Normal Anatomic Variants and Miscellaneous Skeletal Anomalies
Lee F. Rogers
L. F. Rogers: Department of Radiology, Wake Forest University School of Medicine, Winston-Salem, North Carolina 27157.
Unlike the congenital and genetic disorders described in Chapter 9, the anatomic variants and miscellaneous skeletal anomalies described here are encountered daily in the practice of radiology. A general familiarity with these structures and their variants is necessary to lessen concern, decrease confusion, and increase the accuracy and confidence of radiographic interpretation. Their importance lies in the fact that they can easily be misinterpreted as pathologic conditions by those unfamiliar with them, when in reality they are of little or no clinical significance. When misconstrued as an abnormality they may lead to costly and unnecessary additional examinations. One of the principal differences between the trained and experienced diagnostic radiologist and other physicians is the ability of the radiologist to recognize and dismiss normal variations, thereby avoiding a potentially expensive, added workup for the patient. The texts by Keats9 and by Kohler and Zimmer11 are excellent, thorough references devoted to this subject. It is difficult to conceive of practicing radiology without one or both of them close at hand. In this chapter, only the most common variants of the peripheral skeleton are described. Many are found in the skull and spine and are covered in Chapters 11 and 12, respectively.
Miscellaneous skeletal anomalies are isolated, anomalous developments. In most cases, they are sporadic and nonfamilial. They may be considered as (1) supernumerary developments, (2) a failure to develop, or (3) segmentation defects.
Supernumerary development is usually seen in the hands and feet as the development of an extra digit (polydactyly) on either side of the hand or foot (Fig. 8-1). These may be sporadic or genetically determined and, at times, are associated with malformation syndromes.
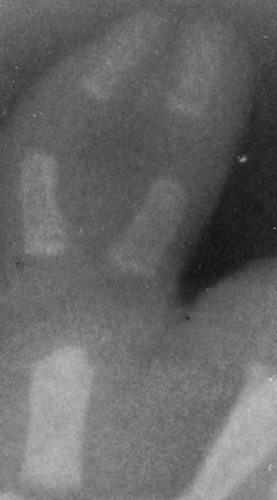 FIG. 8-1. Duplication of the thumb in the newborn. Note the two separate and distinct distal and proximal phalanges, with fusion of the intervening soft tissues. |
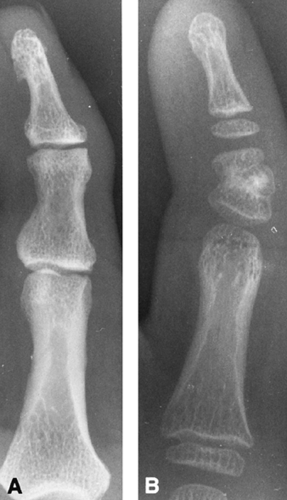
Failure to develop is usually either hypoplasia of a structure or, less commonly, aplasia. Hypoplasia is most commonly identified in the middle phalanx of the fifth digit and is known as clinodactyly (Fig. 8-2). This condition may be sporadic, familial, or associated with a whole host of congenital disorders. Hypoplasia and aplasia are most commonly encountered in the posterior elements of the spine, particularly in the pedicle and transverse process.
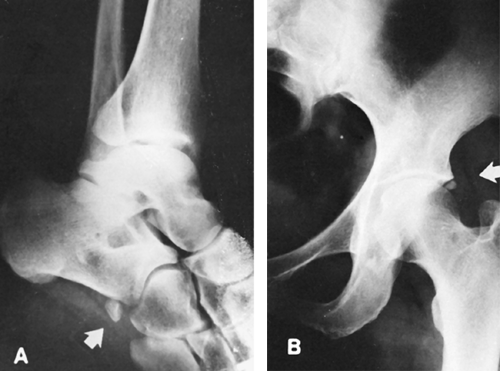
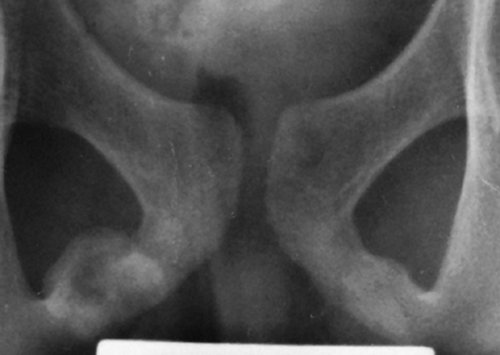
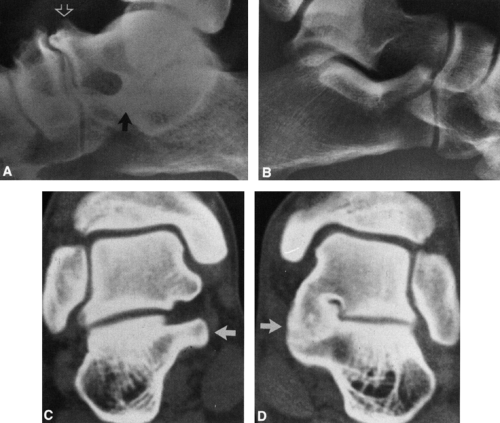
Defects of segmentation are common. They may consist of a fusion of segments, commonly encountered in the vertebrae as a partial or complete fusion of two or more vertebral bodies, which is described in Chapter 12. Fusion occurs less commonly in the carpal (Fig. 8-3) and tarsal bones. The fusion of tarsal bones is often symptomatic (Fig. 8-39 and 8-40).
 FIG. 8-3. Lunatotriquetral fusion in a 13-year-old girl. The lunate (L) and triquetrum (T) are fused, and there is a small, incomplete cleft between them distally. |
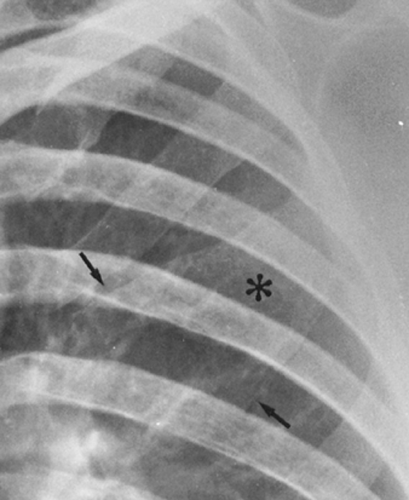
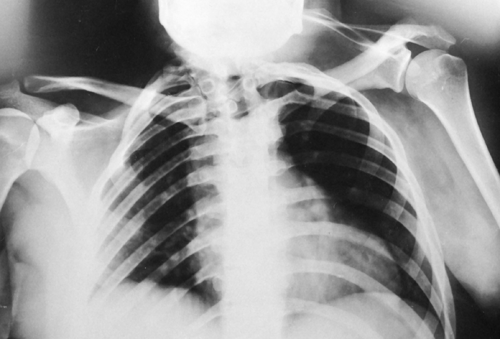
 FIG. 8-11. Student’s tumor. Prominent ossification in the cartilaginous ends of the first ribs (arrow). These are easily misconstrued as tumors in the underlying lung. |
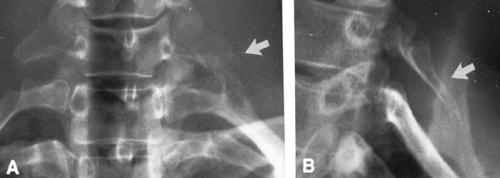
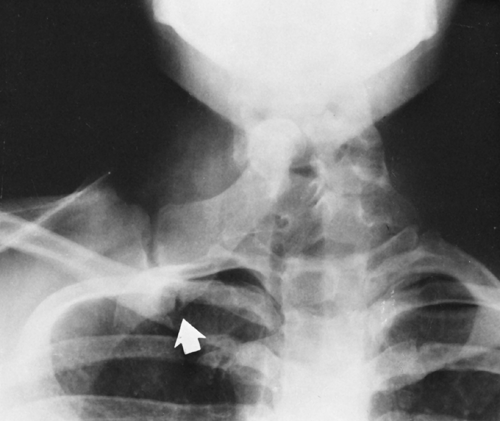 FIG. 8-17. The omovertebral bone in association with Sprengel’s deformity. The bone forms an articulation with the scapula (arrow) and the arch of one of the cervical vertebrae. |
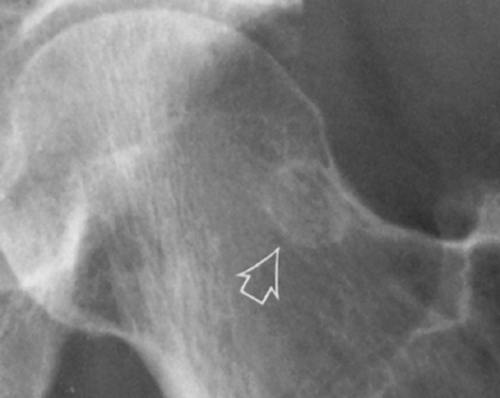
 FIG. 8-18. Pseudocyst of the humeral head. A radiolucency is present within the greater tuberosity because of the relative absence of bone trabeculae. This is a frequent normal finding that is easily mistaken for evidence of metastatic disease or other abnormalities (see Fig. 8-34). |
 FIG. 8-19. Proximal humeral epiphysis. Anteriorly the growth plate is chevron shaped, whereas posteriorly it is transverse (arrow) and could be misconstrued as a fracture. |
 FIG. 8-21. Supraclavicular nerve foramen. The small lucency in the superior cortex of the middle third of the clavicle (arrow) represents a foramen for the supraclavicular nerve. |
 FIG. 8-31. Blount’s disease. There is bilateral involvement, with an angular deformity at the physis. The tibial shafts are straight and the femurs are uninvolved. |
 FIG. 8-32. Pellegrini-Stieda disease. A thin, shell-like calcification is seen at the superior margin of the medial femoral condyle (arrow). |
 FIG. 8-33. Cortical desmoid. Note the irregularity of the surface of the cortex of the distal femur (arrows) at the site of the insertion of the adductor magnus and gastrocnemius muscles. |
 FIG. 8-36. Bifid sesamoids. Both the medial and lateral sesamoids of the great toe are bifid (arrows). |
 FIG. 8-37. Pseudocyst of the calcaneus. The relative radiolucency beneath the tuber angle (arrow) represents an area devoid of trabeculae. This is a normal finding and is similar to the pseudocyst of the humeral head seen in Fig. 8-18. |
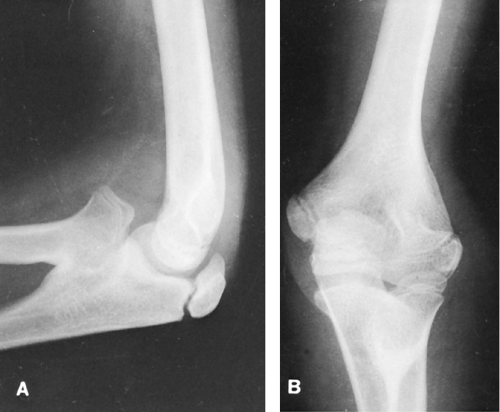 FIG. 8-38. Congenital radioulnar synostosis with congenital dislocation of the head of the radius. There is bony fusion between the proximal radius and the ulna. |
 FIG. 8-39. Tarsal coalition, calcaneonavicular bar (arrow). Note also the thin, white line paralleling the distal tibial joint surface. This is an epiphyseal scar, the bony residua of the physis. |
The failure of segments to fuse is most commonly encountered in the spine, involving the laminae and spinous processes. This failure of fusion is known as spina bifida. When seen as an isolated radiographic abnormality, it is known as spina bifida occulta. It may be associated with other congenital abnormalities of the spine, as described in Chapter 12.
Bifid structures may also occur. These may develop from a natural growth, as in the bifid anterior margin of ribs (Fig. 8-4), or from a failure of fusion of structures that arise from more than one center, most commonly in the sesamoids of the great toe (see Fig. 8-36). Certain apophyses and epiphyses arise from multiple centers of ossification, which eventually fuse in most cases. Multiple centers of ossification are seen in the proximal humerus and elbow. The trochlear center of ossification of the elbow itself may arise from separate centers, as may the epiphyses of the proximal phalanx of the great toe. Less commonly, individual carpal or tarsal bones arise from separate centers of ossification.
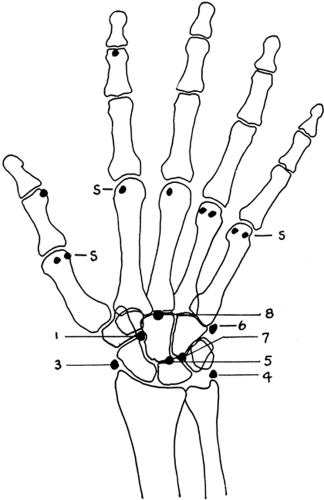
Accessory centers of ossification and accessory bones are found rather frequently in the skeleton (Figs. 8-5 and 8-6). An accessory bone represents either a supernumerary ossicle not ordinarily found in the skeleton or a secondary center of
ossification that has failed to fuse and remains as a separate structure (Fig. 8-7). On occasion, they may predispose to injury or degenerative change and be responsible for symptoms.13, 15, 23 This is often associated with a positive bone scan in the region of the abnormality. Sesamoid bones (Fig. 8-8) arise in tendons, particularly those of the feet, and are very similar in appearance to accessory centers of ossification. These small accessory bones and sesamoids may be mistaken for pathologic conditions, particularly fractures, and knowledge of their distribution and frequency is therefore important.
ossification that has failed to fuse and remains as a separate structure (Fig. 8-7). On occasion, they may predispose to injury or degenerative change and be responsible for symptoms.13, 15, 23 This is often associated with a positive bone scan in the region of the abnormality. Sesamoid bones (Fig. 8-8) arise in tendons, particularly those of the feet, and are very similar in appearance to accessory centers of ossification. These small accessory bones and sesamoids may be mistaken for pathologic conditions, particularly fractures, and knowledge of their distribution and frequency is therefore important.
DIFFERENTIATION OF ANOMALOUS BONES FROM FRACTURES
A fracture line is ragged along its margin, irregular, and poorly defined; anomalous ossification centers and sesamoids are characterized by smooth cortical margins (see Figs. 8-5, 8-7, and 8-8). An avulsion or small fracture has an irregular, uncorticated surface at the line of fracture and a defect in the adjacent bone that corresponds to the avulsed fragment. Fresh fractures are accompanied by swelling of the contiguous soft tissue, which should not be present about an accessory center. Accessory centers and anomalous bones are commonly bilateral. Examination of the corresponding part of the opposite extremity is helpful in doubtful cases, but it is usually unnecessary. The precise diagnosis can usually be determined by reference to standard charts and diagrams (see Figs. 8-7 and 8-23).4
Normal Radiographic Findings Confused with Pathology
Nutrient Canals and Foramina
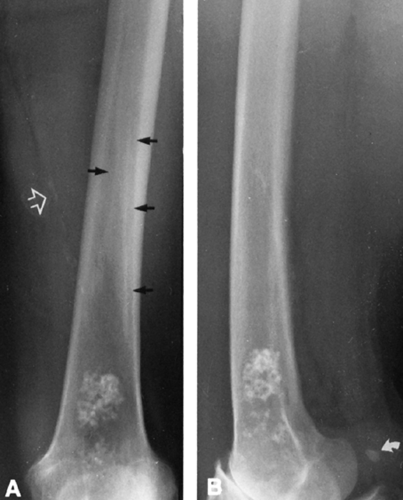
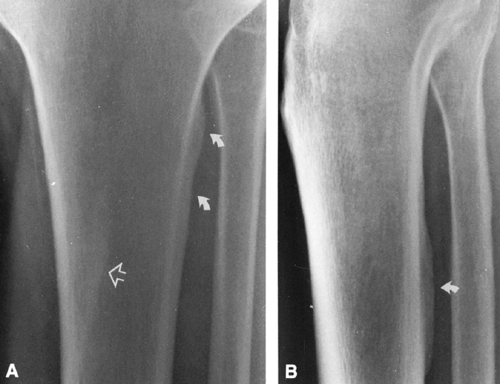
Nutrient canals are present in all the long and short tubular bones. These are fine, sharply marginated radiolucencies that extend obliquely
through the cortex, and they should not be mistaken for a fracture (Fig. 8-9). Nutrient canals are less radiolucent than a fracture and have a characteristic course. Nutrient foramina generally occur at the ends of bones, appearing as a small circular radiolucency, and are seen most commonly at the intercondylar notch of the knee.
through the cortex, and they should not be mistaken for a fracture (Fig. 8-9). Nutrient canals are less radiolucent than a fracture and have a characteristic course. Nutrient foramina generally occur at the ends of bones, appearing as a small circular radiolucency, and are seen most commonly at the intercondylar notch of the knee.
Interosseous Ridges
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree