Methods of Examination, Techniques, and Anatomy of the Chest
John H. Juhl
Janet E. Kuhlman
J.H. Juhl and J.E. Kuhlman: Department of Radiology, University of Wisconsin Medical School, Madison, Wisconsin 53792-3252.
METHODS OF EXAMINATION
It is generally agreed that radiographic examination of the chest is extremely important in the diagnosis of pulmonary disease. Its value is equally great in the diagnosis of diseases of the mediastinum and bony thorax. It is a very cost-effective study and is the most frequently performed procedure in most departments. The chest roentgenogram serves as a record of the presence or absence of disease on the date it was taken, and follow-up examinations can determine progress or development of disease. On the other hand, the chest roentgenogram should not supplant the routine physical examination and clinical history, even though it demonstrates lesions that cannot be found in any other manner. It is possible to make positive diagnoses of several conditions on the basis of chest roentgenograms alone; in other instances a lesion is disclosed, the nature of which must be ultimately determined by bacteriologic, cytologic, or other laboratory studies. Cardiovascular disease can also be studied by radiographic and other imaging methods and is discussed in Chapter 35.
RADIOGRAPHY
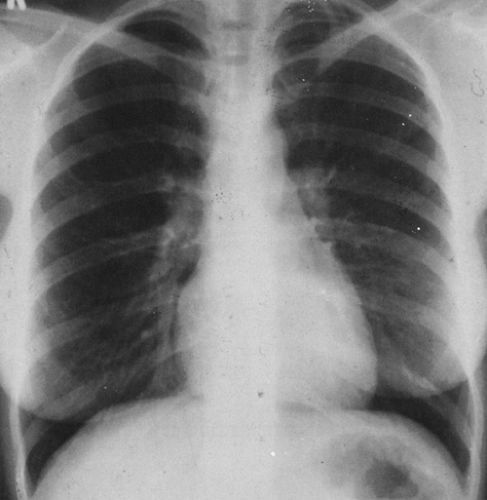
Standard roentgen examination of the chest varies in different institutions but should consist of at least a posteroanterior (PA) and possibly a lateral projection. Most departments include a lateral film in the standard chest examination of patients with suspected thoracic disease, although some studies suggest that its value is limited, particularly in patients younger than 40 years of age.22 It is not cost-effective in routine follow-up or screening studies. The chest radiographs are obtained at a tube-film distance of at least 6 feet to minimize divergent distortion and magnification and are secured in full inspiration. Most radiologists prefer a high-voltage technique (120 to 150 kVp). This permits good penetration and visualization of retrocardiac and mediastinal structures. Chest radiographs taken at a higher voltage (350 kVp) have been used in some institutions. However, there is a difference of opinion as to the advantages of this method,39,77 and it is not generally employed. It is desirable to visualize the upper thoracic vertebral interspaces and to define clearly the vascular markings behind the heart (Fig. 22-1). It is also imperative to obtain films of sufficient penetration to permit identification of retrocardiac disease. Slight overexposure is preferable to underexposure, because viewing in bright light may compensate for overexposure but there is no way to compensate for underexposure. A stationary grid and ionization chamber timing are helpful in obtaining quality films. Fine-line grids do not detract appreciably from film quality but are not necessary when an air-gap technique is used.97 It is advantageous to use copper-wedge filtration of the x-ray beam to secure good mediastinal penetration. Some departments use a tunnel or trough filter for this purpose.
Several other views are used in special circumstances to outline local lesions or to visualize areas that are not well seen on the routine roentgenograms. Oblique projections are obtained at approximately 45° angles and are named according to the side of the chest nearest the film and away from the roentgen-ray tube. For example, the designation right anterior oblique indicates that the patient is standing with the right anterior chest wall in contact with the cassette holder at an angle of 45° so that the left posterior chest wall is nearest the tube; the rays then traverse the thorax from posterior to anterior in an oblique direction. Greater or lesser degrees of obliquity may be used as desired. When small nodules below
the level of the dome of the diaphragm are poorly seen on routine examination, the tube may be angled upward or downward as necessary. Special views may also be obtained tangential to lesions of the thoracic wall to define them clearly.
the level of the dome of the diaphragm are poorly seen on routine examination, the tube may be angled upward or downward as necessary. Special views may also be obtained tangential to lesions of the thoracic wall to define them clearly.
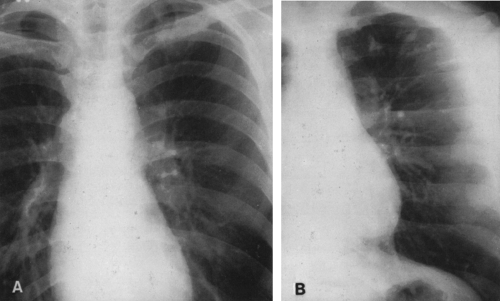
The apical lordotic view is used to see disease in the pulmonary apices, which may be obscured by the clavicle and first rib. This roentgenogram is taken in an anteroposterior (AP) direction with the patient leaning backward on the cassette holder. An AP upright projection with the tube angled cephalad 15° may be used when it is difficult or impossible to obtain a standard apical lordotic view. This is somewhat easier for the patient and is more readily reproducible. This projection results in clear visualization of the lung apices because the clavicle and first rib are projected above the pulmonary apex (Fig. 22-2).
The lordotic projection does cause difficulty in interpreting basal abnormalities because there is an apparent elevation of the diaphragm and poor visualization of basal disease. Also, the aortic arch may be poorly defined, an apparent superior mediastinal widening may be present, the left heart border may be indistinct, and the left hilum is projected caudally and may be hidden by the heart.42 The AP supine view, often used for portable films, may also be taken inadvertently in a somewhat lordotic position. Many of the patients are in intensive care facilities for severe problems and are candidates for basal pneumonia or atelectasis. When the tube is angled in a cephalad direction in these patients, the loss of left diaphragmatic definition may simulate these basal conditions. Care must be taken not to overlook this possibility.116
Lateral decubitus views are sometimes indicated to outline fluid levels in cavities or in the pleural space and to determine the presence of free pleural fluid. The films are exposed with the roentgen-ray beam directed in a horizontal plane and with the patient lying on either the right or left side, as indicated by the PA and/or lateral views. If there is any question of obstructive emphysema (overinflation) involving a lung, lobe, or segment, a film in complete expiration in addition to a film in inspiration is indicated. This combination can also be used to record diaphragmatic motion in conditions affecting the diaphragm on one or both sides.
Stereoscopic roentgenograms are used by some radiologists and are particularly helpful in localizing small, solitary nodular lesions and in studying chronic pulmonary granulomatous diseases, in which pulmonary opacities and cavities at varying depths can more readily be identified. Because there are two films, this method of examination also tends to eliminate the danger of misinterpreting an artifact. An automatic film changer is used, and two films are exposed in quick succession. The patient remains stationary, and the tube is shifted approximately one-tenth of the distance between the anode of the roentgen-ray tube and the film. There is some question as to whether this extra film is necessary and cost-effective, and routine stereoscopic radiographs have been discontinued in most radiology departments. It may be that stereoscopic radiographs are cost-effective in very-high-risk patients for the detection of lung nodules.51
In the air-gap technique described by Jackson,46 a 10-foot distance from the focal spot of the tube to the film is used. The patient is separated from the film cassette a distance of 15 cm by a suitable frame. Moderately high voltages are employed (average of 120 kVp for adults). There is no need for a grid. Jackson prefers to use the AP position. The outstanding advantage is the clarity of vascular markings in the lung.97 Patient exposure to radiation is comparable to that of nongrid techniques and is less than that of grid techniques. The major disadvantage is the additional space required by the longer focal film distance.
Direct magnification is another type of examination. Although used infrequently, it is of particular value in the examination of the chest of the newborn.1 The distance between the object (chest) and the film is increased in this technique, but the focal spot size must be very small (0.3 mm or less) to avoid unacceptable lack of sharpness of the image.
The prone chest film is useful in patients in whom the lung bases are obscured by fluid. Simultaneous frontal and lateral views may be useful in evaluating heart size and lung volumes in infants with respiratory distress.35 An AP view with the tube angled caudad about 30° may be used to define posterior pulmonary lesions obscured by the dome of the diaphragm on standard chest films, but it is seldom used because oblique and lateral films usually suffice. The angle may be altered to fit the situation if this method is used.
Supine radiographs are used extensively, especially in intensive care units, which have increased considerably in size and number in recent years. Technique is a problem, because patients often cannot cooperate very well. Therefore, shorter focal film distances are used; also, optimal equipment may not be available. High-kilovoltage equipment is necessary to obtain good-quality films.
Supine radiographs are used extensively, especially in intensive care units, which have increased considerably in size and number in recent years. Technique is a problem, because patients often cannot cooperate very well. Therefore, shorter focal film distances are used; also, optimal equipment may not be available. High-kilovoltage equipment is necessary to obtain good-quality films.
Newer techniques, such as digitization and processing of x-ray exposures on a special cassette or digital processing of radiographs using a laser scanner, show promise and may turn out to be very helpful in manipulating suboptimal supine films taken with portable equipment.60,61,90 There is now a considerable interest in scanning systems and in production of digital images, directly and indirectly, in order to improve the diagnostic usefulness of chest images.28,76,90 Among the most promising are (1) film digitization; (2) phosphor plates, which are photostimulable.27,60,61; (3) direct digital radiography using a selenium drum detector60,61; and (4) beam equalization radiography.60,61 Advanced multiple-beam radiography (AMBER) uses a filter that is effectively patient-specific.102 The ultimate place of these and other new systems in chest radiography remains to be determined.
Computed radiography (CR), which employs photostimulable phosphor plates, is rapidly gaining clinical acceptance at many institutions, particularly for use in intensive care units for portable chest radiography. In these systems, the patient and a special, reusable photostimulable phosphor imaging plate are exposed to an x-ray beam with the use of currently available conventional portable equipment. The latent image stored on the imaging plate is read out by a laser beam which causes luminescence of the plate. The resulting light signal is captured, amplified, and converted into a digital signal.2,60,61 A variety of image processing algorithms, including exposure recognition and analysis, contrast enhancement, and edge enhancement by unsharp masking, are then applied to the digital information to enhance the image. Optical density of the image is set and adjusted by the computer, which can compensate for overexposure or underexposure. The processed image can then be viewed on one or more video display monitors, recorded on film, and stored electronically, for example on optical disks.60,61
The advantages of CR include its much wider exposure latitude compared with conventional film-screen combinations. CR is particularly useful under circumstances in which exposure is variable and difficult to control, as in portable radiography. CR also has the advantages inherent to all digital imaging systems, including improved image transfer and storage capabilities and improved image manipulation through advanced computer processing.2 However, the spatial resolution of CR images (2.5 line pairs per millimeter) remains less than that achievable by film-screen systems (5 line pairs per millimeter), and CR imaging plates are more sensitive to scattered radiation.61 Newer improvements in CR technology which may prove advantageous include high-resolution CR systems designed for dedicated chest radiography and a dual-energy system that allows generation of a soft-tissue and bone image of the chest.60,61
FLUOROSCOPY
There are several indications for fluoroscopy of the chest; they are discussed under the various conditions for which
fluoroscopy is used. The dynamics of the cardiovascular system and respiration can be studied by this method. Fluoroscopy is also particularly useful in acute obstructive overinflation secondary to aspiration of a foreign body. Air trapping, regardless of cause, can produce mediastinal motion on respiration, which may be more readily apparent fluoroscopically than on films, particularly in children. Conditions affecting diaphragmatic motion are also indications for fluoroscopy of the thorax. Loculated effusions can be localized, if necessary, for thoracentesis. However, ultrasonography is now being used extensively for this purpose and carries no radiation hazard.
fluoroscopy is used. The dynamics of the cardiovascular system and respiration can be studied by this method. Fluoroscopy is also particularly useful in acute obstructive overinflation secondary to aspiration of a foreign body. Air trapping, regardless of cause, can produce mediastinal motion on respiration, which may be more readily apparent fluoroscopically than on films, particularly in children. Conditions affecting diaphragmatic motion are also indications for fluoroscopy of the thorax. Loculated effusions can be localized, if necessary, for thoracentesis. However, ultrasonography is now being used extensively for this purpose and carries no radiation hazard.
Because there are radiation hazards to both patient and physician in the use of fluoroscopy, it is important to reduce radiation to a practical minimum. Image intensification is used to improve visualization and to decrease radiation. It is necessary to have chest roentgenograms available for study and to know as much as possible about the patient’s problem before beginning fluoroscopy. This avoids unnecessary search for a lesion that is much better examined by radiographic methods. It is necessary to use the smallest possible aperture and to limit the total fluoroscopic time in order to reduce radiation exposure. A built-in timer that indicates the duration of radiation exposure is the best method for timing fluoroscopy. We attempt to keep the total fluoroscopic time as low as possible and always less than 5 minutes.
The actual procedure used in fluoroscopy varies with the indication and with the examiner, but the examination should be systematic. For example, diaphragmatic motion is observed during normal and deep inspiration in the oblique as well as in the AP positions; slight weaknesses can often be detected by having the patient sniff. It is sometimes helpful to observe diaphragmatic motion in both lateral decubitus positions to detect small variations in motion on the two sides. Valsalva’s maneuver (forced expiration with the glottis closed) can be used to increase the intrathoracic pressure to empty or decrease the size of veins, cardiac atria, and arteriovenous malformations. Müller’s experiment (forced inspiration with the glottis closed) can be used to decrease intrathoracic pressure and thereby increase the size of these thin-walled vascular structures. At times it is necessary for the patient to be examined while in the supine position, particularly when pleural effusion obscures the diaphragm on one or both sides. Fluoroscopy of the chest is often useful but should be undertaken only when roentgenographic studies do not or cannot answer the questions raised by the clinical problem at hand.
BRONCHOGRAPHY
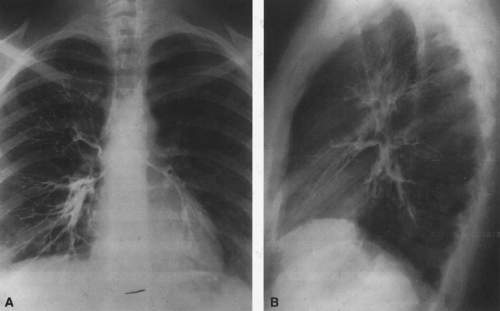
Bronchography is the study of the bronchial tree by means of the introduction of opaque material into the desired bronchi, usually under fluoroscopic control (Fig. 22-3).
At present, bronchography is used rarely, if at all, at most institutions; it is not described in further detail here. Computed tomography (CT), a less invasive method of evaluating the airways, has replaced bronchography for most indications, including the evaluation of bronchiectasis, suspected bronchogenic tumor, and anomalies of the bronchial tree. In addition, direct methods such as fiberoptic bronchoscopy with biopsy, brush biopsy, and percutaneous biopsy permit a tissue or bacteriologic diagnosis that is not obtained with bronchography. Particularly with the advent of helical or spiral CT, the airways can be mapped in great detail and displayed in a variety of CT formats including traditional axial cross-sectional images of the bronchi, reformatted two-dimensional multiplanar images, and three-dimensional shaded surface displays or volumetrically rendered models of the airways (see Fig. 22-5B). CT data can even be used to generate interior views of the central airways similar to the perspective seen during bronchoscopy, so-called virtual bronchoscopy.25,50,94
TOMOGRAPHY
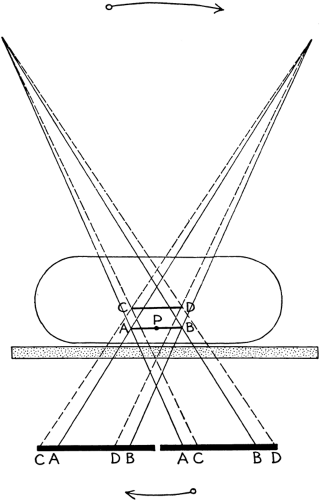
Tomography has been largely replaced by CT but is still used occasionally by some in the study of hilar abnormalities. This is a method of radiographic examination by which it is possible to examine a single layer of tissue and to blur the tissues above and below the level by motion. This is accomplished by simultaneous motion of the roentgen-ray tube and the film cassette during the exposure by means of a connecting rod or bar. The tube and film move in opposite directions, and the fulcrum of the bar or rod connecting the tube and film carrier is placed at the level to be examined (Fig. 22-4). The amount of blurring depends on the distance of the object or tissue from the level of the fulcrum. The thickness of the plane of tissue examined is determined within certain limits by the distance traveled by the tube and film during the radiographic exposure. Zonography is a variation in which the thickness of the plane of tissue examined is increased by shortening the excursion of the tube. By raising or lowering the fulcrum, planes of tissue within the chest can be examined at various levels as desired. Some manufacturers of radiographic equipment also make or distribute attachments for linear tomography. Special tomographic units allowing circular, elliptical, and hypocycloidal motion are also available. These pluridirectional units are preferred to the linear tomographic units,58 because linear tomography does not represent planar anatomy as accurately as pluridirectional tomography. When whole-lung tomography is used, the AP projection is employed. Posterior oblique tomography at a 55° angle is preferred when the hilum is being studied.
There were many indications for tomography of the chest, but standard tomography has been replaced for most of them by CT.
COMPUTED TOMOGRAPHY
CT has become an integral part of the chest radiologist’s imaging armamentarium, and many applications have been
found for its use in the chest.47,89 In the lung it is of value in (1) the evaluation and staging of primary pulmonary neoplasms; (2) the detection of pulmonary metastases from nonpulmonary primary tumors; (3) the characterization of solitary pulmonary nodules as benign or malignant through detection of calcium, fat, and contrast-enhancement patterns87,95; and (4) the characterization of focal and diffuse lung diseases for diagnosis. It is helpful as a means of guidance in needle biopsy when fluoroscopy is inadequate. It is also helpful in the study of cavitary masses, peripheral lung tumors, and pulmonary collapse.
found for its use in the chest.47,89 In the lung it is of value in (1) the evaluation and staging of primary pulmonary neoplasms; (2) the detection of pulmonary metastases from nonpulmonary primary tumors; (3) the characterization of solitary pulmonary nodules as benign or malignant through detection of calcium, fat, and contrast-enhancement patterns87,95; and (4) the characterization of focal and diffuse lung diseases for diagnosis. It is helpful as a means of guidance in needle biopsy when fluoroscopy is inadequate. It is also helpful in the study of cavitary masses, peripheral lung tumors, and pulmonary collapse.
In the mediastinum, CT is useful in the study of causes for mediastinal widening, staging of tumors that spread to the mediastinum (e.g., lymphoma), and characterization of mediastinal masses for diagnosis (i.e., differentiating cysts from solid tumors, vascular from nonvascular lesions, and fatty from nonfatty masses). In patients with myasthenia gravis, it can be used to evaluate possible thymic masses; in hyperparathyroidism it may be helpful in finding adenomas, particularly if they are ectopic and have not been located at surgery.
In the pleura, plaques, masses, loculated fluid, and occult calcification can be localized and the extent determined. In the chest wall, masses involving soft tissue, bone, spinal canal, and adjacent lung can be studied advantageously.
Additional uses include study of trauma involving the pleura, chest wall, mediastinum, and lung. Diffuse pulmonary disease such as emphysema, pulmonary fibrosis, and bronchiectasis can be accurately delineated as to extent with CT. In patients with lung cancer, CT size criteria are used to determine the likelihood of mediastinal node involvement by tumor, but because CT is not tissue specific, malignant involvement must be confirmed by nodal tissue sampling. CT is very useful, however, in mapping the mediastinal nodes for biopsy guidance. In masses adjacent to the mediastinum and chest wall, invasion can be simulated because of lack of tissue specificity.
High-resolution computed tomography (HRCT) makes use of narrow-beam collimation (1- to 1.5-mm slice sections at 10-mm intervals) and a high-spatial-frequency, edge-enhancing algorithm to achieve CT images of the lung parenchyma with improved spatial resolution. Because of the increased visibility of image noise on HRCT images, optimal technique may also require higher kVp/mA settings than conventional CT.107 Indications for HRCT include evaluation of interstitial lung diseases, bronchiectasis, emphysema, and cystic lung disease. Clinical applications include (1) detection of occult lung disease when the chest radiograph is normal or equivocal, particularly in the immunocompromised host; (2) further characterization of known lung disease for diagnosis; (3) accurate localization and quantification of disease extent; (4) determination and monitoring of disease activity, progression, or resolution. HRCT morphologic features of a variety of lung diseases have been described, including HRCT findings in sarcoidosis, idiopathic pulmonary fibrosis (usual interstitial pneumonia), other interstitial lung diseases (e.g., desquamative interstitial pneumonia, scleroderma lung, rheumatoid lung), histiocytosis X, hypersensitivity pneumonitis, lymphangitic carcinomatosis, pneumoconiosis, alveolar proteinosis, lymphangiomyomatosis, bronchiolitis obliterans, mycobacterial infection, pneumocystis pneumonia, pulmonary drug toxicity, emphysema, and bronchiectasis. In many of these disease entities, HRCT is more sensitive and specific than the chest radiograph in detection and characterization for diagnosis as well as for delineation of the extent of disease.108
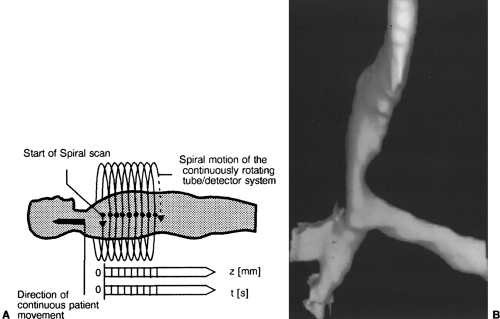
Spiral or helical CT technology is rapidly replacing older-generation CT models. Spiral CT makes use of new slip-ring technology that allows for continuous rotation of tube and detector (Fig. 22-5). This, coupled with multiple consecutive scans of 1 second or less and continuous patient translation through the CT gantry, results in a spiral acquisition of CT data that is then interpolated to generate axial CT images. The spiral acquisition process is much faster than conventional slice-by-slice CT and allows for a volumetric acquisition of data, often in a single breath-hold, which greatly diminishes respiratory artifacts and slice misregistration.18,49,103 As a result, spiral CT is more accurate in the detection of small pulmonary nodules; generates higher-quality, respiratory motion–free multiplanar and three-dimensional images of the chest, airways, and vessels; and allows for more optimal use of intravenous contrast agents in the chest.13,16,17,18,19,40,48,49,72,74,78,82,86,101,113,114,115
ULTRASONOGRAPHY OF THE THORAX
Ultrasonography, particularly real-time scanning, is noninvasive and may be very useful in certain conditions. There is no radiation exposure of the patient. It is used in patients with pleural disease. Fluid can be detected, localized, and differentiated from solid pleural masses and can be removed if necessary using ultrasound guidance. Fluid can also be detected in peripheral lung lesions that are in contact with the chest wall. Mediastinal cysts in contact with the chest wall can be differentiated from solid masses. Several conditions in and near the diaphragm can be detected, localized, and often diagnosed; these include loculated effusion (intrathoracic or subphrenic), hepatic abscess or cyst, and, in some instances, diaphragmatic rupture and hernia.
MAGNETIC RESONANCE IMAGING
Magnetic resonance imaging (MRI) has a limited but growing number of specific applications in the chest. There are several obvious advantages of this modality. First, there is no radiation hazard or other known biologic risk at imaging levels now in use. Second, the images may be obtained without the use of mechanical motion devices and views in multiple planes, including coronal, sagittal, and oblique views, can be acquired directly. MRI also allows for larger field-of-view images to display an overview of the anatomy. Third, intravenous contrast agents are not necessary to identify intrathoracic vascular structures or to show the presence of vascular flow (Fig. 22-6). Fourth, MRI
has a greater ability than CT or plain films to differentiate types of tissues based on signal characteristics. Finally, magnetic resonance angiography is capable of demonstrating some vascular anatomy in a display format comparable to that of conventional angiography, but noninvasively (Fig. 22-6).5,7,9,37,41,63,64,83,92,111
has a greater ability than CT or plain films to differentiate types of tissues based on signal characteristics. Finally, magnetic resonance angiography is capable of demonstrating some vascular anatomy in a display format comparable to that of conventional angiography, but noninvasively (Fig. 22-6).5,7,9,37,41,63,64,83,92,111
MRI also has several disadvantages. First, motion artifacts caused by respiration, cardiac pulsation, and blood flow in the heart and major vessels cause degradation of the images, but these artifacts can be minimized with techniques such as respiratory compensation and respiratory triggering, cardiac gating, and presaturation of inflowing blood. Second, imaging of lung parenchyma is poor with MRI because of the low proton density of the lung tissue and the many air–tissue interfaces that cause loss of signal. Third, patients with cardiac pacemakers, ferromagnetic intracranial aneurysm clips, metal fragments in the eye or near the spinal cord, cochlear implants, and neurostimulators cannot be examined. Fourth, claustrophobia may prevent a small percentage of patients from undergoing an MRI examination. Fifth, biopsy and other interventional techniques require specially designed open scanner equipment, which is currently available only at a few centers. Fifth, the time required for most MRI examinations is greater than for CT scanning. Finally, the cost of MRI is significantly higher than for CT. It is likely that many of these disadvantages will be overcome as technology and instrumentation improve.5,7,9,37,41,63,64,83,92,111
Currently, applications for MRI include the following: (1) assessment of aortic vascular disease, subacute and chronic dissection, vascular anomalies, and venous obstruction of mediastinal and subclavian vessels; (2) cardiac evaluation of selected congenital and acquired heart conditions and pericardial diseases; (3) evaluation of brachial plexopathy including determination of the extent of pancoast tumors; (4) evaluation of the diaphragm and peridiaphragmatic processes; (5) evaluation of intracardiac and paracardiac masses including staging of tumors that may potentially involve the heart, pericardium, or pulmonary arteries and veins; (6) assessment of chest-wall lesions and infections; (7) evaluation of breast implants for rupture and breast masses; (8) evaluation of congenital and developmental anomalies of the pediatric chest such as vascular rings, coarctation of the aorta, lymphangiomas, and sequestrations; (9) determination of the extent of posterior mediastinal masses, especially those with intraspinal extension; and (10) detection of ectopic parathyroid adenomas in the mediastinum.5,7,9,37,41,63,64,83,92,111
PULMONARY ANGIOGRAPHY
Technique
The purpose of this examination is to outline the pulmonary arterial system (Fig. 22-7). This can be accomplished in several ways: (1) injection of contrast material into the superior vena cava with the use of digital subtraction angiography (DSA); (2) injection of contrast material into the right atrium using DSA; (3) direct injection of contrast medium through a catheter placed in a main pulmonary artery; and (4) selective injection of contrast material into a pulmonary artery branch using DSA or balloon-occlusion cineangiography or serial filming.26,33 The nature of the process for which the procedure is performed tends to determine the method used. The advantage of DSA is that a very small amount of iodinated contrast material is necessary. The major disadvantages are artifacts produced by motion and the limited field of view. These may be overcome by the use of dual-energy rather than temporal subtraction and a large-field image intensifier.
Indications
Pulmonary angiography is used in the study of patients with suspected pulmonary arterial or venous anomalies or diseases. Most important is the study of thromboembolic disease of the lungs by means of pulmonary arteriography. The procedure is not used routinely but may be needed when the diagnosis remains in doubt after roentgen and scintiscan studies or when the patient is not responding to treatment for presumed pulmonary embolism. A number of recent studies suggest that spiral CT with intravenous contrast may be a
cost-effective alternative to conventional angiography for the diagnosis of pulmonary emboli proximal to the subsegmental vessels.81,93,98,99,100,110 What role spiral CT will play with respect to ventilation-perfusion scans and Doppler venous studies in the workup of patients with suspected thromboembolic disease remains to be determined and awaits a multi-institutional study along the lines of the original PIOPED study of pulmonary emboli.114
cost-effective alternative to conventional angiography for the diagnosis of pulmonary emboli proximal to the subsegmental vessels.81,93,98,99,100,110 What role spiral CT will play with respect to ventilation-perfusion scans and Doppler venous studies in the workup of patients with suspected thromboembolic disease remains to be determined and awaits a multi-institutional study along the lines of the original PIOPED study of pulmonary emboli.114
BRONCHIAL ARTERIOGRAPHY
Bronchial arteriography requires selective catheterization of bronchial arteries. Its use in pulmonary disease is very limited, but it still plays a therapeutic role in the treatment of selected cases of life-threatening hemoptysis that may be mitigated with bronchial arterial embolization.
PERCUTANEOUS TRANSTHORACIC NEEDLE BIOPSY
This method of examination is used extensively to obtain material for histologic and bacteriologic study. Indications include peripheral lung masses beyond the reach of fiberoptic bronchoscopy8,53 and focal or general pulmonary infections in immunocompromised hosts.104 In the hands of experienced operators, there is a high diagnostic yield and a low incidence of complications. The major complications are pneumothorax and hemorrhage. Pneumothorax usually is easily managed, but hemorrhage occurring after any of the percutaneous procedures can be difficult to manage and has been fatal in rare instances.75 Therefore, these percutaneous procedures are contraindicated in patients with bleeding diathesis or thrombocytopenia, a suspected vascular lesion, recent severe hemoptysis, or severe dyspnea at rest, as well as in those who cannot cooperate.
GENERAL CONSIDERATIONS IN CHEST INTERPRETATION
Interpretation of chest roentgenograms requires that the viewer first find the abnormality. It is useful to develop a method of studying the film to make certain that all areas are searched. The mediastinum, including the heart and great vessels, trachea and central bronchi, lungs, diaphragm, bony thorax, soft tissues of the thorax and neck, and subdiaphragmatic upper abdominal structures should be inspected. It is helpful for the student or trainee to compare the two lungs interspace by interspace until the normal chest is thoroughly understood and variations and abnormalities can be recognized. Once an abnormality is observed, interpretation of the changes follows. We find it valuable to make the initial examination of the film without knowledge of the clinical findings. Before a decision is reached, however, roentgen observations must be correlated with all of the available clinical information. This requires a second study of the film, which has been found valuable in reducing errors. Specific questions may arise, the answers to which may not be available on the chart. Additional information must then be sought from the referring physician or from the patient.
In the chapters on chest roentgenology to follow, the presentation is disease oriented. Patterns of pulmonary opacities of various types are observed. The terms interstitial and alveolar are used to describe the predominant pattern of pulmonary involvement. The terms are not intended to indicate that the pathologic process is necessarily interstitial or alveolar in each instance.
The alveolar or air-space pattern is characterized by homogeneous opacity, which may vary from a small area, just large enough to be recognizable, to consolidation of an entire lobe or more. The alveoli are filled with exudate, transudate, blood, or tissue, which replaces the air. When the lung parenchyma is opacified by some type of fluid, the acinus




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree