZL, Narayan RK. Intracranial hemorrhage in the hypertensive patient. Neuroimaging Clin North Am 1992;2:171–186.
KEY FACTS
 Related to hypertension, more common with increasing age and male gender.
Related to hypertension, more common with increasing age and male gender.
 When related to hypertension, they tend to cluster around deep cerebral and cerebellar structures, generally found in presence of underlying white matter disease.
When related to hypertension, they tend to cluster around deep cerebral and cerebellar structures, generally found in presence of underlying white matter disease.
 When related to amyloidosis, they tend to occur in the cortex, cortical surface, or subcortical white matter; superficial siderosis maybe present; white matter disease is also present
When related to amyloidosis, they tend to occur in the cortex, cortical surface, or subcortical white matter; superficial siderosis maybe present; white matter disease is also present
 High number correlate with decreased cognition.
High number correlate with decreased cognition.
 May predict fatal future hemorrhages and infarctions.
May predict fatal future hemorrhages and infarctions.
 May predict bleeding in anticoagulated patients.
May predict bleeding in anticoagulated patients.
 Better seen on SWI than on gradient echo imaging.
Better seen on SWI than on gradient echo imaging.
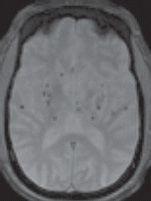
FIGURE 10-7. Axial T2* shows dark microbleeds clustered in deep brain regions.
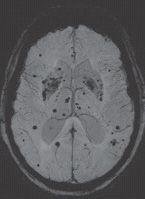
FIGURE 10-8. Axial SWI, in a different patient, shows innumerable microhemorrhages particularly in and around the basal ganglia, but some subcortical ones are also present.
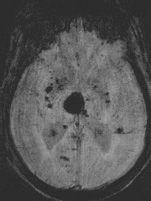
FIGURE 10-9. Axial SWI, in a different patient, shows acute right thalamic dark hemorrhage and multiple microbleeds.
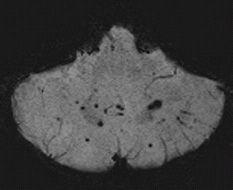
FIGURE 10-10. Axial SWI, in a different patient, shows microbleeds in deep central regions of cerebellum.
SUGGESTED READING
Naka H, Nomura E, Takahashi T, Wakabayashi S, Mimori Y, Kajikawa H, et al. Matsumoto Combinations of the presence or absence of cerebral microbleeds and advanced white matter hyperintensity as predictors of subsequent stroke types. Am J Neuroradiol 2006;27:830–835.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree