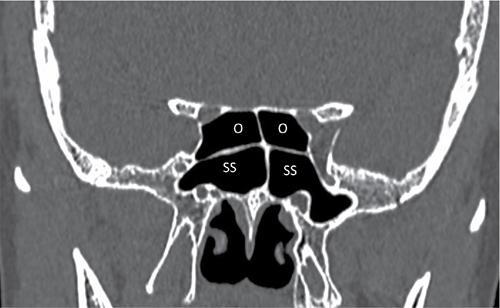
Anagha Rajeev Joshi, Ankita U. Shah, Ashwini Sankhe CT acquisition is done in axial plane using thin collimation (1 mm or below) followed by retrospective multiplanar reconstruction (MPR) which is done in all three planes, i.e. coronal, axial and sagittal plane, using both the bone and soft tissue window. If need be, curved reconstruction can be done. It is advisable to use nasal decongestants prior to CT, unless contraindicated. PNS CT mainly is a plain study with few indications for contrast study such as nasal or PNS masses, e..g., JNA, carcinoma, inverted papilloma and uncommon conditions such as Wegener’s Granulomatosis (Granulomatosis polyangitis—GPA) Role of MRI is limited, naming few, extension of lesion intracranially, into the orbit, into orbital apex, into skull base and perineural spread following the paranasal carcinoma. Nose: The nasal cavity is formed by the nasal bones and is separated into left and right halves by the nasal septum, both of them are triangular shaped. The nasal septum is easily identifiable both on coronal and axial CT sections. Lateral walls of the nasal cavities are complex structures supporting the inferior, middle and superior nasal turbinates and, occasionally, a fourth turbinate, known as the supreme turbinate. The middle and inferior nasal turbinates usually have a similar shape and demonstrate a convex margin medially and a concave margin laterally. The nasal cavity is divided by these turbinates into the superior, middle and inferior meatus (Fig. 3.24.1). The paranasal sinuses consist of paired frontal, ethmoid, maxillary and sphenoid sinuses. The functions of the sinonasal cavity are as follows: The pattern of pneumatization is unique to each group of sinuses and the continuous change in the size and aeration of the sinus as a child grows has a significant impact on the treatment/surgery of sinus pathology in the pediatric age group. There are multiple anatomical variants related to paranasal sinuses, both some of which are significant and insignificant, nonetheless, need to be mentioned in the report. Significant variant is the one, which impairs normal drainage pathways, hinders endoscopic access to distal areas, serves as a focus for occult disease or increases the risk of surgical error. Before we proceed to other variations related to paranasal sinuses, we need to know certain nomenclature regarding pneumatization of sinuses which was first described for the frontal sinus. Although this classification was developed for the description of frontal sinus anatomic variations, it has been now used in the literature for all paranasal sinuses. Cribiform plate: Located in the midline and separates the roof of the nasal cavity from the anterior cranial fossa. It consists of horizontal lamina cribrosa and lateral/vertical lamella. The lateral lamella is the thinnest and most vulnerable bony portion of the skull base and is more prone for intraoperative injury like CSF leak (Table 3.24.1) Narrowness of OMU is due to variations in the uncinate process, ethmoid bulla, middle turbinate, Haller cells, septal deviation or a combination of these (Table 3.24.2). This variable attachment can cause probable damage to the skull base and lamina papyracea while uncinectomy. It increases the wideness of the uncinate and can be potentially dangerous for the infundibulum causing its narrowing. It can cause significant deterioration in OMU function by acting functionally like a concha bullosa or a widened ethmoid bulla. It can obstruct ventilation in the frontal ethmoid cells and the frontal recess region. Lateral deviation—obstructs infundibulum and/or hiatus semilunaris. Medial deviation—affects middle meatus. Horizontal UP is commonly related to an enlarged ethmoid bulla. This variation is significant, if anterior endoscopic sinus surgery is applied. It can cause dangerous complications of orbital and optic nerve injury during uncinectomy, if unidentified radiologically. Variations: Depending on its superior attachment, it can be divided according to Landsberg and Friedman criteria. Ethmoid bulla is large anterior ethmoid air cells and is a reliable surgery marker point because it is the highest and the most constant anterior ethmoid cell. The degree of pneumatization is highly variable. It may present as a giant ethmoid bulla which may narrow or obstruct the middle meatus and infundibulum. The anterior vertical portion of the lamella of middle turbinate attaches to the cribriform plate. The middle portion called ground lamella/basal lamella forms the landmark between anterior ethmoid air cells from the posterior ethmoid air cells. The posterior most attachment is to the medial wall of maxillary sinus (Table 3.24.3). Variations Ethmoidal air cells (Table 3.24.4) The purpose of this IFAC classification was to identify anomalies and variations leading to obstruction of frontal sinus drainage pathway and guide the surgeon for planning of surgical extent (Fig. 3.24.14, Table 3.24.5). Orbital roof pneumatization in the coronal plane is categorized in three patterns – The agenesis of paranasal sinuses is a rare entity which is found to affect the frontal sinus commonly (12%) and maxillary sinus secondarily (5%–6%). Aplasia/hypoplasia of the frontal and/or sphenoidal sinuses may be part of the spectrum of primary ciliary dyskinesia or secondary ciliary dyskinesia; also seen commonly in spectrum of cystic fibrosis. Other clinical syndromes associated with agenesis of paranasal sinuses include Down’s syndrome (hypoplasia of frontal sinus), craniosynostosis, and osteodysplasia (Melnick-Needles). Frontal cells or Kuhn cells: Ethmoidal cells closely related to agger nasi cells (Fig. 3.24.15). According to their pneumatization pattern, frontal cells can be divided into four different types: (Table 3.24.7)
3.24: Nose and paranasal sinuses
Abbreviation
Introduction
Technique
Anatomy
Parts of Nasal Cavity
Drains
Via
Paranasal sinuses
Frontal sinus
Ethmoid sinus
Maxillary sinus
Sphenoid sinus
Drainage pathways of the sinuses
Osteomeatal unit
Drainage pathways



The pattern of pneumatization
At Birth
Growth
Variants of paranasal sinuses
Location
Description of variant
Clinical significance
Radiological points
Olfactory fossa (Fig. 3.24.8)
Olfactory fossa is bounded by horizontal fovea ethmoidalis which is the superior boundary while lamina cribrosa forms the inferior boundary of the olfactory fossa. The vertical distance between the lamina cribrosa and the fovea ethmoidalis represents the depth of the olfactory fossa with the vertically oriented lateral lamella as its lateral border.
Greater the depth, the more prone is lateral lamella for intraoperative injury directly or through manipulation during turbinectomy or ethmoidectomy. Asymmetry in the depth of olfactory fossa can be noted.
The depth of the olfactory fossa is determined by Kero’s classification and measured as height of vertical lamella
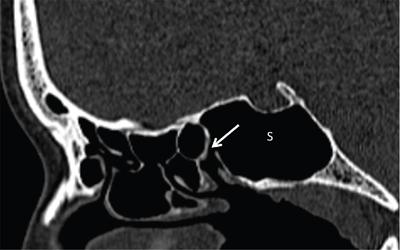
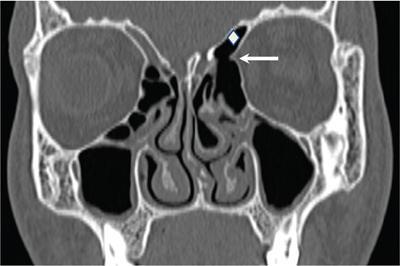
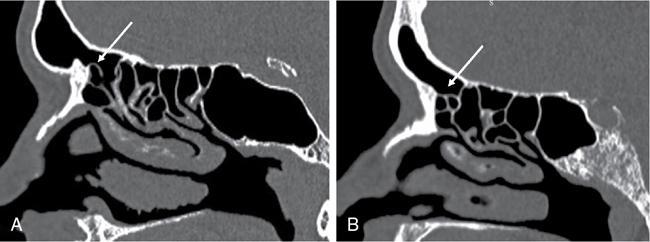
Anterior ethmoidal artery (Fig. 3.24.9)
If the notch abuts the fovea ethmoidalis or lateral lamella, then the artery is considered relatively protected during FESS. The presence of supraorbital pneumatization of ethmoid air cells above the anterior ethmoidal notch places the artery at increased risk of injury during FESS, since the artery travels freely within the ethmoid sinus.
Supraorbital pneumatization is a common and often overlooked critical variant, occurring in approximately 26%–35% of patients. The injury of artery during surgery causes retroorbital haematoma.
Located on coronal CT images by identifying the anterior ethmoidal notch along the medial orbital wall at the level of the anterior ethmoid sinus

Location
Description of Variant
Clinical Significance
Radiological Points
Superior attachment of uncinate process
Lamina papyracea (medial wall of orbit) Or skull base/middle concha.
Infundibular disease will be seen if uncinate process is attached to the skull base or middle turbinate as the frontal recess opens into the ethmoidal infundibulum.Infundibular disease will be spared when the superior attachment is to the lamina papyracea as the frontal sinus will open into the middle meatus directly.
Pneumatized uncinated process or uncinate bulla
Aeration of UP
Can be misinterpreted as concha bullosa or widened ethmoidal bulla.
Deviation of the tip of the uncinate
The UP can show lateral deviation or medial deviation. Rarely, the UP can be spiral, obstructing the middle meatus.
Best seen on coronal CT images.
Curved UP
If it is seen anteriorly and exiting from the middle meatus, it is called ‘Kaufmann’s double middle turbinate’. The horizontal and vertical orientation of UP is determined by adjacent structures.
The UP can show a set of rotation and attachment variations resulting in curved UP. The most commonly observed variation is a medially oriented UP.
Atelectatic UP
It is seen attached to the inferior aspect of medial wall of orbit.
Atelectatic UP is generally seen together with an opacified hypoplastic maxillary sinus.
Bifid UP
Mentioned very rarely in literature
Variant
Description of variant
Clinical significance
Radiological points
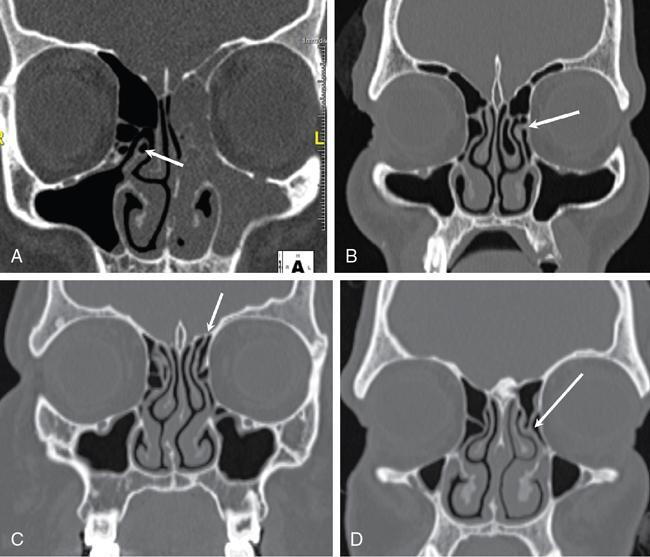
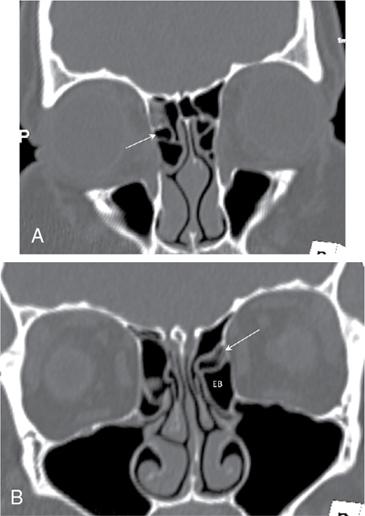
Concha bullosa (30.6% cases)
Pneumatization of the middle turbinate (MT).Occurs due to variation in the ethmoidal air cell system development.
Generally asymptomatic and diagnosed incidentally by CT. Over-pneumatized MT sometimes can lead to nasal obstruction, headache, deviated nasal septum and chronic sinusitis.
Bolger et al classified it into three types depending upon the site of pneumatization.
Paradoxical middle turbinate
Related to change in the curve of middle turbinate. The curved middle turbinate edge is seen inferomedially with the concave surface facing the nasal septum.
It can lead to significant narrowing of the middle nasal meatus and impede the normal drainage of OMU.
Can be easily recognized in CT however can be overlooked by endoscopy.
Secondary and accessory middle turbinates
It arises from the lateral wall of the middle meatus, just below the basal lamella and is located posterosuperior to the infundibulum and generally curves medially and superiorly.
Rare, recently described
Can mimic the real middle turbinate.
Variant
Description of Variant
Clinical Significance
Radiological Points
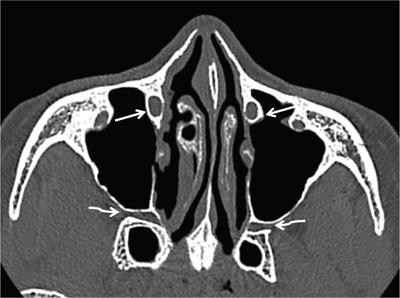
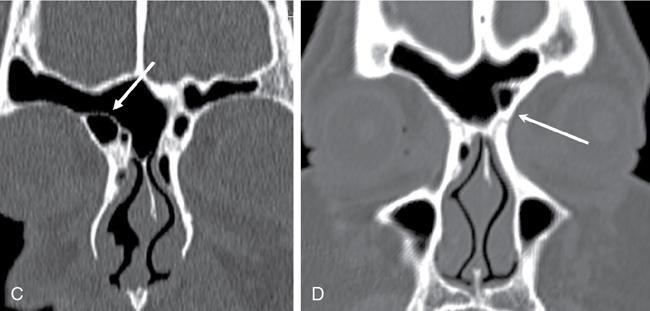
Haller cells (or Infraorbital ethmoidal cells)(Fig. 3.24.12)
Ethmoidal cells located below the ethmoidal bulla, along the orbit floor and related to the maxillary sinus roof. They are seen lateral to the uncinate process and related to the inferior most part of lamina papyracea.
The chances of maxillary sinusitis are more with larger Haller cells.
Best evaluated in coronal computed tomography.
Agger nasi cells(Fig. 3.24.12) (30.6% cases)
The anterior most ethmoidal air cells. Located anteriorly to the upper margin of the nasolacrimal duct and anteriorly to the maxillary sinus infundibulum.
Initially described by H. Meyer; present in up to 98% of cases. Its larger dimensions may directly influence the patency of the frontal recess with frontal sinusopathy.
Best evaluated in coronal computed tomography.
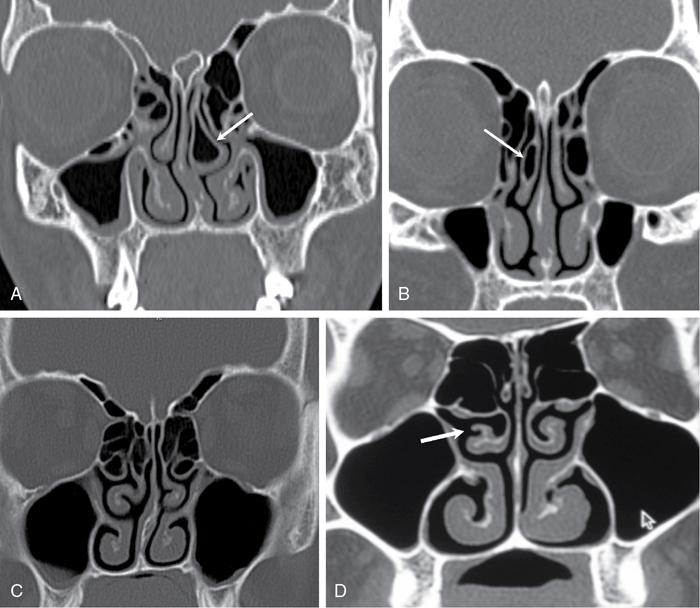
Onodi cells —- also known as sphenoethmoidal cells.(Fig. 3.24.13)
Posterior most ethmoidal cells.
They are closely related to the optic nerves and internal carotid arteries, hence clinically important in the case of sinusopathy of the sphenoid sinuses.
Best evaluated in coronal computed tomography. The optic nerve is at risk when surgical excision of these cells is performed, hence, radiological evaluation prior to surgery is important. These cells also can be a potential cause of incomplete sphenoidectomy.

International frontal sinus anatomy classification (IFAC)
Ethmoidal cell
Cell name
Definition
Anterior cells (displace the drainage pathway of the frontal sinus medial, posterior or posteromedially)
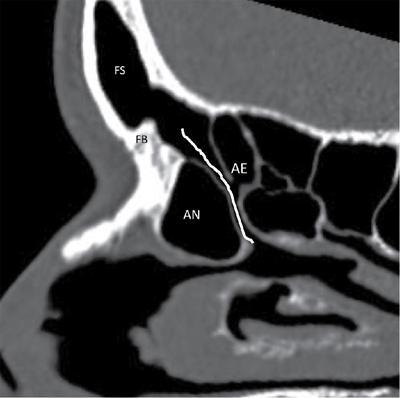
Agger nasi cell (ANC)
Cell that sits either anterior to the origin of the middle turbinate or sits directly above the most anterior insertion of the middle turbinate into the lateral nasal wall
Supra agger nasi cell (SAC)
Anterior-lateral ethmoidal cell, located above the agger nasi cell (not pneumatizing into the frontal sinus)
Supra agger frontal cell (SAFC)
Anterior-lateral ethmoidal cell that extends into the frontal sinus. A small SAFC will only extend into the floor of the frontal sinus, whereas a large SAFC may extend signiflcantly into the frontal sinus and may even reach the roof of the frontal sinus
Posterior cells (displace the drainage pathway anteriorly)
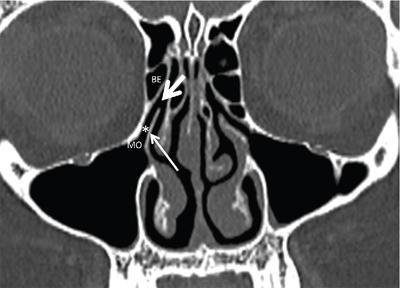
Supra bulla cell (SBC) (Fig. 3.24.13)
Cell above the bulla ethmoidalis that does not enter the frontal sinus.
Supra bulla Frontal cell (SBFC)
Cell that originates in the supra-bulla region and pneumatizes along the skull base into the posterior region of the frontal sinus. The skull base forms the posterior wall of the cell
Supraorbital Ethmoid cell (SOEC) (Fig. 3.24.9)
An anterior ethmoid cell that pneumatizes around, anterior to, or posterior to the anterior ethmoidal artery over the roof of the orbit. It often forms part of the posterior wall of an extensively pneumatized frontal sinus and may only be separated from the frontal sinus by a bony septation
Medial cells (displace the Drainage pathway laterally)
Frontal septal cell (FSC)
Medially based cell of the anterior ethmoid or the inferior frontal sinus, attached to or located in the interfrontal sinus septum, associated with the medial aspect of the frontal sinus outflow tract, pushing the drainage pathway laterally and frequently posteriorly.
Location
Description of Variant
Clinical Significance
Radiological Points
Hyperpneumatization
Aplasia/hypoplasia of frontal sinus
Nasal ventilation has been demonstrated to be an important factor in the development of the paranasal sinuses and thus nasal obstruction might be a contributing factor to reduced expansion of the sinuses.
Type of Kuhn Cell
Location
Percentage %
I
Single cell above agger nasi and below the frontal sinus floor
37%
II
Two or more anterior ethmoidal cells (cluster of cells) that pneumatize above the agger nasi cell, and may extend to the interior of the frontal sinus
19%
III
Unique anterior ethmoidal cells, which, due to their large volume, pneumatize above the agger nasi cell, extending superiorly into the frontal sinus
6%–8%
IV
Isolated cells located inside the frontal sinus, above the agger nasi cell
2%–4%
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







