Abstract
All women should be offered prenatal screening or diagnostic testing for aneuploidy, regardless of maternal age, but with the increasing number of prenatal screening options now available, deciding which is the most appropriate test is increasingly complex. Nuchal translucency (NT) measurement in the first trimester is a powerful marker for Down syndrome. The combination of NT with serum markers in the first trimester detects 87% of cases of Down syndrome for a 5% false-positive rate. NT is also often increased in fetuses with a variety of other genetic conditions, including trisomies 13 and 18, Turner syndrome and triploidy, as well as structural birth defects such as congenital heart defects.
Noninvasive prenatal screening using maternal cell-free DNA (cfDNA) is rapidly transforming prenatal screening, with all tests providing a high sensitivity and specificity for trisomies 21 and 18. In high-risk obstetric populations, it is recommended that this form of testing now be offered as a first-line screening option. The lower prevalence of aneuploidy in younger, low-risk women increases the false positive rate in this particular population. Additionally, trisomies 13, 18, and 21 represent a lower proportion of the chromosomal abnormalities that occur in this group compared with older women. Conventional screening methods with serum analytes and NT measurements are more likely to detect other chromosomal abnormalities, as well as the risk of other adverse pregnancy outcomes. As such, conventional screening with ultrasound (US) for NT remains the most appropriate choice for first-line screening in the general obstetric population.
Keywords
aneuploidy, cystic hygroma, nuchal translucency, prenatal screening
Introduction
In 1866, Down first reported an accumulation of excessive skin in individuals with trisomy 21. In the early to mid-1990s, ultrasound (US) evaluation in the first trimester revealed an accumulation of subcutaneous fluid behind the fetal neck that could explain the apparent excess skin; this finding became known as nuchal translucency (NT). An increase in NT is now recognized to be an early presenting feature of a broad range of fetal chromosomal, genetic, and structural abnormalities. As a result, first-trimester US to assess NT has evolved from an imaging evaluation used in a research setting to a screening tool that is widely available to the general obstetric population.
Major prospective studies from the United States and Europe have confirmed that US performed for NT is a powerful prenatal marker for Down syndrome, with detection rates ranging from 63% to 77% with a 5% false-positive rate. The First and Second Trimester Evaluation of Risk (FASTER) trial showed that screening with NT-based US is even more efficient when combined with maternal serum-free beta-human chorionic gonadotropin and pregnancy-associated plasma protein-A, increasing detection rates to 87% at a 5% false-positive rate.
An increased NT measurement is not uniquely associated with trisomy 21. It is also often increased in fetuses with a variety of other genetic conditions, including trisomies 13 and 18, Turner syndrome and triploidy, as well as structural birth defects such as congenital heart defects, diaphragmatic hernia, skeletal dysplasia, fetal anemia, and neuromuscular disorders. Identification of increased NT alerts the practitioner to the risk of aneuploidy and should prompt a thorough anatomic survey for structural abnormalities and a detailed fetal echocardiogram, even in the setting of a normal karyotype.
All women should be offered prenatal screening or diagnostic testing for aneuploidy, regardless of maternal age, but with the increasing number of prenatal screening options now available, deciding which is the most appropriate test is increasingly complex. Noninvasive prenatal screening using maternal cell-free DNA (cfDNA) is rapidly transforming prenatal screening, with all tests providing a high sensitivity and specificity for trisomies 21 and 18. In high-risk obstetric populations, it is recommended that this form of testing now be offered as a first-line screening option. This population includes women 35 years or older, fetuses with ultrasonographic findings indicative of an increased risk of aneuploidy, women with a history of trisomy-affected offspring, a parent carrying a balanced Robertsonian translocation with an increased risk of trisomy 13 or trisomy 21, and women with positive first-trimester or second-trimester screening test results. Conventional screening with US for NT, however, remains the most appropriate choice for first-line screening in the general obstetric population.
It is important to note that no single test is regarded by the American College of Obstetricians and Gynecologists (ACOG) as superior to other screening tests in all characteristics, and the decision on which test to perform must be based on a number of factors, including the woman’s desire for information, her prior history, cost analysis, and the local availability of reliable testing and appropriate care following an abnormal result.
Disease
Definition
Fetal NT refers to the normal subcutaneous fluid-filled space between the back of the neck and the overlying skin. A small but measureable amount of nuchal fluid can be identified in virtually all fetuses between the 10th and 14th week of gestation. Increased fetal NT thickness refers to the measurement of the vertical thickness in the midsagittal section of the fetus that is equal to or greater than a specific threshold.
Different thresholds have been used to classify NT as abnormal or thickened. NT measurements normally increase with gestational age (crown-rump length), by approximately 15%–20% per gestational week from 10 to 13 weeks. Gestational age–specific cutoffs are required, which might include 95th or 99th percentile values, MoM values (multiples of the median NT measurement for that gestational age), or delta values (deviation of NT from the median for that gestational age). Because gestational age–specific calculations are required, the use of interpretative software programs for risk assessment is necessary. For each measured crown-rump length, the NT measurement represents a likelihood ratio, which when multiplied by the a priori maternal and gestational age–related risk produces a new risk. The larger the NT, the higher the likelihood ratio becomes and therefore the higher the new risk. In aneuploidy screening programs, NT measurements are combined with other risk data, including a range of serum markers, before a final risk estimate is provided to the patient.
Prevalence and Epidemiology
The risk of aneuploidy increases with increasing nuchal thickness; the proportion of fetuses affected depends on the threshold used. In one large series, 12% of fetuses had chromosomal abnormalities when the 95th percentile for NT was used. In another large series, the incidence of aneuploidy by nuchal thickness measurement was 7% with an NT between the 95th percentile for crown-rump length and 3.4 mm, 20% with NT between 3.5 mm and 4.4 mm, 50% with NT between 4.5 mm and 6.4 mm, and 75% with NT 8.5 mm or greater. Approximately 50% of fetuses with increased NT and an abnormal karyotype had trisomy 21; the remainder had other chromosomal abnormalities, such as trisomy 13, trisomy 18, and Turner syndrome.
With respect to euploid fetuses, structural anomalies are detected in approximately 4% to 10% of fetuses with enlarged NT. Cardiac malformations, the most common malformation associated with increased NT, have an overall risk of 3% to 5%.
Etiology and Pathophysiology
Because of the large number of anomalies associated with increased NT thickness, it is unlikely that a single mechanism is responsible for this abnormal fluid accumulation. It is more likely that different pathophysiologic pathways lead to the endpoint of increased nuchal fluid. Cardinal proposed etiologies include abnormal dermal collagen composition in Down syndrome, abnormal nuchal lymphogenesis in Turner syndrome (monosomy X), and aberrant endothelial development and cardiac dysfunction in cardiac anomalies. A number of candidate genes—mainly encoding for endothelium—are involved in both cardiac and lymphatic development. Alterations in these candidate genes may provide a genetic origin for the strong relation between increased nuchal translucency and congenital heart defects. It is proposed that the association with skeletal dysplasias may be due to the presence of a narrow thorax with mediastinal compression, reduced fetal movements secondary to limb fractures, and abnormalities of the cutaneous composition linked with collagen defects.
Manifestations of Disease
Imaging Technique and Findings
Ultrasound.
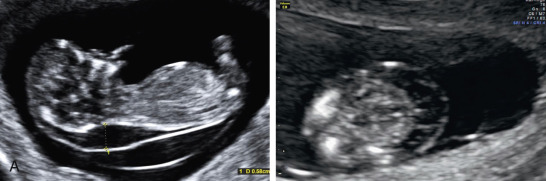
When performing US to assess NT and obtain measurements, optimal technique is critical to ensure the greatest degree of accuracy ( Fig. 45.1 ). The following points summarize criteria derived from the Fetal Medicine Foundation (FMF) and the FASTER Research consortium:
- 1.
NT screening should be performed only by sonographers or sonologists trained and experienced in the technique.
- 2.
Transabdominal versus transvaginal approach should be left to the discretion of the sonographer, based on maternal body habitus, gestational age, and fetal position.
- 3.
US and transducer settings should be optimized to ensure clarity of the image and of the borders of the nuchal space in particular.
- 4.
Gestation should be limited to between 10 weeks and 3 days, and 13 weeks and 6 days (approximate crown-rump length of 38 to 84 mm, although the actual limits will depend on the lab performing the serum analyte testing and the software used).
- 5.
The fetus should be examined in the midsagittal plane, which is defined by the presence of the echogenic tip of the nose and rectangular shape of the palate anteriorly, the translucent diencephalon in the center, and the nuchal membrane posteriorly.
- 6.
The fetus neck should be in a neutral position. The neck is defined as extended if the angle between the lower chin and the anterior neck is more than 90 degrees. Excessive flexion occurs when no amniotic fluid is seen between the lower chin and the anterior neck.
- 7.
The fetus should be observed as distinct from the amnion. The amnion may be separate from the chorion until 16 weeks’ gestation and may be mistakenly identified as the posterior aspect of the fetal skin. Fetal movement should be awaited to distinguish between amnion and overlying fetal skin.
- 8.
The fetal image should occupy at least 75% of the viewable screen.
- 9.
Calipers should be placed on the maximum echolucent space at the back of the fetal neck. The cross of the calipers should be placed on the inner borders of the nuchal fold. Only a cross-shaped caliper (+) should be used; other caliper configurations (e.g., ×, /, ÷) should not be used.
- 10.
Calipers should be placed perpendicular to the long axis of the fetal body.
- 11.
More than one measurement should be obtained, and the largest measurement that meets quality criteria should be used.
- 12.
The umbilical cord may be around the fetal neck in about 5% of cases, and this finding may produce a falsely increased NT. In such cases the measurements of NT above and below the cord may differ, and in the calculation of risk it is appropriate to use the average of the two measurements.
- 13.
At least 20 minutes should be dedicated to the NT measurement before abandoning the effort as failed.

The FMF in the United Kingdom and the Nuchal Translucency Quality Review (NTQR) program developed by the Maternal Fetal Medicine Foundation in the United States both advocate an initial didactic training program that outlines and discusses the theory underlying NT-based screening, and demonstrates US technique to standardize measurements. Sonographers and sonologists demonstrate their technique in the clinical setting by submitting images (five images for NTQR, three images for FMF) for approval to a central expert review team. Both groups also provide ongoing quality monitoring for their respective participants by periodically comparing the distribution and standard deviation of NT measurements against measurements obtained from a standard referent curve. Ongoing quality monitoring is essential to achieve the detection rates shown in clinical trials, with remediation for excessive deviation from established standards.
Differential Diagnosis From Imaging Findings
Differentiation between septated cystic hygroma (CH) and increased NT is frequently debated in the field of first-trimester screening ( Fig. 45.2 ). In the FASTER study, CH was defined as an enlarged hypoechoic space at the back of the fetal neck, extending along the length of the fetal back, with clearly visible septations. Using this definition, 132 cases of CH were identified with a mean NT size of 6.5 mm. They were associated with abnormal fetal karyotype in 51% of fetuses and fetal structural malformation in 34% of chromosomally normal fetuses.