It is imperative for all imaging specialists to be familiar with detailed multiplanar CT anatomy of the paranasal sinuses and adjacent structures. This article reviews the radiologically relevant embryology of this complex region and discusses the region-specific CT anatomy of the paranasal sinuses and surrounding structures. Radiologists also need to know the clinical implications of identifying preoperatively the numerous anatomic variations encountered in this region and prepare a structured report according to the expectations of the referring clinician.
Key points
- •
The radiologist needs to be familiar with the complex sinonasal CT anatomy as visualized by an endoscopic sinus surgeon.
- •
Multiplanar region-specific reporting and preoperative identification of anatomic variants provide the endoscopic surgeon with a useful intraoperative roadmap and avoid intraoperative complications.
- •
This article reviews the CT anatomy of the paranasal sinuses and discusses the clinical relevance of the anatomic variants encountered in the sinonasal region.
But chiefly the anatomy You ought to understand If you will cure well anything That you do take in hand! —John Halle, British Surgeon, 1529–1568
Introduction
Anatomic concepts of the paranasal sinuses have been known since the late nineteenth and early twentieth centuries. These have assumed greater significance in recent times due to advances in functional endoscopic sinus surgery (FESS) and imaging technology. Multiplanar high-resolution CT (HRCT) of the paranasal sinuses provides a precise and reliable preoperative roadmap for the endoscopic sinus surgeon. All radiologists should be familiar with the 3-D anatomy of the paranasal sinuses and the anatomic variants that surgeons are likely to encounter. This article reviews the embryology of the paranasal sinuses and outlines the CT technique/protocols for imaging this region. CT anatomy of the nasal cavity and paranasal sinuses is described in detail together with the anatomic variants encountered in each region.
Imaging techniques and protocol
Preoperative CT imaging of the paranasal sinuses is performed after completion of the medical treatment because up to 80% of patients suffering from acute upper respiratory tract infection show evidence of mucosal disease in the sinonasal region. Intranasal decongestant drops are administered 15 to 20 minutes before commencing the examination and the patient is directed to clear the nasal cavities prior to the scan to clear mucus discharge, which may interfere with the radiologic interpretation. Postoperative CT examinations are performed after a period of 8 weeks once the inflammatory changes have subsided and mucociliary clearance has returned to normal. Table 1 outlines the CT protocols used at the first author’s center for pre-FESS examinations of the paranasal sinuses. All examinations are carried out on a 64-channel CT scanner and viewed on a workstation to facilitate multiplanar reconstructions in standard orthogonal and nonorthogonal planes. Customized low-dose CT protocols are used while scanning pediatric population. Images are reconstructed in soft tissue windows to evaluate structures surrounding the paranasal sinuses (orbits, brain, and nasopharynx) and to document any extra sinus extension of the pathology. Use of cone-beam CT or digital volume CT is advised, if available, to minimize radiation doses in children and young adults.
| Patient Position | Supine |
|---|---|
| Collimation | 64 × 0.625 |
| Reconstruction slice thickness | 0.67 mm |
| Increment | 0.33 mm |
| Reconstruction capability | 0.20 mm |
| Resolution | High |
| Field of view | 180 mm |
| Pitch | 0.641 |
| mA/slice | 200 |
| kV | 120 |
| Rotation time | 0.5 s |
| Filter | Y-sharp |
| Image display matrix | 512 |
All routine pre-FESS CT examinations are performed without the use of intravenous contrast medium. Contrast-enhanced CT or MR imaging examinations are indicated in unilateral pathology, suspicion of neoplastic or vascular pathology, and fungal disease for identifying associated intracranial, intraorbital, and soft tissue extension.
Multiplanar CT evaluation of paranasal sinuses in orthogonal and nonorthogonal planes is important to outline the anatomy and identify surgically important anatomic variants.
Pre-FESS CT examinations of the paranasal sinuses are usually non–contrast-enhanced studies. Contrast examinations are reserved for evaluating specific pathologies (aggressive infections, neoplasm, and vascular lesions) and for assessing extension into orbit, intracranial compartment, and surrounding soft tissues.
Knowledge of relevant embryologic events in paranasal sinus development can avoid pitfalls in diagnosis. Sinus pathologies in children younger than 4 years are uncommon except in the ethmoid sinuses because these are the only sinuses that are pneumatized at birth.
Embryology
The embryo gets its first identifiable head and face between the fourth and fifth weeks of gestational age with a central orifice, called the stomodeum, which is surrounded by the mandibular, maxillary, and frontonasal prominences. The nasal placodes differentiate from the frontonasal prominence and later develop into the nasal cavity and choana. At approximately 25 to 28 weeks of gestation, the ethmoid bone begins to develop from the folding of the cartilaginous olfactory capsule, a central structure in the forming skull base. The ethmoid sinuses that develop within are present at birth whereas the other sinuses (frontal, maxillary, and sphenoid) develop due to pneumatization beyond the confines of the olfactory capsule. Hence, the ethmoid sinus is phylogenetically, anatomically, embryologically, and functionally different from the other air-containing paranasal sinuses. The further ossification pattern is complex and readers are referred to numerous excellent texts in the literature for a more detailed discussion. The pneumatization pattern is unique to each group of sinuses and the continuous change in the size and aeration of the sinus as a child grows has a significant impact on the treatment/surgery of sinus pathology in the pediatric age group. Table 2 outlines the growth pattern of each sinus group and the ostiometal complex with the resultant clinical implications. Fig. 1 depicts the childhood development of the paranasal sinuses and related structures.
| Sr.no | Sinus/Structure | Childhood Development | Clinical Implications |
|---|---|---|---|
| 1. | Frontal sinus | Not seen on imaging at birth Present as a small pit or furrow at birth Slow pneumatization between 1 and 4 y, rapid growth between 4 and 8 y, reaching the orbital roof by 5–7 y of age and attaining adult appearance by 12 y of age Narrower anteroposterior diameter compared with adult | Children cannot develop frontal sinusitis before 4 y of age. Frontal trephination procedures are contraindicated in an immature frontal sinus (until it reaches the orbital plate) due to risk of inadvertent intracranial penetration, meningeal trauma and likely iatrogenic infection. |
| 2. | Ethmoid sinus | Present and seen on imaging at birth Rapid pneumatization between 1 and 4 y Slow growth between 4 and 8 y Adult appearance by 12 y of age | Source of sinus/contiguous orbital infection in young children Accessible to both internal and external drainage procedures if required |
| 3. | Maxillary sinus | Not seen on imaging at birth Present as a shallow rounded sac at birth Rapid pneumatization between 1 and 4 y: floor of the sinus reaches level of the inferior meatus by 7 y of age Adult appearance is attained by 12 and 14 y when the floor of the sinus reaches level of the nasal cavity floor. Slow pneumatization continues until 20 y of age. | Height discrepancy between the inferior margins of the sinus and the nasal cavity precludes the use of certain surgical techniques in children. These procedures may damage developing teeth, cause inadvertent injury to lateral sinus wall, or be ineffective in treating the pathology completely. |
| 4. | Sphenoid sinus | Not seen on imaging at birth. Tiny mucosal sac posterior to the nasal capsule at birth. Pneumatizes between 1 and 3 y of age. Grows progressively between 7 and 14 y and may continue to pneumatize further into adulthood. | Limited clinical significance before the age of 10 y Because the posterior ethmoid sinus pneumatizes earlier, it can grow above the developing sphenoid sinus to form the Onodi cell. Location of critical neurovascular structures around the sphenoid sinus depends on the degree of pneumatization of the sinus. |
| 5. | The ostiomeatal complex | All components are developed and present in the newborn. | All the components of the ostiomeatal complex are packed tightly together leading to a narrow caliber of the infundibulum, which must be appreciated preoperatively. Proximity of the uncinate osseous to the lamina papyracea predisposes to inadvertent intraorbital penetration. |
| 6. | Anterior cranial fossa | The midline structures (crista galli, cribriform plates, and perpendicular ethmoid plate) are cartilaginous at birth and ossify by 2 y of age. They represent the lucent stripe on CT scans of infants as the surrounding ethmoid bone, vomer, and palate are ossified. | The lucent stripe should not be misinterpreted as a bony defect, sinus tract, cephalocoele, or bony destruction. |
Anatomy overview of the sinonasal region
The sinonasal region consists of the nose, nasal cavities, and the paranasal sinuses (frontal, ethmoid, maxillary, and sphenoid). The sinonasal anatomy is discussed in the order of visualization during endoscopic surgery.
The Nose and Nasal Cavities
Fig. 2 depicts the imaging anatomy of the surface of the nose. The nasal cavities are triangular structures separated by the nasal septum in the midline, limited superiorly by the cribriform plate and inferiorly by the hard and soft palate. Lateral walls of the nasal cavities are complex structures that support the inferior, middle, and superior nasal turbinates and, occasionally, a fourth turbinate, known as the supreme turbinate. The middle and inferior nasal turbinates usually have a similar shape exhibiting a convex margin medially and a concave margin laterally. These turbinates divide the nasal cavity into the superior, middle, and inferior meati. The superior meatus drains the posterior ethmoidal air cells and the sphenoid sinus through the sphenoethmoidal recess. The middle meatus drains the frontal sinus via the frontal sinus drainage pathway (FSDP), the maxillary sinus via the maxillary ostium, and the anterior ethmoidal air cells. The inferior meatus drains the nasolacrimal apparatus via the nasolacrimal duct.

The Nasal Cycle
The mucosal lining over the nasal septum and the nasal turbinates is influenced by the nasal cycle, which is responsible for alternating changes in the turbinate sizes due to mucosal engorgement. This cyclic and physiologic enlargement of the turbinates alternates between both nasal cavities every 45 minutes to 1 hour and should not be mistaken for pathology.
The nasal septum
The nasal septum consists of an anterior cartilaginous component (the septal cartilage) and a posterior bony component (the bony septum) comprising the vomer and the perpendicular plate of the ethmoid.
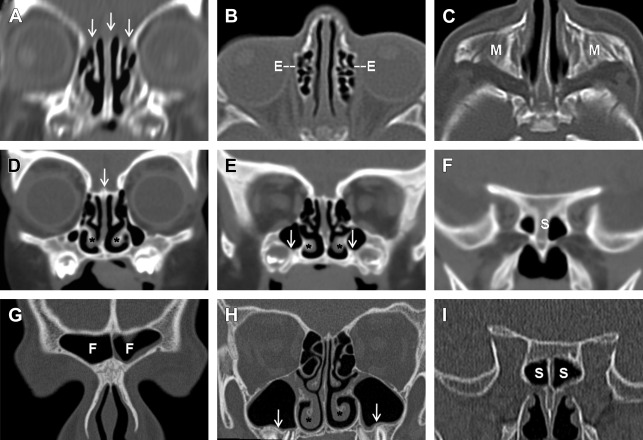
Anatomic variations and the implications ( Fig. 3 ):
- 1.
Septal deviation: Seen in 20% to 79% of the population. The septum is commonly deviated in its inferior portion near the chondrovomeral junction and can also assume an S-shaped configuration with an undulating deviation onto both sides of the midline. Gross septal deviations can displace the middle turbinate and interfere with surgical access to the middle meatus. Septal deviations must be addressed to improve surgical exposure.
Septal spurs may be associated with septal deviations and may form adhesions with the adjacent turbinates.
- 2.
Septal pneumatization: pneumatization may occur anteriorly from the crista galli or posteriorly from the sphenoid sinus. Posterior septal pneumatization may occasionally narrow the sphenoethmoidal recess and impede access to the sphenoid ostium.

The middle turbinate
The middle turbinate is a part of the ethmoid bone with attachments in all 3 planes (ie, sagittal, coronal, and axial). The anterior part of the middle turbinate is oriented vertically and is attached superiorly to the anterior skull base at the lateral border of the cribriform plate. Posteriorly, the attachment becomes oblique attaching to the lamina papyracea and further posteriorly lies in a coronal plane attaching to the medial wall of the maxillary sinuses ( [CR] ). The obliquely directed midportion of the middle turbinate is known as the basal lamella, which is a surgical landmark marking the division between the anterior and posterior ethmoidal sinuses.
Anatomic variants and the implications ( Fig. 4 ):
- 1.
Concha bullosa: pneumatization of the inferior bulbous portion of the middle turbinate occurs in approximately 24% to 55% of the population and is usually bilateral. If the pneumatization is restricted to the vertical lamella of the turbinate above the level of the ostiomeatal unit, it is termed an interlamellar cell of Grunwald, lamellar bulla, or conchal neck air cell. This cell generally does not disturb sinonasal physiology. A large concha bullosa may cause septal deviation and obstruct the ethmoidal infundibulum.
- 2.
Paradoxic middle turbinate: in 26% of the population, the middle turbinate exhibits a paradoxic lateral convexity, which can impede surgical access to the ostiomeatal unit and contribute to recurrent rhinosinusitis.
- 3.
Turbinate sinus: occasionally the inferior portion of the middle turbinate curves acutely on itself producing a deep invagination called a turbinate sinus.
- 4.
Pneumatized basal lamella: may be mistaken for an anterior ethmoidal air cell leading to incomplete exploration of the posterior ethmoid sinuses.

Lamellar anatomy
Lamellae are organizational plates, which develop within the cartilaginous olfactory capsule. They are important surgical landmarks and partition the sinonasal cavity into well-defined compartments. The lamellae course through the ethmoidal air cells and extend superiorly up to the skull base from the lateral nasal wall. These structures are best seen in the parasagittal planes ( Fig. 5 ) and from anterior to posterior include the uncinate process, anterior margin of the bulla ethmoidalis, lamella of the middle turbinate (basal lamella), lamella of the superior turbinate, and, if present, the lamella of the supreme turbinate. If the supreme turbinate is absent, the anterior face of the sphenoid sinus is considered the fifth lamella.

Anatomic variants and the implications:
- 1.
The lamellae may be displaced, distorted, remodeled, or attenuated by a variety of disease processes. Visualization of intact lamellae indicates, however, a benign pathology in most cases. The lamellae are destroyed or eroded by malignant neoplastic lesions or aggressive infective pathologies like invasive fungal disease.
- 2.
The fifth lamella is not identified in case of a nonpneumatized sphenoid sinus.
- 3.
The suprabullar and retrobullar recesses can be identified while viewing the lamellar anatomy in the sagittal plane.
The uncinate process
The uncinate process is a thin crescent-shaped bone, which runs in a sagittal plane from anterosuperior to posteroinferior. It is attached anteriorly to the lacrimal bone and inferiorly to the ethmoidal process of the inferior turbinate as well as to the perpendicular process of the palatine bone. Posteriorly the uncinate has a free concave margin. The superior attachment of the uncinate process may be variable. On coronal CT scan, the space between the uncinate process and the medial wall of the orbit denotes the ethmoidal infundibulum.
Anatomic variants and the implications:
- 1.
Variable attachments: the uncinate process may attach superiorly to the lamina papyracea, the anterior skull base, or the middle turbinate and may also have multiple attachments to these structures. The pattern of attachment determines the position of the FSDP ( Fig. 6 , Table 3 ).

Fig. 6
Coronal CT images showing unicate process attachments. ( A ) Left uncinate process (UP) attached to lamina papyracea ( arrow ) with the FSDP ( dashed lines ) draining into the medial meatus (MM). ( B ) Right uncinate process attaching to the middle turbinate ( arrow ) with the FSDP ( dashed lines ) draining into the ethmoidal infundibulum (EI). RT, recessus terminalis.
Table 3
Pattern of superior attachment of the uncinate process
Lamina papyracea
Seen in more than 50% of individuals, resulting in a medial FSDP draining into the middle meatus, creating a blind pouch laterally termed the recessus terminalis
Anterior skull base
Results in a lateral FSDP opening into the ethmoidal infundibulum, increasing chances of retrograde spread of infection into the frontal sinus from the ethmoidal sinus
Middle turbinate
FSDP is displaced posterior to the agger nasi cell, which needs to be fractured to access the FSDP.
- 2.
The uncinate process may be pneumatized ( Fig. 7 A ) in 4% of the population or everted. A pneumatized uncinate process (uncinate bulla) can narrow the infundibulum and impair normal sinus ventilation. An everted uncinate process may be mistaken for a double middle turbinate on endoscopy.