Normal Variants
Skeletal variants, anomalies, and defects are often seen during plain film interpretation. A general understanding of their presentation and appearance is important because many appear similar to more aggressive pathologic disease states and traumas. Thus, successfully identifying a normal variant saves time, effort, and expense.
Tables 7-1 through 7-7 list selected variants, anomalies, and other defects by region. The selected entries are not intended to represent an exhaustive list. Entire textbooks have been dedicated to normal variants and the reader is directed to those textbooks (see, e.g., Keats TE: Atlas of normal variants that may simulate disease, St. Louis, 2001, Mosby; Schmidt H et al: KÖhler/Zimmer Borderlands of the normal and early pathologic in skeletal pathology, New York, 1993, Thieme Medical).
TABLE 7-1
SKELETAL VARIANTS, ANOMALIES, AND DEFECTS OF THE SKULL
| Variant/Artifact | Comments |
| Artifacts (Figs. 7-1 and 7-2) | Common artifacts visualized are hearing aids, hairpins, dental fillings, etc. |
| Arnold-Chiari malformation | Arnold-Chiari malformation describes the presence of a myelomeningocele with varying degrees of caudal displacement of the cerebellar tonsils and hindbrain. It is discussed more fully in Chapter 33. |
| Basilar invagination (Fig. 7-3) | Basilar invagination describes a cephalic deformity of the margins of the foramen magnum with resulting deformity of the condyles and skull base (basilar impression). Although some authors separate the upward displacement of the foramen magnum (basilar invagination) from the resulting deformity of the skull base (basilar impression), most sources use the terms as synonyms. The presentation is either primary6 (congenital syndromes such as Klippel-Feil syndrome and Arnold-Chiari malformation) or acquired (bone softening pathologies such as osteomalacia, fibrous dysplasia, or Paget disease). Primary basilar impression is also known as Bull-Nixon syndrome. The deformity is identified on lateral projection by constructing lines from the posterior extreme of the hard palate to either the posterior margin of the foramen magnum (Chamberlain line) or lower margin of the base of the occiput (McGregor line), and examining the distance between that line and the tip of the odontoid process.x (See Chapter 4 for more detail on construction of these roentgenometrics.) In contrast to describing the relationship of the odontoid to the skull base, as is done for basilar invagination, the term platybasia (meaning “flat base”) describes the morphology of the skull base without using the odontoid as a reference point. Platybasia is assessed by constructing approximations of the hard palate and clivus. If the resulting angle (the Martin basilar angle, see Chapter 4) is greater than 152 degrees, platybasia is present. Basilar impression increases the risk of neurologic damage and circulatory embarrassment. |
| Cerebral falx calcification | A calcified cerebral falx appears as a single sheet of calcification extending from the frontal bone. It is related to infection, trauma, or normal aging. A multiple layer (lamellar) appearance of calcification is seen in Gorlin syndrome. |
| Choroid plexus calcification | Calcification of the choroid plexus is one of the most common normal intracranial calcifications, nearly always occurring in the lateral ventricles. It appears as a stippled pattern of calcification located immediately superior to the orbits on a frontal projection and slightly superior and posterior to the pinna of the ear on the lateral film. Usually beginning after age 20 years, it should be differentiated from the punctuate cortical and linear basal ganglia calcifications associated with toxoplasmosis. |
| Dermoid | Dermoids are small (<1 cm), midline, well-marginated, radiolucent defects of the skull, representing a congenital inclusion of ectoderm, mesoderm, and endoderm. |
| Digital impressions | Digital impressions are shallow, broad grooves on the inner table of the skull corresponding to the adjacent cerebral gyri. They are most often found between 4 and 8 years of age, typically in the parietal bone of children and in the squamous portion of the temporal bone when in adults. Craniosynostosis may cause accentuation of the local digital impressions. In children older than age 1 year, an absence of digital impression suggests underdevelopment of the cerebrum.87 |
| Doughnut lesion | A doughnut lesion is a small (<1 cm) radiolucent defect with well-defined surrounding sclerosis and often a central calcification. They are normal variants of little clinical significance and are differentiated from the more clinically relevant button sequestrations by the absence of reported pain and disability. |
| Dural venous sinus (Fig. 7-4) | A radiolucent defect may be seen in the skull corresponding to the dural venous sinus. |
| Emissary veins | Emissary veins are normal conduits connecting dural venous sinuses to extracranial venous pathways. Their foramina may appear on radiographs of the skull as unilateral or bilateral radiolucent defects, typically in the frontal, parietal, and occipital bones. Their enlargement suggests elevated intracranial pressure or dural arteriovenous malformation. |
| Empty sella syndrome | Empty sella syndrome is a small, flattened, or absent pituitary gland within a usually (see Fig. 16-8 in Chapter 16) enlarged sella turcica. It is caused by a congenital (primary) or acquired (secondary to trauma, surgery, radiation, etc.) defect of the diaphragm sellae that allows an intrasellar extension of the suprasellar arachnoid space. Pulsations of the cerebrospinal fluid are thought to cause enlargement of the sella turcica and compression of the pituitary gland. Secondary empty sella syndrome is common among women who are overweight or have high blood pressure. Symptom expression is highly variable and may include headache, galactorrhea, hyperprolactinemia, dysmenorrhea, visual disturbance, and runny nose. Usually the pituitary function is normal. Primary empty sella syndrome typically is an incidental finding on radiologic imaging of the brain. Patients are usually without symptoms, and pituitary function usually is normal. Rarely, primary empty sella syndrome presents with abnormal facial features, short stature, highly arched palate, and osteosclerosis. Plain film findings demonstrate an enlarged sella turcica (width >16 mm, r depth >12 mm). Computed tomography (CT) and magnetic resonance imaging (MRI) demonstrate a small or absent pituitary gland. |
| Encephalocele | An encephalocele is the extension of intracranial tissue through a cranial defect. Typically, the defect is congenital. Encephaloceles are most common in the occiput, and may be supratentorial or infratentorial. Ultrasound is used for antenatal evaluation. MRI will expose the type and extent of the lesion. Encephaloceles may be associated with Meckel-Gruber syndrome, microcephaly, cystic dysplastic kidneys, and polydactyly. |
| Frontal sinus hypoplasia (Fig. 7-5) | The frontal sinuses commonly lack symmetry (hypoplasia), or are missing on one or both sides (aplasia). Rarely, hypoplasia of the frontal sinuses presents with sinusitis, bronchiectasis, and situs inversus; together, this latter triad is known as Kartagener (dyskinetic cilia) syndrome. |
| Habenular calcification | Habenular calcification appears as a characteristic C-shaped or comma-shaped radiodensity noted on plain film and often seen on CT scans. It is of no clinical significance and is differentiated from pineal gland calcification by its smaller size and C-shaped configuration. |
| Hyperostosis frontalis interna (Fig. 7-6) | Hyperostosis frontalis interna is an idiopathic thickening of the internal table of the frontal (enostosis cranii) bone. It progresses slowly over time in a bilateral fashion, but spares the midline. The condition is most common in women older than 40 years of age. It is not uncommon for the condition to spread to proximate regions of adjacent bones. If other bones are extensively involved, the term hyperostosis interna generalisata is used. Morgagni-Stewart-Morel syndrome describes the combined presentation of hyperostosis-frontalis interna, obesity, and hirsutism and virilism. |
| Lacunar skull | Lacunar skull (Lückenschädel, craniolacunia) describes an appearance of multiple radiolucent areas of calvarial thinning seen in newborns and infants. The appearance may be seen in association with meningoceles, encephalocele, or Arnold-Chiari malformations. The appearance may lessen or completely resolve within a few years. It is not analogous to the normal cortical sulcal impressions (digital impressions; see the preceding) that are a feature of young children. Also, lacunar skull is in contrast to the “beaten silver” appearance seen with increased intracranial pressure. |
| Lenticular calcification (Fig. 7-7) | The lens of the eye may calcify as a consequence of injury, inflammation, or old age. It appears as a ring or semicircular shadow in the orbit.48 Calcifications larger than 1 cm may represent vitreous calcifications.84 |
| Metopic suture | The two halves of the frontal bone fuse by 3 years of age. Less than 10% of individuals may demonstrate a persistent frontal (or metopic) suture. Trigonocephaly refers to premature closure of the frontal suture resulting in a triangular forehead with pinching of the temples laterally. |
| Occipital vertebra (Fig. 7-8) | Uncommonly, a portion of the caudal occipital somite or cephalic cervical somite detaches, forming a separate ossicle positioned between the occiput and atlas. If the ossicle is located anteriorly between the anterior tubercle of atlas and the occiput, it is termed a proatlas ossicle. These ossicles usually are of no clinical significance. |
| Occipitalization of atlas (Fig. 7-9) | Also known as assimilation of atlas or occipitocervical synostosis, this anomaly arises from a defect of formation of the most caudal occipital somite resulting in partial or complete fusion of the atlas to the base of the occiput. Occipitalization is the most cephalic example of congenital blocked segmentation. The radiographic features are marked by decreased space between the atlas and the occiput. On sagittal plane flexion and extension radiographs, an occipitalized atlas demonstrates a consistent atlantooccipital space, instead of the typical enlargement of the atlantooccipital space during cervical flexion and narrowing of the same space during cervical extension. Magnetic resonance imaging provides an assessment for the extent of neurologic involvement. When presenting as an isolated phenomenon, occipitalization of atlas generally is viewed as clinically insignificant, although accompanying defects of the transverse atlantal ligament may make stress radiography prudent, especially if congenital blocks of other cervical vertebrae are found. Occipitalization has been associated with limited range of motion, vertigo, unsteady gait, paresthesias, more severe neurologic finding, and even death.90,91 Also, occipitalization of atlas may occur with Klippel-Feil syndrome, platybasia, Goldenhar syndrome, and Sturge-Weber syndrome. |
| Pacchionian granulations | Pacchionian granulations are multiple, nearly circular, smooth, radiolucent, usually symmetric, parasagittal erosions of the inner table of the skull. They are common in the frontal bone and generally of no clinical significance. |
| Paracondylar processes (Fig. 7-10) | A paracondylar process originates from or adjacent to the occipital condyle and extends inferiorly to or near the transverse process of the atlas. It is of little clinical significance, unless significant synostosis between the atlas and occiput exist that limits range of motion across the occipitoatlantal joint.44,57 It is differentiated from an epitransverse process that arises in the opposite direction, from the transverse process of the atlas and extends superiorly to the occiput. |
| Parietal foramina | Parietal foramina are variants presenting as well-marginated, symmetric, parasagittal, radiolucent defects, representing passageways for emissary veins. |
| Petroclinoid ligament calcification (Fig. 7-11) | With calcification the petroclinoid ligaments appear as a horizontal, linear radiodense structure running from the dorsum sella to the petrous portion of the temporal bone, although commonly only the dorsum sella portion of the ligament actually calcifies. |
| Pineal gland calcification (Fig. 7-12) | Calcification of the pineal gland is present in up to one-half of all adults and is a common finding on the lateral projection of the skull; it is even more common on CT scans of the region. Pineal calcification usually is without clinical significance; however, in children the finding is more significant, at times suggesting the presence of neoplasm. The calcification may appear amorphous or homogenously radiodense, typically measuring 3 to 5 mm in size. Pinealoma is suggested by size greater than 1 cm. Displacement of the calcified pineal gland from its typical midline position, as noted on a frontal projection, is an indirect sign of a space-occupying lesion within the skull.29 |
| Stylohyoid ligament ossification (Figs. 7-13 and 7-14) | Approximately 4% of the general population demonstrates elongated styloid processes and calcification of the stylohyoid ligaments, usually representing nothing more than an anatomic variant. However, in rare cases (estimated prevalence of 0.2% to 0.4%) the stylohyoid ligament thickens and ossifies, creating a more clinically relevant presentation (known as Eagle syndrome) as the enlarged structure compresses the external carotid artery, producing pain in the orbit and temporal region.68 The ossification may result from persistence of a cartilaginous anlage. Associated symptoms include foreign body sensation in the throat, dysphagia, and intermittent facial pain.5 Surgical consultation may be advised if related symptoms are identified. |
| Wormian (intrasutural or suture) bones (Fig. 7-15) | Wormian bones are small, irregular islands of bone located within sutures of the skull. The lambdoidal, posterior sagittal, and tympanosquamosal sutures are most often involved. They may regress into the adjacent bone over time. They commonly represent nothing more than a normal variant. Chapter 16 summarizes the diseases associated with wormian bones. |
TABLE 7-2
SKELETAL VARIANTS, ANOMALIES, DEFECTS, AND ARTIFACTS OF THE CERVICAL, THORACIC, AND LUMBAR SPINE
| Variant/Artifact | Comments |
| Atlas | |
| Agenesis of the anterior arch of the atlas (Figs. 7-16 and 7-17) | Agenesis of the anterior arch of the atlas has rarely even been reported. Hypoplasia of the anterior arch is relatively more common but remains rare. |
| Agenesis of the posterior arch of the atlas (Figs. 7-18 and 7-19) | The posterior arch of the atlas begins to form from a secondary center of ossification during the second year of life, completely forming by the age of 3 or 4 years. Although typically viewed as a normal variant, there is a potential for an associated defect of the transverse atlantal ligament, warranting flexion-extension radiographs in those affected. Enlargement of the C2 spinous process (megaspinous of C2) or enlargement of the anterior tubercle of atlas may be accompanying defects of agenesis of the posterior arch of the atlas. The latter is believed to be a stress response to the undeveloped portion of the atlas. |
| Atlantoaxial pseudojoint | Uncommonly, the posterior tubercle of the atlas approximates the superior margin of the spinous process of C2. The resulting frictional sclerosis has been referred to as a pseudojoint or Baastrup disease of the cervical spine. Baastrup disease is more common in the lumbar spine, and is associated with degenerative reduction of the disc height with resulting approximation of the spinous processes. |
| Down syndrome | Approximately 6% to 20% of those with Down syndrome demonstrate laxity of the transverse atlantal ligament and the ligaments from the lateral masses of the atlas to the occipital condyles,98 jeopardizing the stability of the upper cervical spine and possibly resulting in irreversible spinal cord damage. Chapter 8 further discusses this presentation. |
| Epitransverse process (Figs. 7-20 and 7-21) | An epitransverse (supratransverse) process arises from the superior aspect of the transverse process of the atlas and extends superiorly to or near the occiput.44,57 It is of little clinical significance unless significance synostosis between the atlas and occiput exists that limits range of motion across the occipitoatlantal joint. It is in contrast to a paracondylar process, which arises near or at the occipital condyle and extends inferiorly to the transverse process of the atlas. |
| Increased atlantodental interval (Figs. 7-22 and 7-23) | The atlantodental interval (ADI) defines the joint space created by the posterior surface of the anterior tubercle of the atlas and the anterior margin of the odontoid process. Normally the space measures less than 3 mm in adults, and, because of their greater joint laxity, less than 5 mm in children. Enlargement of the ADI indicates joint instability secondary to trauma, inflammatory joint disease, congenital defect, and so on. (See Chapter 17 for a more detailed differential list.) As a normal variant, the ADI may appear V-shaped, opened superiorly. In such cases, the lower margin of the joint should be used as a reference to measure the joint space. Sagittal plane flexion–extension radiographs may be used to stress the joint on equivocal cases of instability. |
| Posterior ponticle of the atlas (Figs. 7-24 and 7-25) | A posterior ponticle (also known as ponticulus posticus, foramen arcuale, Kimmerle anomaly, or Kimmerle variant) represents a small bridge of bone arching over the arcuate rim of the atlas (forming an arcuate foramen). Although traditionally attributed to ossification of the anterior margin of the atlantooccipital membrane, some believe it to represent well-organized bone formed from a distinct ossification center.77 It is seen in approximately 15% of the general population and often is bilateral. It is more common among women when it presents as a partial bridge of bone, and more common in men as a complete bridge of bone between the lateral mass and posterior arch.94 Although controversial, it is generally felt to be a variant of normal. Associations with headaches, Barr-Liéou syndrome, photophobia, and migraine have been reported.3,14 Given that the vertebral artery passes through the defect, there is some concern about ischemia of the posterior cerebral circulation. Posterior ponticles are visualized on lateral or oblique cervical projections. Rarely, a lateral variation, known as lateral ponticle, is seen on the anteroposterior open-mouth projection as an osseous bridge from the superior-lateral margin of the lateral mass of atlas to the lateral portion of the transverse process of the atlas. |
| Spina bifida occulta (Fig. 7-26) | Spina bifida is a generalized term for congenital posterior midline defects of spine, alternatively known as spinal dysraphism, spondyloschisis, posterior rachischisis, or neural tube defects. Approximately 5% to 10% of the general population may have spina bifida occulta, the mildest form of midline defect. Spina bifida occulta usually is clinically insignificant; rarely (<0.1%), however, it may be associated with symptoms and other anatomic findings such as spinal lipomas, syringomyelia, and diastematomyelia. Rarely, spina bifida occulta is associated with cervical spondylolisthesis, usually at C6. Spina bifida occulta is most common to the posterior arch of atlas or vertebral arch of S1, presenting as missing spinolaminar lines on lateral radiographic projections and as incomplete fusion of the posterior arch on the frontal projections. Chapter 8 offers a complete discussion of this condition. |
| Axis | |
| Odontoid process agenesis (Fig. 7-27) | Rarely, a defect of ossification of the odontoid will result in an absent (agenesis) or small (hypoplasia) odontoid process of C2. Resulting instability of the atlantoaxial joint causes concern for spinal stenosis and spinal cord insult. Sudden death has been reported secondary to minor trauma. Atlantoaxial instability is more common among those with Down syndrome, Klippel-Feil syndrome, and skeletal dysplasias. The defect is well visualized on APOM (anterior-to-posterior open-mouth) view. CT offers definitive evaluation. |
| Os odontoideum (Figs. 7-28 to 7-31) | Persistence of the odontoid synchondrosis leads to the formation of a separate odontoid bone (os odontoideum) instead of a normally united odontoid process. The underlying mechanism of the defect is disputed, with both developmental51 and acquired33 etiologies proposed. It is a clinically significant defect, increasing cord pressure related to atlantoaxial instability. The defect is well visualized on the anteroposterior open-mouth projection, and noted to a lesser extent on the lateral cervical projection. See Chapter 8 for complete discussion of the os odontoideum. |
| Os terminale (Figs. 7-32 and 7-33) | The tip of the odontoid process forms from a secondary center of ossification that presents at 3 years of age and fuses to the odontoid process by age 12 years. Rarely, the tip of the odontoid fails to unite, creating an os terminale (also known as a Bergmann defect). It should not be mistaken for a fracture, which demonstrates irregular margins, or an os odontoideum, which occurs lower. On the APOM view, the os terminale appears as a smooth-bordered round, oval, diamond-shaped ossicle separated from and cephalic to the odontoid process. |
| Pseudosubluxation of C2 | Typically, significant vertebral misalignment raises concerns for trauma, advanced degeneration, and instability. However, in children and teenagers younger than age 15 years, it is common to see significant anterolisthesis of 2 mm or more at C2 on C3 (and less common at C3 on C4) without any signs of trauma or degeneration. The finding is believed to be the result of immature muscles and other connective tissues present in the young. Pseudosubluxation of C2 is seen only on lateral cervical projections that demonstrate a neutral or flexion position of the cervical spine. Pseudosubluxations tend to resolve with cervical extension. This helps differentiate a pseudosubluxation from a true injury of the upper cervical spine with resulting anterior displacement of C2 (e.g., hangman fracture). However, caution should be applied to avoid patient extension among those demonstrating significant indicators of fracture. Computed tomography is helpful in such cases. Also, the Swischuk line may be useful to differentiate pseudosubluxation from true injury. This line is drawn along the anterior margin of the posterior tubercle of C1 to the posterior aspect of the posterior arch (spinolaminar line) of C3. The posterior aspect of the posterior arch (spinolaminar line) of C2 should be within 1 to 2 mm of the Swischuk line. A true subluxation is indicated by posterior deviations of more than 2 mm and pseudosubluxation by deviation less than 2 mm.95 |
| Spina bifida occulta (Fig. 7-34) | Spina bifida occulta is a small midline defect, sometimes occurring at C2. Spina bifida occulta is described in greater detail in the atlas or lumbar entries of this chapter, as well as in Chapter 8. |
| Agenesis of the pedicle (Figs. 7-35 to 7-40) | Aplasia of the pedicle is uncommon, representing a unilateral developmental defect of the cartilage anlage dedicated to forming one half of the posterior arch of the vertebrae. Empiric evidence suggests that congenital absence is more common among males and at the L4 vertebrae.93 In the cervical spine, it is seen in decreasing prevalence at C6, C5, C4, and C7. Because aplasia interrupts the structural integrity of the posterior arch, spondylolisthesis may result from this defect. This is a classic finding at C6. The missing pedicle shadow is best seen radiographically, on the oblique projection, but is well demonstrated on the frontal radiograph. In adults, congenital agenesis often presents with an enlarged, radiodense contralateral pedicle, an appearance specific to the condition of aplasia. This is not typically the case among infants and children. If present, the enlarged radiodense contralateral pedicle may provide sufficient proof that the missing pedicle is associated with a congenital etiology as opposed to the more clinically relevant possibility of osteolytic bone disease. Metastasis or multiple myeloma (“winking owl” sign) should be of immediate concern in adult patients. Pathologic destruction of the pedicle by tumor, infection, or erosion seen with neurofibromatosis is not typically associated with hypertrophy or sclerosis of the opposite pedicle. If both pedicles are missing (“blind vertebra”), aggressive bone disease is clinically assumed until proved otherwise. Also, the vertebrae and lamina generally are not affected by developmental aplasia of the pedicle, where aggressive bone disease often has associated bone changes. Wilkinson syndrome describes a sclerotic pedicle with a contralateral pars defect. |
| Artifacts (Figs. 7-41 and 7-42) | Miscellaneous radiodense foreign objects, surgical implantations, and other features may be present in the field of view. Some of these may include central venous port, tantalum mesh/hernia repair, portal stents, Pepto-Bismol in the stomach, gastric bypass staples, umbilical rings, gall bladder surgery, renal surgery, abdominal aorta surgery, Greenfield-Kinney filter, and too many others to fully list. Overlying anatomy may also mimic the appearance of disease. |
| Baastrup phenomenon (kissing spines) (Figs. 7-43 and 7-44) | Baastrup phenomenon, also known as kissing spines, refers to the approximation and resulting pseudoarthrosis of two or more spinous processes. It occurs secondary to intervertebral disc and posterior joint arthrosis but is also related to increased lumbar lordosis. The pseudoarthrosis is marked by a radiodense sclerotic zone subadjacent to the articulating portion of the spinous processes. In some patients, it may be a source of regional pain. Although it is most common in the lumbar spine, a similar frictional sclerosis has been noted between the posterior tubercle of the atlas and the spinous process of C2. |
| Block vertebra (Figs. 7-45 to 7-55) | Block vertebra describes a union between adjacent segments. It can be the result of congenital nonsegmentation of vertebral somites during the third to eighth fetal week of life or from acquired causes, such as infections and surgery. A congenital block vertebra can occur anywhere in the cervical, thoracic, or lumbar region, but is most common to the C2-3 and C5-6 levels. Although several contiguous segments may be involved, usually only two vertebrae are affected. The intervening intervertebral disc may be missing or rudimentary in both a vertical and horizontal dimension, the latter producing a narrowed waist at the junction of the fused segments. Very often the posterior arches of the segments are also fused and the corresponding intervertebral foramina appear prominent. |
| Butterfly vertebra (Figs. 7-56 to 7-59) | This anomaly describes a persistent midline sagittal cleft of the vertebra body. When viewed from the frontal plane, the separated halves of the vertebra appear like butterfly wings, or the full vertebra, like a sideways hourglass. Commonly seen is a slight triangular-shaped elevated area of bone that extends from the adjacent endplate of the normal segments above and below the butterfly defect that fits into the sagittal cleft of the anomalous segment. Disagreement exists over whether the configuration is an ossification defect of the right and left primary growth centers of the vertebral body, or results from a failure of notochordal regression. A butterfly vertebra is typically an isolated phenomenon and is of minor clinical significance. |
| Carotid calcification (Fig. 7-60) | Calcification of the carotid vessel is often seen as an age-related phenomenon. However, vessel calcification does play a role in the development of atherosclerosis. Therefore, when present, a review of the patient’s history should exclude clinical features of obstructive vessel disease. Severe calcification, especially in the area of the carotid siphon, correlates to vessel stenosis. |
| Cervical ribs (Figs. 7-61 and 7-62) | Cervical ribs are supernumerary ribs arising from cervical vertebrae. Approximately 1% of the population demonstrates radiographic evidence of ribs from the cervical vertebrae. Cervical ribs usually are isolated to the C7 segment, bilateral approximately two-thirds of the time, and are less commonly seen at more cephalic levels of the cervical spine. They may fuse to the first thoracic rib (osseously or by a fibrous band) or end freely. For reference, the T1 segment is identified as the first segment with transverse processes directed cephalically, in contrast to the lower cervical vertebrae, which exhibit a caudal direction of their transverse processes. Cervical ribs should not be confused with C7 transverse process hyperplasia; the latter does not exhibit a costotransverse joint. Transverse hyperplasia is defined as a transverse process that expends laterally to the distal tip of the T1 transverse process with no evidence of a costotransverse joint. Clinically, cervical ribs are significant because they may promote thoracic outlet syndrome by compressing the brachial plexus or the subclavian vessels at the thoracic outlet. Specifically, cervical ribs may narrow the space between the posterior margin of the first thoracic rib and anterior scalene muscle, through which the nerves and subclavian artery pass to the upper extremity. Thoracic outlet syndrome is marked by upper extremity claudication or neurologic symptoms, especially pain and paresthesia along the ulnar borders of the hands and forearm. The thenar eminence demonstrates muscle weakness and wasting in some patients. Symptoms may be exacerbated by turning the head to the ipsilateral side or raising the involved arm overhead. Additionally, symptoms are more likely with postural changes of drooping shoulders and increased thoracic kyphosis. Cervical ribs may have cartilaginous extensions that are not seen on radiographs, making it difficult to appreciate the true size of the rib on plain film studies. |
| Clasp-knife deformity (Figs. 7-63 and 7-64) | Clasp-knife (or knife-clasp) deformity is the combination of a caudal elongation of the L5 spinous process and spina bifida occulta of S1. At times, a person may experience clinical symptoms (e.g., pain, bladder or bowel dysfunction) during lumbar extension, a presentation known as clasp-knife syndrome. |
| Cystic hygroma | Cystic hygromas are nonmalignant malformations of lymph vessels occurring in the neck and (less commonly) head region. They are typically present during childhood, may be single or multiple, and may regress over time. They appear as a large mass or soft-tissue density in the anterior region of the neck. |
| Diastematomyelia (Fig. 7-65) | This condition is marked by a fibrous, cartilaginous, or osseous bar, partially or completely extending across the vertebral canal. The bar may divide the cord, cauda equina, and meninges. It is most commonly found in the thoracolumbar region and is often accompanied by spina bifida occulta, hemivertebrae, and scoliosis. The impact of the bar on the neuroanatomy is best evaluated with magnetic resonance imaging. |
| Facet tropism (Figs. 7-66 and 7-67) | The lumbar zygopopyphyseal joint planes are normally J-shaped, with the longest part of the joint oriented symmetrically in the sagittal plane. Facet tropism (Greek for “turn”) or facet asymmetry describes an asymmetric presentation of the joint planes, where one side is oriented mostly in a sagittal plane and the contralateral side is oriented in a coronal plane. The clinical importance of this finding remains an issue under debate. Most studies trivialize facet joint asymmetry, although it may alter the application of chiropractic care given biomechanical concerns, as has been noted with upper cervical joint asymmetry.82 The lumbar facet angle has been associated with disc degeneration and herniation.22,32,70,98 However, other studies find no association with disc degeneration or disc herniation.10,16,52,67,99 |
| Hahn fissures (clefts)/vascular grooves (Fig. 7-68) | A single, thin, horizontal, radiolucent shadow traversing the middle of the vertebral body. It represents the channel for the segment’s vascular plexus. It is often visualized on radiographic projections of the thoracic and lumbar regions, typically presenting at multiple levels. Hahn fissures are common in young children, but the appearance may persist into adulthood. Vessels provide a similar appearance on the T2-weighted magnetic resonance scans, presenting as a small triangular focus of increased signal. |
| Hemivertebra (Figs. 7-69 to 7-72) | The term hemivertebra describes a vertebra that is only half formed. These vertebrae usually appear in the thoracic region. Three varieties are noted based on the portion of the vertebral body in which this occurs: lateral, dorsal, and ventral hemivertebrae. All hemivertebrae are trapezoidal or triangular in appearance in the frontal plane. They may be continuous with one or both of the adjacent segments (nonsegmented) or separated from the adjacent segments by an intervertebral disc (segmented). A singular lateral hemivertebra promotes a structural scoliosis with the lateral hemivertebra located at the apex of the curvature. Often lateral hemivertebrae are found in bilateral pairs, at differing spinal levels, forming a balanced S configuration of structural scoliosis that is usually small in magnitude, because each compensates for the other. Dorsal hemivertebrae increase the thoracic kyphosis or decrease the lumbar lordosis. Ventral hemivertebrae create the opposite effect. The term scrambled spine has been applied to the presence of multiple levels of block vertebrae and hemivertebrae. |
| Hyoid fragmentation (Fig. 7-73) | The hyoid may appear fragmented as a normal variant. |
| Iliolumbar ligament calcification (Fig. 7-74) | Calcification of the iliolumbar ligament appears as a radiodense band extending from the tip of the transverse process of the lowest lumbar vertebra laterally to the medial aspect of the iliac crest. It sometimes occurs with diffuse idiopathic skeletal hyperostosis (DISH), but more commonly is an isolated finding. Its relationship to clinical findings is ambiguous. |
| Intercalary ossicle (Figs. 7-75 and 7-76) | A small ossicle is sometimes found in the anterior margin of the intervertebral disc space representing calcification of the anterior longitudinal ligament. It is metaplastic in origin and represents a normal variant of no clinical significance; it may be found in association with degenerative disc disease of the corresponding disc segment. |
| Intervertebral disc calcification (Figs. 7-77 to 7-79) | Intervertebral disc calcification occurs in the nucleus or, more commonly, the anulus fibrosus. It may appear linear, oval, or round. It is often seen in adults in association with degeneration, but idiopathic asymptomatic changes also can occur in children. Chapter 17 presents a more lengthy discussion of intervertebral disc calcification. |
| Intervertebral disc hypoplasia | Underdevelopment (or hypoplasia) of the intervertebral disc is seen in several congenital defects such as blocked segmentation and sacralization or lumbarization. When the L5 disc space is slightly decreased, care should be taken not to misinterpret the changes as degenerative. Thus, a narrowed L5 disc space, without features of degeneration (e.g., osteophytes, vacuum phenomena) should be interpreted as disc hypoplasia, assuming that infection and other causes can be excluded. Disc hypoplasia is a common cause of a narrow disc space at the L5 level in a younger patient who is not likely to exhibit degeneration. |
| Klippel-Feil syndrome (Figs. 7-80 and 7-81) | Klippel-Feil syndrome is a rare condition marked by one or multiple levels of blocked segmentation. Approximately half of patients with multiple blocked segments demonstrate a clinical triad of low hairline, limited range of motion, and a short webbed neck. (See Chapter 8 for a complete discussion of Klippel-Feil syndrome.) |
| Limbus bone (Figs. 7-82 to 7-86) | A limbus bone is a small (<1 cm), permanently separated portion of the vertebra’s ring epiphysis that occurs secondary to a peripheral intravertebral herniation of disc material. They are usually noted at the anterior–superior margin of a middle lumbar segment and are of little to no clinical significance. Limbus bones are caused by peripheral intravertebral disc herniations; by contrast, Schmorl nodes are caused by central intravertebral disc herniations. Limbus bones are distinguished from a teardrop fracture by their usual presence of smooth, well-corticated margins, close proximity to the segment, and lumbar location (teardrop fractures are more common to the cervical spine). Intercalary bones are typically in the cervical spine and do not have a defect in the adjacent vertebra, differentiating them from limbus bones. |
| Lymph node calcification (Fig. 7-87) | Calcification of the lymph nodes is a common result of granulomatous diseases (e.g., tuberculosis or histoplasmosis). They usually appear mottled, but at times outer “eggshell” calcification is noted, a feature suggesting pneumoconiosis, treated lymphoma, and sarcoidosis as the etiology when presenting in the pulmonary tissue. Lymph node calcification often appears in the paraspinal soft tissues of the cervical spine. |
| Myelogram remnant | Some of the radiodense contrast may remain in the thecal sac following a myelographic procedure. The older oil-based residual contrast resorbs at approximately 5 mL per year until completely removed. The more contemporary water-based products resorb faster. Radiographically the contrast appears as multiple radiodense droplets in the lumbar dural sac. |
| Nuchal bone (Fig. 7-88) | A nuchal bone is a focal ossification of the nuchal ligament appearing as an oblong, vertically oriented, radiodense osseous structure that varies in size, but is often approximately 1 cm wide and 2 to 4 cm long. It is commonly seen among patients older than 40 years of age and is of limited clinical significance. A nuchal bone is sometimes confused with an ununited secondary growth center of the spinous process, which is typically smaller and has an associated defect of the spinous process, or a clay shoveler’s fracture, which usually is adjacent to a spinous fracture with ragged margins, is inferiorly displaced, and is accompanied by a history of trauma. |
| Nuclear impression (Figs. 7-89 to 7-91) | Nuclear impression, also known as notochordal persistence, is marked by subtle, gradual inward defects of the endplates that tend to involve most of the endplate. They appear as a concave deformity in a lateral radiographic projection. They may appear as two inward defects, creating a double hump appearance known as cupid’s bow in a frontal radiographic projection. The two inward defects appear as radiolucent disc material on axial CT scans, known as an owl sign. Nuclear impression is thought to be a normal variant of no importance, apparently related to a variation of notochordal development. |
| Oppenheimer ossicles (Figs. 7-92 and 7-93) | A persistent or ununited apophysis at the tip of the superior or inferior articular process is termed an Oppenheimer ossicle. They are most common to the lumbar region. Oppenheimer ossicles are differentiated from traumatic fragments by their smooth, well-corticated margins seen on either side of the intervening radiolucent defect, and by the fact that fractures of the articular processes are notably uncommon. Fractures are common in the region of the pars interarticularis but not confined to the articular processes. |
| Rima glottidis (Figs. 7-94 and 7-95) | The rima glottidis (true glottis, rima vocalis) is the fissure between the right and left true vocal folds of the larynx. In the frontal radiographic projection, it appears as a thin (1 to 2 mm), vertical, radiolucent shadow of 2 to 3 cm in length. It is inferiorly continuous with the tracheal air shadow and superiorly continuous with the piriform sinus. The appearance is often mistaken for spina bifida occulta, usually of the C4 segment. The narrow slit of the rima glottidis expands during respiration with abduction of the true vocal folds. |
| Salivary gland calcification (Fig. 7-96) | Calcification within the salivary glands may occur secondary to stone formation, infection, or, less commonly, tumor. Calculi occurring in a salivary gland are usually found in the submandibular gland, but also can occur in the parotid, sublingual, and minor salivary glands. |
| Schmorl node (see also Figs. 7-82 and 7-86) (Figs. 7-97 and 7-98) | A Schmorl node is an intravertebral body herniation of the nucleus pulposus common to the thoracic and lumbar regions of the spine. Schmorl nodes may occur through incomplete pores of the cartilaginous endplates formed by evacuated vascular loops that regress as part of the maturation process. Schmorl nodes tend to appear during childhood. On imaging studies, they appear as abrupt, squared-off, U-shaped, focal defects of either (or both), the superior and inferior endplates. The margins of the defect are sclerotic. Large, usually peripheral Schmorl nodes are sometimes associated with increased diameter of the vertebral body and narrowing of the intervertebral disc space. Schmorl nodes are often multiple and sometimes associated with endplate irregularity and trapezoidal configuration of the vertebrae, together defined as Scheuermann disease. Scheuermann disease is discussed fully in Chapter 9. Schmorl nodes are differentiated from nuclear impressions. Both represent inward defect of the vertebral endplate, but differ in that Schmorl nodes are abrupt, focal defects and nuclear impressions are subtle, gradual defects. Schmorl nodes are similar to limbus bones in that both represent defects arising from adjacent intervertebral disc herniations. However, a limbus bone represents a permanently separated fragment of the epiphysis secondary to a subepiphyseal disc herniation, and Schmorl nodes develop from an intravertebral herniation of disc material. |
| Spina bifida occulta (Figs. 7-99 to 7-102) | Spina bifida occulta describes small, midline, osseous defects of the posterior arch. They are common to L5, S1, and the atlas, appearing as a radiolucent cleft on frontal radiographic projections and as a missing spinolaminar line on lateral projections. |
| Spinous apophysis (Figs. 7-103 and 7-104) | Persistence of the apical spinous apophysis is common at the C7 level. It may result from childhood trauma or represent a nontraumatic variant. It differs from a spinous process fracture in that the former is usually smooth and nondisplaced, while the latter has an irregular anterior margin and is usually inferiorly displaced secondary to muscle tension. |
| Supernumerary segments (Figs. 7-105) | A supernumerary segment is an extra segment. Variation in the number of cervical, thoracic, and lumbar segments is not uncommon. The lumbar region demonstrates the greatest variation. |
| Thyroid cartilage calcification (Figs. 7-106 to 7-108) | Physiologic calcification of the thyroid cartilage is common with increasing age. The finding appears as a mottled pattern of the calcification at the C5-6 level. It has the shape of a shield on anteroposterior film. |
| Transitional vertebra (Figs. 7-109 to 7-111) | A transitional vertebra (lumbarization and sacralization) is a segment that takes on the morphologic characteristics of an adjoining structure or region. Occipitalization, cervical ribs, lumbar ribs, or variations in the number of vertebrae are all types of transitional segments. The most common transitional segment occurs at the lumbosacral junction. For instance, at the lumbosacral junction, the S1 segment may appear with lumbar characteristics (lumbarization of S1) or the L5 segment may appear with sacral characteristics (sacralization of L5). Lumbarization and sacralization appear identical on imaging studies. The terms refer to whether the transitional segment represents the true L5 or S1 level. In other words, lumbarization is lumbar assimilation of S1 and sacralization is sacral assimilation of L5. Because of the variation in the number of segments in each region, it is not possible to definitively know whether a lumbosacral transitional segment is L5 (sacralization) or S1 (lumbarization) without counting down from the T1 segment. It is not always possible to obtain a true count of the vertebrae, leading most to prefer the inclusive term transitional vertebra over the more specific terms of lumbarization or sacralization. The prevalence of a lumbosacral transitional vertebra is reported to be 0.6% to 25%.80 Sacralization of L5 is approximately 30 times more common than lumbarization of S1.60 Transitional segments have been reported to be more common among men,60 but equal gender predisposition also has been reported.55 Radiographically, they are defined by the presence of a rudimentary, thin intervertebral disc below the transitional segment and broad transverse processes on one or both sides of the transitional segment (known as batwing deformity if bilateral). More specifically, there are four types of presentation of transitional vertebrae.17 Each type has two subtypes. Type I appears with a dysplastic broad (or spatulated) transverse process that measures more than 19 mm in a vertical dimension. A type II transitional segment demonstrates a pseudojoint between the broad transverse process of the transitional segment and the superior margin of the sacrum. A type III transitional segment is marked by bone fusion between the transverse process of the transitional segment and the segment below. Types I, II, and III have subtypes A and B, denoting whether the morphologic changes defining the type are presenting unilaterally (subtype A) or bilaterally (subtype B). Type IV is a mixed presentation of type II on one side of the transitional segment and type III on the opposite side. There are suggested but not well-supported links between lumbosacral transitional vertebrae and clinical findings. Vergauwen and others found higher incidence of intervertebral disc degeneration, facet arthrosis, and spinal stenosis at the level above a transitional vertebrae than normally expected.100 The types I and II transitional segments are associated with reduced intersegmental motion. No intersegmental motion is expected across types III and IV transitional vertebrae. Transitional segmentation often is mentioned as a possible cause of low back pain61; however, a strong empirical correlation is lacking.55,60 When a lumbosacral transitional segment presents with scoliosis and sciatica it is termed Bertolotti syndrome. |
| Transverse process apophysis (Figs. 7-112 to 7-114) | Persistence of the apical apophysis of the transverse process is considered a normal variant, appearing most commonly at T1 or upper lumbar segments. |
| Transverse process pseudoarthrosis (Fig. 7-115) | The transverse process of adjacent cervical vertebrae may demonstrate enlarged anterior tubercles that articulate forming pseudoarthrosis. This finding is most common at C5-6.2 |
| Trapezoidal segments (Figs. 7-116 and 7-117) | Middle to lower thoracic and upper lumbar vertebrae present with a slight trapezoidal or wedged configuration, narrowed to the anterior, as a variant of normal, unrelated to accompanying disease. In such presentations, traumatic or pathologic compression fractures need to be excluded. A trapezoidal shape is clinically relevant if found at the level of spondylolisthesis. Trapezoidal segments, narrowed to the posterior, are more likely to continue to anteriorly displace. |
| VACTERL syndrome | VACTERL is an abbreviation for Vertebral anomalies (and vascular defects), Anal atresia, Cardiac anomalies, Tracheoesophageal fistula, Esophageal atresia, Renal and Radial dysplasia, and Limb bud anomalies. The common link among the defects is that they all arise from a mesodermal defect occurring before the seventh week of fetal development. |
| Vertebral ring epiphysis (Fig. 7-118) | The vertebral bodies of infants and very young children appear oval on a lateral radiograph. As the child ages, the ossifying vertebral body demonstrates more of a rectangular appearance, but there remain “step-like” defects seen most prominently at the anterior corners of the lumbar vertebrae and slanted anterior corners of the thoracic vertebrae. This appearance is most notable between ages 6 and 9 years. Typically around the age of 12 years, the cartilaginous endplates begin to ossify, giving the appearance of small ossicles adjacent to the anterior margins of the vertebral bodies of the thoracic and lumbar segments. Fusion of the endplates begins around 15 years of age and is typically complete by 25 years of age. |
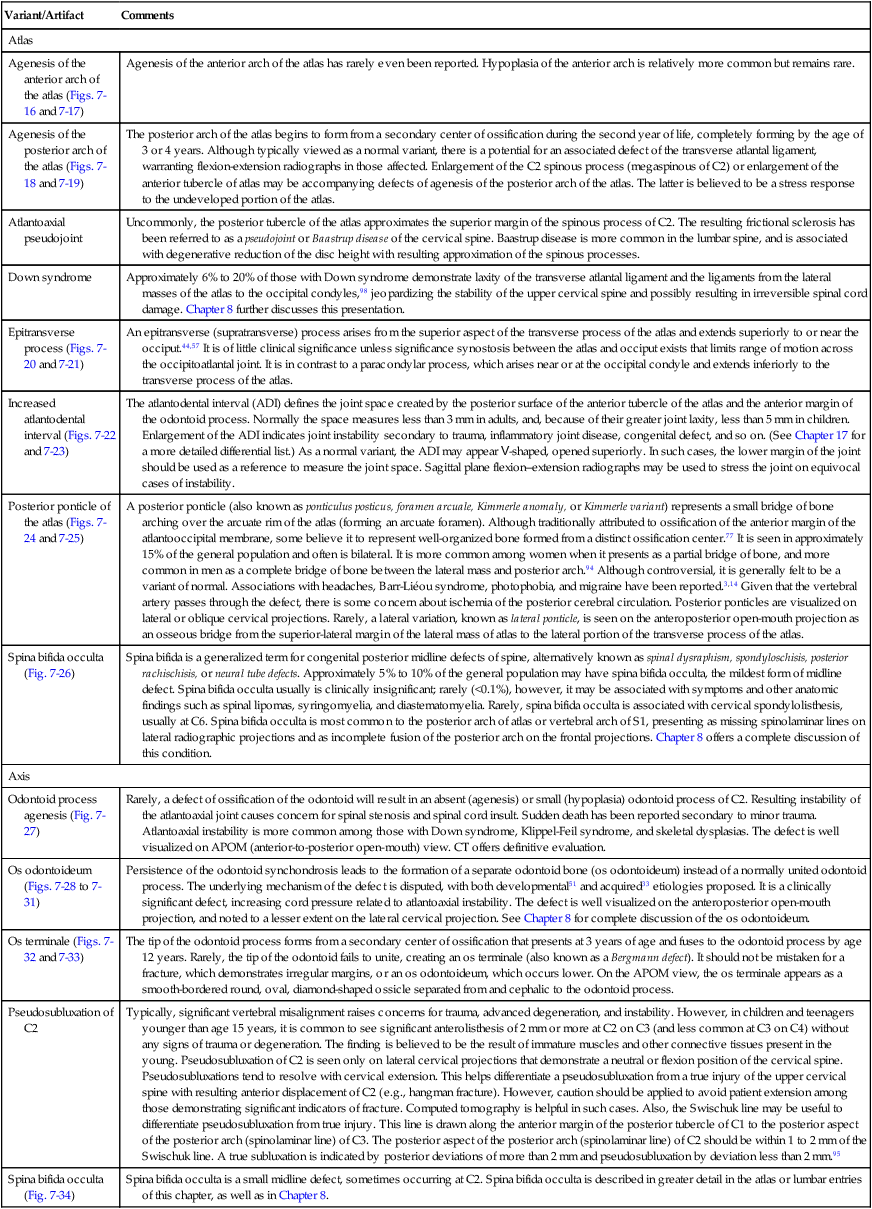
TABLE 7-3
NORMAL SKELETAL VARIANTS AND DEFECTS OF THE SACRUM, COCCYX, AND PELVIS
| Variant | Comments |
| Acetabular protrusion (Fig. 7-119) | Inward migration of the medial wall of the acetabulum on one or both sides. Inward migration can be assessed with a Köhler line. See Chapter 19 for more detail on this condition. |
| Anterior deviation of the coccyx | Often the caudal end of the coccyx is significantly anteriorly deviated. This configuration is believed to be a normal variant in presentation but must be differentiated from trauma. |
| Artifacts (Fig. 7-120) | A wide variety of artifacts may be identified in the abdomen and pelvis. Commonly seen are tantalum mesh/hernia repair, abdominal aorta surgery, Greenfield-Kinney filter (Greenfield inferior vena cava [IVC] filter), intrauterine device, Hulka clips for tubal ligation, and prostate seeding. |
| Gluteal striations (Fig. 7-121) | At times, the muscle striations of the gluteus major can be seen on the frontal radiographs of the pelvis. |
| Iliac horns (Fig. 7-122) | Bilateral, horn-shaped exostosis, of approximately 2 to 4 cm, may be noted from the posterior surface of the iliac fossae. These iliac horns are pathognomonic of a rare inherited condition termed hereditary osteoonychodysostosis (HOOD), also known as Turner-Fong syndrome or simply Fong syndrome. HOOD also demonstrates dysplastic brittle nails, small or absent patella, small or absent articular condyles of the knees and elbows, joint contracture (especially the elbow), clubfoot, “shamrock”-colored irises, renal dysplasia, and other bone and soft-tissue changes. |
| Iliac vascular channel (Fig. 7-123) | The normal iliac vessel may project as a Y-, J-, or V-shaped radiolucent tubular defect with sclerotic margins overlying the lower margin of the iliac fossa in the frontal projection. It should not be mistaken for a fracture. Iliac vascular channels are similar to the horizontal vascular (Hahn) clefts of the vertebral body. |
| Injection granulomas (Fig. 7-124) | Intramuscular and subcutaneous injections may cause localized inflammatory response, necrosis, and resulting residual tissue calcification. The usual appearance is of homogenous, round densities, less than 2 cm in diameter, common in the buttocks. |
| Ischiopubic synchondrosis (Fig. 7-125) | The normal ischiopubic synchondrosis may persist beyond adolescence, usually appearing as a bilateral bulbous defect at the predictable site of the normal synchondrosis. |
| Os acetabulum (Fig. 7-126) | In the radiology literature, a persistent marginal epiphysis of the acetabulum is referred to as os acetabulum. In truth, this is more likely accessory ossicles located at the lateral margin of the acetabulum. An os acetabulum may be confused with the slightly more superior defect of an avulsion of the anterior inferior iliac spine (AIIS). |
| Osteitis condensans ilia (Fig. 7-127) | Osteitis condensans ilia (OCI) (hyperostosis condensans ilia) is a triangular-shaped (apex superior, base inferior) hyperostosis of the lower, medial portion of the ilium immediately adjacent to the lower portion of the sacroiliac joint. It is uncommon in males, and most common in multiparous females. The defects are usually bilateral, and generally asymmetric. It is mostly a radiographic diagnosis, and is believed to represent a stress response of bone secondary to stresses across the sacroiliac joint71 and pubic symphysis13 secondary to pregnancy or other causes of joint instability. OCI can be differentiated from ankylosing spondylitis by the latter’s tendency to be mostly found in males, involve the sacroiliac joint space, be present with marginal erosions, and cause sclerosis on both the sacral and iliac sides of the joint. An oblique film is invaluable to determine if both sides of the joint are involved, suggesting inflammatory arthritis. OCI has an ambiguous association with clinical complaints. Mild pain is seen in some patients, but not all. Pain is likely associated with the degree of joint instability.13 The condition of OCI may resolve completely, yielding a normal appearance to the pelvis over time. |
| Paraglenoid sulci (Figs. 7-128 and 7-129) | Paraglenoid (preauricular) sulci are symmetric, semilunar notched defects approximately 1 cm deep, located in the lower margin of each ilium immediately lateral to the caudal margins of the sacroiliac joints. Both men and women can demonstrate paraglenoid sulci, but in men they are uncommon and shallow. Women, especially those who have given birth, show deeper paraglenoid sulci. Because the sulcus develops at the site of attachment of the anterior sacroiliac ligament, some believe paraglenoid sulci represent a stress resorption of bone. Other sources suggest the sulci are created by the overlying superior gluteal artery; however, this is thought to be a less-plausible cause.84 Paraglenoid sulci are of no clinical significance. |
| Prostate brachytherapy (Fig. 7-130) | Permanent radioactive prostate seed implants are used alone or in combination with external radiation as a treatment for prostate cancer. |
| Prostate calcification (Fig. 7-131) | Prostate calcification is a common finding among older men. The calcification may be primary or secondary. Primary calcifications develop in the acini of the prostate’s parenchyma. Although the etiology has not been identified, it may be related to desquamated epithelial cells. Secondary prostate calcification is associated with benign hyperplasia, infection, radiotherapy, or carcinoma. |
| Pseudosubluxation of S1 (Fig. 7-132) | The posterior aspect of the S1-2 interspace may appear widened in children. The appearance is a feature of the developing sacrum and should not be confused with trauma or other disease process.15 |
| Pubic ears (Fig. 7-133) | A small (<1 cm) sessile exostosis may be noted from the inferior margin of the superior pubic ramus projecting into the obturator foramen on each side of the pelvis, forming a normal variant known as pubic ears or pubic spurs. Their small size and symmetric bilateral presentation distinguish them from osteochondromas. |
| Sacral agenesis (Figs. 7-134 and 7-135) | Sacral and lumbosacral agenesis describes an uncommon group of congenital disorders that present with a missing caudal portion of the sacrum. In severe cases, all of the sacrum and portions of the lumbar spine are missing, denoting the term lumbosacral agenesis. Four types have been described.78 Type I is either partial or total unilateral sacral agenesis. Type II is partial sacral agenesis with bilateral symmetric defects, but intact sacroiliac joints with the first sacral segment. Type III is total sacral agenesis with the ilia articulating with the lowest vertebrae present. Lastly, type IV is variable sacral and lumbar agenesis with the caudal endplate of the lowest vertebrae articulating with the superior margin of the fused ilia or ilia pseudoarthrosis. The etiology of sacral agenesis is poorly defined. Maternal diabetes9 and exposure to organic solvents have been implicated as causes. |
| Sacral fossae (Fig. 7-136) | Normal fossae of the sacral wings may mimic bone destruction. |
| Spina bifida occulta (Fig. 7-137) | Spina bifida occulta is a small midline defect of spine development. It is common at S1. Table 7-2 discusses the condition in more detail. |
| Supernumerary coccygeal segments | Normally there are four coccygeal segments, but it is not uncommon to have five or six segments constituting the coccyx. |
| Vas deferens calcification (Fig. 7-138) | Calcification of the vas deferens is seen in men, and is associated with longstanding diabetes. It appears as bilateral, tubelike structures present in the lower middle pelvis. |
TABLE 7-4
NORMAL SKELETAL VARIANTS AND COMMON ARTIFACTS OF THE THORAX
| Variant/Artifact | Comments |
| Artifacts (Fig. 7-139) | Commonly seen artifacts include: breast implants, prosthetic valves, pacemaker, and coronary artery bypass graft (CABG). |
| Clavicle companion shadow (Fig. 7-140) | The overlying skin of the clavicle may cause a radiodense shadow that parallels the shaft of the clavicle. The appearance should not be confused with a periosteal response. |
| Clavicle medial apophysis (Fig. 7-141) | Persistence of the medial clavicular apophysis presents as a thin osseous structure that may be confused with a fracture or apical calcification. |
| Costal cartilage calcification (Figs. 7-142 and 7-143) | Calcification of the costal cartilages is common. It is slightly more common among men than women and has a positive correlation to age. It typically presents bilaterally and nearly symmetrically. The pattern of calcification generally begins at the first rib level and progresses to inferior levels. Men tend to demonstrate conduit-like calcification in the periphery of the costal cartilages. Women demonstrate central calcifications, likened to the appearance of a wagging tail or tongue. Calcification of the first rib’s costal cartilage has been noted in 50%39 to 88%58 of subjects studied with CT, with various ages sampled. The prevalence is less on plain films, but it remains a common finding. If the calcification of the first costal cartilage is prominent and isolated, it may be mistaken for a pulmonary mass in the lung apex (known as a Student tumor). An apical lordotic projection (an anteroposterior projection of the lung apex taken with 15 to 20 degrees cephalic tube tilt) resolves any controversy, by projection of the first costal cartilage above the lung field. |
| Hypoplastic ribs | Smaller than normally expected ribs are sometimes noted, typically at T12. |
| Intrathoracic rib | Intrathoracic ribs are usually hypoplastic anomalous ribs that extend into the thoracic cavity, appearing as radiodense shadows appearing transverse or oblique to the normally formed ribs. They need to be distinguished from pulmonary lesions. |
| Pectus carinatum (Figs. 7-144 to 7-146) | Pectus carinatum (pigeon or keel chest) is a deformity where the anterior chest wall is sharply protruded anteriorly. At times, lateral deviation also can be seen. Pectus carinatum is significantly less common than pectus excavatum, the former having an overall prevalence estimated at 0.06% in the United States.63 Although most patients exhibit some degree of thoracic rigidity and decreased inspiratory function, most individuals remain asymptomatic and typically present during adolescence for cosmetic or related psychologic concerns. Pectus carinatum may occur as an isolated anomaly, or in association with congenital heart disease (usually mitral valve prolapse), scoliosis, Morquio syndrome, hyperlordosis, and increased kyphosis.81 Bracing and surgical correction may be used to address significant presentations.35,86 |
| Pectus excavatum | Pectus excavatum (“hollow,” “funnel,” or “sunken” chest) is an inward deformity of the anterior chest wall beginning at the manubrium and sloping posterior to its deepest point just before the xiphoid. The anterior portions of the lower ribs are also posteriorly curved. Pectus excavatum occurs in an estimated 0.3% births, and is three times more common among men.36 It typically presents in the first year of life, but becomes most prominent during the rapid growth phase of adolescence.36 It is associated with scoliosis, congenital heart disease, low bone density, rickets, and asthma. The psychologic impact related to the cosmetic deformity is a more common clinical concern than the possibility of cardiopulmonary compression.31 Because clinical symptoms are uncommon in early childhood, surgical management has been controversial. However, long-term follow-up studies and less invasive surgical techniques confirm benefit of surgical correction in selected cases.35,41 In the lateral projection, the anterior chest wall appears convex posteriorly. In the frontal projection, radiographic features include a straight left-heart border, indistinct right-heart border (false-positive silhouette sign), displaced cardiac shadow to the left, and a prominent pulmonary trunk. Assessment is best accomplished with computed tomography and quantified with the pectus index, calculated by dividing the thorax width (right to left dimension) by the depth (anterior to posterior dimension). The normal value for this index is 2.55 with a standard deviation of 0.35. Patients with an index of more than 3.25 may require surgical intervention.42 |
| Rhomboid fossae | Rhomboid fossae define normal, bilateral, and symmetric irregularities along the lower margin of the medial ends of the clavicles. They mark the site of costoclavicular ligament insertion and should not be confused with fracture or tumor. |
| Rib bifurcation (Figs. 7-147 and 7-148) | A bifurcated (bicipital, bifid, or Luschka) rib is one that appears forked at its sternal end. They are nearly always of no clinical significance, but may be associated with Gorlin syndrome, a rare autosomal dominant cancer syndrome marked by the presence of basal cell carcinomas (or basal cell nevus syndrome where the nevi are basal cell carcinomas) and anomalies of multiple organ syndromes. At times the bifid end of the rib gives the false appearance of a pulmonary cyst. |
| Rib foramen | This is a variant formation of a radiolucent foramen within the body of a rib. |
| Rib synostosis (Fig. 7-149) | Adjacent ribs sometimes fuse, representing a variant of no significant clinical concern; however, there is a weak association with the presence of developmental foregut defects. |
| Scapula apophysis (Fig. 7-150) | The secondary ossification centers of the scapula typically fuse by the third decade; persistence may mimic a fracture. |
| Srb anomaly | Srb anomaly is partial longitudinal fusion of the first and second ribs to form a continuous osseous plate. |
| Straight back syndrome (Fig. 7-151) | Straight (or flat) back syndrome describes the coupled findings of reduced thoracic kyphosis (“cobbler chest”) and heart murmur. Traditionally, straight back syndrome was thought to be a “pseudo” heart disease; that is, that the heart murmur was secondary to the narrowed anteroposterior diameter of the thoracic and resulting compression of the heart. However, current literature suggests that straight back syndrome is related directly to mitral valve prolapse.3 Mitral valve prolapse also is associated with other structural deformities of the chest, including scoliosis and pectus excavatum.54 Palpitations and chest pain are the most common symptoms. According to Davies,25 straight back syndrome is defined on a lateral radiograph by measuring the interval between the anterior margin of T8 and a line constructed from the anterior margin of T4 to T12. A distance less than 1.2 cm is indicative of straight back syndrome. |
| Supernumerary ribs | Rib anomalies may occur in form and number. Too few or too many ribs can present as bilateral or unilateral phenomena. Supernumerary ribs are extra ribs, beyond the normal 12 pair, and typically present at C7 or L1. |
| Suprascapular foramen (Fig. 7-152) | Ossification of the superior transverse ligament (transverse or suprascapular ligament) converts the scapular notch into a foramen or opening. |
TABLE 7-5
NORMAL SKELETAL VARIANTS OF THE UPPER EXTREMITIES
| Variant/Artifact | Comments |
| Accessory ossicle (Figs. 7-153 and 7-154) | An accessory ossicle (small bone) is either an anomalous congenital supernumerary ossicle, a normally present secondary ossification center that failed to unite, or, occasionally, an acquired ossification of posttraumatic degenerative etiology. They are commonly seen about the foot, hand, and wrist. Sesamoid bones are accessory ossicles formed in tendons and ligaments and are common in the first, second, and fifth digits. Although usually they are of no clinical significance, some accessory bones have been related to pain syndromes resulting from fracture, degenerative changes, avascular necrosis, and irritation or impingement of adjacent soft tissue.64,76,79 At times accessory ossicles may be confused with traumatic fragments. Traumatic fragments typically are displaced from the host bone, are irregular, have a partially corticated periphery, and may demonstrate overlying soft-tissue edema. Accessory ossicles usually are smooth, have an entirely corticated periphery, are nondisplaced, and occur in typical locations. In addition, accessory ossicles are most often found to be bilateral and symmetric; fractures are not. Figure 7-153 maps some of the more common accessory bones of the hand. |
| Artifacts | Common artifacts include interphalangeal joint prosthesis and shoulder prosthesis. |
| Brachydactyly | Brachydactyly refers to disproportionately short fingers and toes. It may present as an isolated autosomal dominant defect or in association with other findings (e.g., dwarfism, mental retardation). The short tubular bones develop as a consequence of premature epiphyseal closure. Radiographically, the involved epiphyses appear coned, with the apex directed into the corresponding metaphysis. |
| Calcification of the interosseous | The margin of the interosseous membrane between the radius and ulna often ossifies, membrane yielding an appearance that may mimic a periosteal reaction. Interosseous membrane calcification often occurs concurrently on adjacent bones. |
| Carpal boss | A carpal boss (carpe bossu), first described by Fiolle,34 refers to a bony eminence at the base of the second or third metacarpal. Occasionally it extends to the dorsal aspect of the trapezoid and capitate. It is best visualized on the lateral wrist projection, appearing as a regular bony eminence at the carpometacarpal joint. The condition is usually symptom free; however, pain is associated with overuse syndromes of wrist flexion, and with subluxation of extensor tendons overlying the carpal boss.97 The discomfort and pain are usually treated by conservative means; surgery may be indicated in those cases that do not respond to conservative management. A review of 116 patients treated surgically for symptomatic carpal boss found complete symptoma tic relief in 94% of patients within an average follow-up of 42 months.37 |
| Carpal coalition (Fig. 7-155) | Carpal coalition refers to the uncommon occurrence when a portion of the carpal cartilaginous anlage fails to segment into separate carpal bones. Coalition is most typical between the lunate and triquetrum. Lunate-triquetral coalitions can be subdivided into four types according to the degree of union.88 Previously considered completely asymptomatic, carpal coalition and associated degenerative arthritis of the incompletely involved joints has been proved as a cause of occult wrist pain.62 At times coalition is found with round radiolucent shadows in the subarticular region of the fused bones. This appearance is attributed to abnormal differentiation of the joint space and remnants of misplaced synovial tissue residual to joint development.40 |
| Clinodactyly | Clinodactyly refers to curvature of a finger in a mediolateral plane. Although it may involve any finger, radial deviation of the fifth digit toward the fourth digit is the most common presentation. It can occur as an isolated finding or in association with chromosomal abnormalities (e.g., Down syndrome), developmental disorders (e.g., macrodystrophia lipomatosa), electrical burns, and trauma. |
| Humerus pseudocyst (Fig. 7-156) | The on-end projection of the greater tuberosity during an anteroposterior shoulder projection with internal rotation can sometimes give the illusion of a cyst in the head of the humerus. Similar pseudocysts are seen with the tubercles of the proximal radius. |
| Kirner deformity | Kirner deformity is an uncommon palmoradial curvature of the distal phalanx of the fifth digit. It is usually bilateral. It is thought to result from an anomalous insertion of the deep flexor over the growth cartilage. No treatment is required in view of the absence of any clinical and functional symptoms.26 Splinting may be beneficial for pain relief and, if used early, may delay progression of the deformity. (Disability usually is minimal, and treatment to correct the deformity may prevent recurrence.85) |
| Madelung deformity | Madelung deformity is a congenital malformation of the wrist marked by dorsal and medial bowing of the radius and concurrent normal straight development of the ulna, resulting in a comparatively short radius. The carpal angle (formed by the intersection of two lines on the posteroanterior radiograph, one tangent to the proximal surfaces of the scaphoid and lunate and the other tangent to the proximal margins of the lunate and triquetrum) is decreased beyond the expected normal average value of 130 degrees.43 Consistent with the decreased carpal angle, the proximal row of carpals appears V-shaped. The distal radial epiphysis demonstrates a triangular appearance with premature fusion of its medial half. Over time osteophytes tend to develop along the inferior ulnar aspect of the distal radius. The ulnar head is often enlarged with a tendency toward dorsal subluxation, leading to rupture of the extensor tendons of the fingers related to the deformity.38 Most presentations of Madelung deformity are in association with dyschondrosteosis (Leri-Weill disease), a mesomelic dwarfism, or less commonly with diaphyseal aclasis and Turner syndrome. Cases of independent presentations have been reported.6 Traumatic Madelung deformity may result from injury to the medial aspect of the radial epiphysis. Madelung deformity is more commonly bilateral than unilateral. The clinical impact ranges from little pain and cosmetic disturbance to moderate pain and functional impairment.27 Treatment consisted of resection of the ulnar head, stabilization of the distal ulna, and repair of the extensor tendons by tendon transfers.38 Radiographically it is recognized on the posteroanterior (PA) and lateral wrist projections by the volar and ulnar deviation of the distal end of the radius. Rarely some of the conditions named in the preceding may alternatively result in a “reverse” Madelung deformity marked by an anterior bowing and dorsal angulation of the distal end of the radius with dorsal displacement of the carpals. |
| Negative ulnar variance (Fig. 7-157) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree