The Abdomen
Michael Davis
M. Davis: Department of Radiology, University of New Mexico Health Sciences Center, Albuquerque, New Mexico 87131-5336.
THE ABDOMEN
Multiple options are available for radiologic study of the abdomen. Many, such as the barium enema, are directed at one organ. Plain films, however, allow one to view the entire abdomen before proceeding to a more specific investigation.4
Indications
Abdominal distention, abdominal pain, vomiting, diarrhea, and abdominal trauma are the most common reasons for obtaining plain films. The presence of a palpable abdominal mass warrants imaging by computed tomography (CT) or ultrasonography.7
Normal Abdominal Organs
The liver forms a homogeneous shadow in the right-upper quadrant of the abdomen. Its upper border is limited by the right leaf of the diaphragm, which is confluent with the superior surface of the liver. The superior surfaces of the hemidiaphragms are outlined by aerated lung. The right-lateral margin of the liver is usually separated from the density of the abdominal wall by a thin layer of fat. The lower edge of the right lobe of the liver is seen because of the radiolucency of the adjacent omental and pericolic fat. Gas in the hepatic flexure and in the transverse colon also helps identify the lower margin of the liver. The inferior margin of the left lobe of the liver is not visible. The liver’s complex shape interferes with determining the presence of hepatomegaly until the liver becomes quite large.
The entire spleen or part of it can usually be seen in the left-upper abdomen. The normal spleen, approximately 10 to 14 cm long, is about the same size as the kidney. In rare instances the spleen is unusually mobile and may be found medial to the splenic flexure of the colon.
The kidneys lie on either side of the lumbar spine. Visualization depends on perirenal fat, and their outlines may be lost in patients with markedly diminished body fat. The pancreas cannot be seen on plain films. The outer margins of the psoas muscles can usually be seen because of the fat surrounding them. A loss of body fat or a tapered lateral margin of the muscles may obscure visualization. Less attention is now being paid to the psoas margins in detecting retroperitoneal abnormalities because of the normal variations that exist.8
The lateral margins of the peritoneum often are bounded externally by thin layers of fat sufficient to cause a radiolucent stripe. The three layers of abdominal musculature can be seen lateral to that stripe. The urinary bladder usually is visible if it contains urine and is surrounded by fat. In women the abdominal fat may allow visualization of the uterus.
Supine films may show a mass created by accumulation of stomach fluid in the fundus. When the patient is in an upright position, the gastric fluid shifts to the antrum and the gas to the fundus.
Normal Abdominal Gas
Swallowed air is the source of the gas that is normally seen in the stomach. Some of that gas passes through the small bowel to the colon; it is common to see gas in limited quantities in nondistended small-bowel loops (Fig. 13-1)). The colon normally contains gas and feces, which can be easily recognized. Bacterial gas production has been found to be a significant source of colonic gas. The intestinal gas pattern of infants differs from that of adults in that gas is normally present throughout the small bowel. Within a few hours after birth, gas can be seen throughout the intestinal tract.
Abdominal Calcifications
Calcified mesenteric lymph nodes are observed most often in the right-lower quadrant or in the lower-central part of the abdomen (Fig. 13-2)). Calcification in nodes is believed to be secondary to granulomatous disease. Aortic and arterial calcifications are an almost inevitable consequence of aging and are seen frequently. This calcification often allows estimation of the diameter of the vessel. Aortic and iliac artery aneurysms are the most prevalent and can be confirmed and measured by ultrasonography if necessary (Fig. 13-3)). Venous calcification in the pelvis is very common. These round phleboliths often have a radiolucent center that distinguishes them from urinary tract stones.
 FIG. 13-2. Calcified mesenteric lymph nodes. Calcified nodes are mottled areas of density lateral to the right margin of the third and fourth lumbar vertebrae. |
 FIG. 13-3. Abdominal aortic aneurysm. The diameter of the aneurysm can be measured because of the calcification within the aortic wall (arrows). |
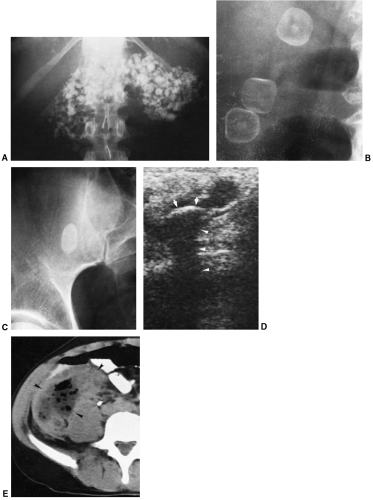
Nodular hepatic and splenic calcifications are seen in people who have lived in endemic areas of histoplasmosis (Fig. 13-4A). Simple splenic cysts often calcify and may be large (Fig. 13-4B, C). The episode that led to the calcification usually cannot be determined. Pancreatic calcification, which is actually pancreatic lithiasis (Fig. 13-5A), occurs secondary to pancreatitis. Most patients with pancreatic calcifications have a history of alcoholism. About 10% of gallstones contain enough calcium to be visible on plain film. Often the calcification is ring-like, and it may be faceted (Fig. 13-5B). Most urinary tract stones are calcified except for nonopaque calculi caused by uric acid, xanthine, or matrix stones. Intestinal contents that remain at one site for too long may calcify, forming fecaliths or enteroliths. There is a strong association of appendiceal fecaliths with acute appendicitis. Rupture of the appendix may allow the fecalith to move freely in the peritoneal space (Fig. 13-5C through E). Enteroliths occur in Meckel’s diverticulum and chronic, partially obstructing lesions of the small bowel and colon. Seed pits may sometimes provide the nidus for the enterolith. Adrenal gland calcification may be a consequence of tuberculosis or of hemorrhagic infarction that occurred when the patient was an infant (Fig. 13-6). Many intra-abdominal cysts, which may calcify, can be found in the spleen, liver, adrenal gland (Fig. 13-7A), kidney, and mesentery. Echinococcal
cysts of the liver calcify, but amebic cysts do not (Fig. 13-7B).
cysts of the liver calcify, but amebic cysts do not (Fig. 13-7B).
 FIG. 13-6. Calcification in the adrenal glands is clearly defined on either side of the first lumbar vertebra. |
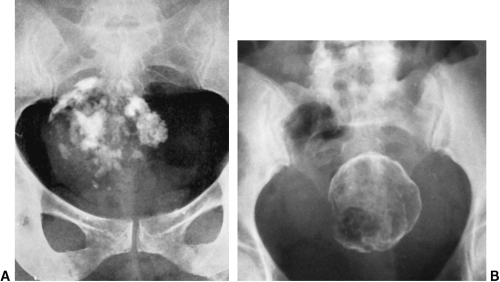
Ovarian teratomas may have calcification within them that simulates teeth and bone. These tumors often contain lipid material as well, which can be identified because of its radiolucency (Fig. 13-8A, B). A tumor that often calcifies is uterine leiomyoma (Fig. 13-9)), whose characteristic mottled “mulberry” calcification occurs as a result of degeneration. Other malignant tumors in the abdomen may also exhibit calcification. The mucin-producing carcinomas of the stomach and colon are an example. Degenerative calcification may occur in renal cell carcinoma. The psammomatous calcification within ovarian carcinomas can occasionally be seen. Neuroblastomas in children frequently contain calcifications.
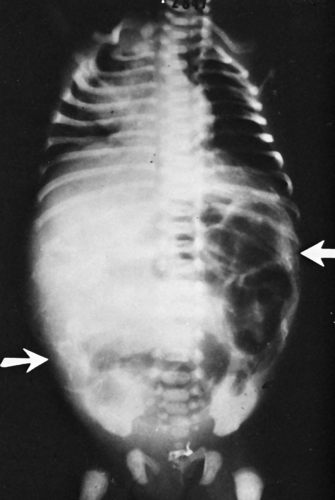
Meconium peritonitis may occur as the result of intestinal atresia or meconium ileus with bowel perforation. In such cases, calcification may be widely distributed throughout the peritoneal space (Fig. 13-10)). Occasionally meconium is calcified while still within the bowel lumen.
Mechanical Small-Intestine Obstruction
Abdominal pain, distention, and vomiting occurring in a patient with a history of previous abdominal surgery direct attention to the possibility of obstruction. A radiographic film of the chest combined with upright and supine films of the abdomen is a good routine to use in evaluating this situation. The upright chest film decreases the possibility of missing perforation of the gut manifested by subdiaphragmatic air and also allows assessment of the status of the lungs. In a simple obstruction, the intestinal lumen is occluded at a single point without any significant interference with its blood supply. Most often an adhesive band is responsible for the obstruction, although a neoplasm, gallstone, or internal hernia may be the cause (Table 13-1).
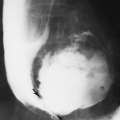
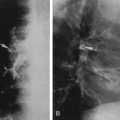
Within 3 to 5 hours after the onset of an obstruction, gas and fluid accumulate proximally and can be seen on the abdominal film. On the upright film, distended bowel loops with gas–fluid levels are present (Fig. 13-11)). In the very early stage or if the obstruction is partial, only a few gas-distended loops may be seen. With the passage of time, the caliber and the number of visible loops increase. The small-bowel loops are distinguished from the colon by their central location in the abdomen and by characteristic small-bowel folds that are close together and extend completely around the circumference of the bowel. This is unlike the colon, where the folds are not circumferential and are widely separated. If the obstruction of the small bowel is complete and enough time has elapsed for colon evacuation, little or no gas may be present in the colon. If the bowel obstruction is incomplete, there may be a normal amount of gas in the colon.
 FIG. 13-11. A: Supine abdomen film shows obstruction with numerous loops of small bowel dilated. B:
Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|