Fig. 30.1
A 55-year-old female patient presenting with symptomatic patellofemoral osteoarthritis due to patellar maltracking and increased lateral patellar tilt – SPECT/CT images show an increased 99mTc-HDP tracer uptake within the lateral part of the patellofemoral joint
30.3.2 Cartilage and Osteochondral Lesions
The importance of the integrity of the subchondral bone plate has not only recently gained increasing interest. Generally, MRI is the standard imaging procedure in patients with suspected cartilage lesions (Hayashi et al. 2012). It is able to accurately characterize the size and depth of the cartilage lesions (Hayashi et al. 2012). In addition, it has been shown that the bone oedema present in MRI is a predictive factor for outcome of these cartilage lesions. However, it is very unspecific and it remains unclear what pathophysiology the bone oedema reflects (Buck et al. 2009). The major advantage of SPECT/CT in patients before and after cartilage surgery lies in its strength to evaluate the integrity of the subchondral bone plate (Hirschmann et al. 2012b). We believe that in contrast to MRI, SPECT/CT helps to differentiate between pure chondral and osteochondral pathologies. Hence, we use SPECT/CT preoperatively to establish the optimal indication for chondral or osteochondral surgery and postoperatively to follow up patients after osteochondral repair procedures (Fig. 30.2).
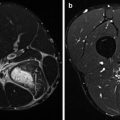
Fig. 30.2
An asymptomatic 19-year-old patient 1 year after osteochondral grafting (MaioRegen, Finceramica, Italy) due to osteochondritis of the medial femoral condyle
Etchebehere et al. noted that bone scans precede radiographic changes in osteonecrosis of the knee (Etchebehere et al. 1998). Another established indication of SPECT/CT is the assessment of osteochondritis dissecans (OCD) (Konala et al. 2010). Konala et al. described that SPECT/CT was helpful in patients with pain after refixation of OCD (Konala et al. 2010). In particular in cases of delayed healing and suspected non-union, SPECT/CT proved beneficial to judge the healing and integration of the osteochondral fragment and guide further treatment (Konala et al. 2010). In our experience, SPECT/CT arthrography further improves the assessment of stability of the OCD fragment and subsequent decision-making pre- and postoperatively (Fig. 30.3).
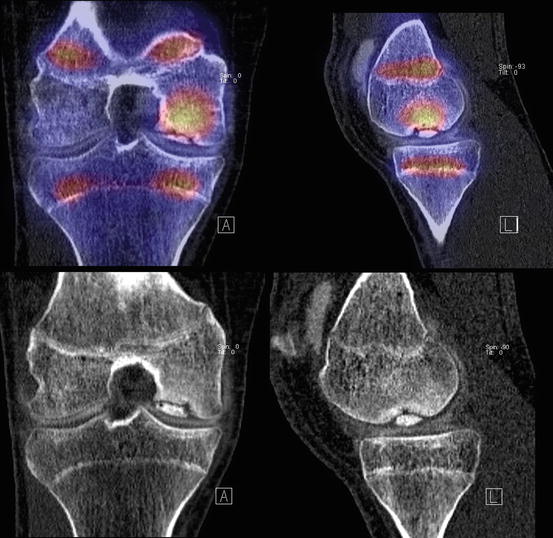
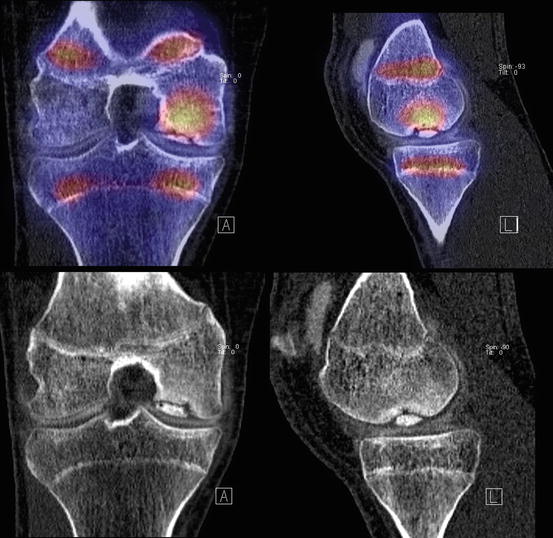
Fig. 30.3
99mTc-HDP arthro-SPECT/CT (upper images) and CT (lower images) of a 16-year-old patient with an osteochondritis dissecans (OCD) of the right medial femoral condyle. The arthro-SPECT/CT shows an intact surface of the OCD and physiologically increased bone tracer uptake at the growth plates
30.3.3 Meniscal Lesions
Clearly, MRI is considered to be the gold standard in the diagnosis of meniscal lesions. Most studies looking into bone scans or SPECT for diagnosing meniscal lesions were performed before the introduction of MRI (Collier et al. 1985; Dorchak et al. 1993; Murray et al. 1990).
However, there are still some indications for nuclear medicine modalities as second-line diagnostics, for example, when a patient has metal implants around the knee joint causing extensive metal artefacts or an implanted pacemaker.
Grevitt et al. investigated 60 patients using SPECT, which then underwent an arthroscopy of the knee due to a suspected meniscal lesion (Grevitt et al. 1993). They reported a sensitivity of 90 %, specificity of 81 % and accuracy of 84 % in diagnosing meniscal lesions (Grevitt et al. 1993). Typically a crescent-shaped pattern of tracer uptake was found (Grevitt et al. 1993). Collier et al. found similar results in terms of sensitivity and specificity (Collier et al. 1985). The biggest problem with these studies is that in most of these studies, chondral and osteochondral lesions as well as the type of meniscal lesion were not taken into account. It is further unclear what the tracer uptake pattern really reflects. Some believe that the uptake is within the vascular zone of the meniscus, others believe that the traction on the coronary ligaments occurring at the time of meniscal trauma and subsequent bony lesions on the attachment site or subchondral bone are responsible for the development of this uptake pattern (Collier et al. 1985; Grevitt et al. 1993). Changes within the adjacent femoral condyles are also taken into consideration for posterior horn lesions (Collier et al. 1985; Grevitt et al. 1993).
In our experience, SPECT/CT is helpful to visualize and identify mechanical overloading of the different knee compartments, which could be regularly seen in patients after total or subtotal meniscectomy (Fig. 30.4). If SPECT/CT is not available, SPECT could also be used considering its limitations. SPECT/CT is also beneficial before and after meniscal substitution surgery, e.g. using polyurethane or collagen meniscus implants. One could evaluate if the preoperatively existing SPECT/CT tracer uptake within the overloaded knee compartment disappears or is at least reduced due to the performed surgery. Using SPECT/CT, the orthopaedic surgeon, sports physician and patient have a direct view into the joint homeostasis and biological state of the knee joint (Hirschmann et al. 2010a; 2011a, b; 2012b). In a currently unpublished date, Hirschmann et al. have shown that in comparison to MRI, the overloading of the knee compartment can be visualized. It was found that bone marrow oedema does not reflect overloading, but bone tracer uptake does. It then guides the optimal treatment (e.g. meniscal substitution, high tibial osteotomy, cartilage or osteochondral repair).
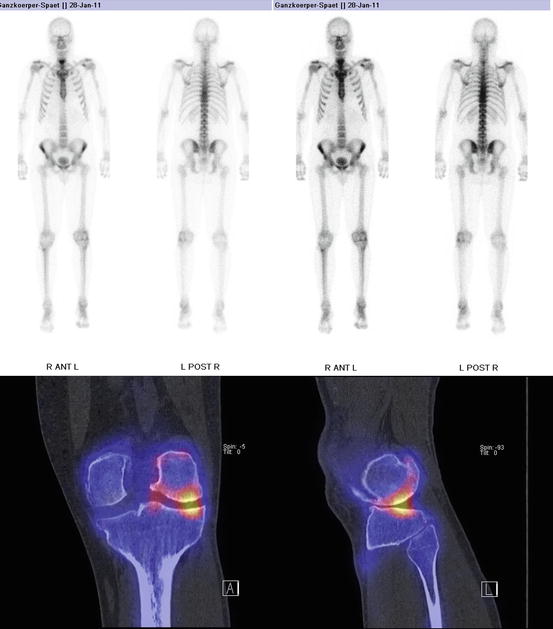
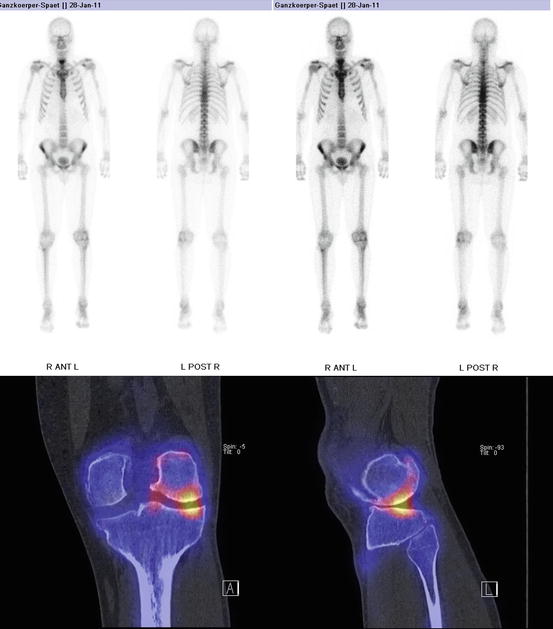
Fig. 30.4
99mTc-HDP SPECT/CT of a 55-year-old female patient 10 years after lateral subtotal meniscectomy indicating an overloading of the lateral knee compartment
30.3.4 Mechanical Overloading of Knee Compartments
Mechanical overloading of the knee joint is characterized by a disbalance of knee protective factors and mechanical loading of the different knee compartments. It is well understood that one of the most important factors leading to mechanical overloading of the medial tibiofemoral knee is a proximal tibial varus deformity, in which the mechanical axis passes medially from the knee centre. Mechanical overloading inevitably leads to an increased risk of osteoarthritis. A variety of nonsurgical such as deloader braces or insoles and surgical therapeutic options (e.g. distal femoral or proximal tibial osteotomies, patellofemoral realignment procedures) aim to reduce the loading in the corresponding medial, lateral or patellofemoral knee compartment.
Conventional radiographs in anterior-posterior, lateral and patella skyline views and long leg radiographs to assess the mechanical leg axis are considered to be the primary imaging in patients under suspicion of a mechanical overloading. In the last decades, bone scans and SPECT have been mainly used as second-line imaging in patients not doing well after correction osteotomy. However, in the last 5 years, the clinical value of SPECT/CT in these patients has been increasingly recognized (Hirschmann et al. 2012b). SPECT/CT offers the combined assessment of structure, mechanical and anatomical alignment and functional information. Only recently Hirschmann et al. reported that the anatomical and mechanical alignment of the knee correlated significantly with the distribution pattern and intensity values of SPECT/CT tracer uptake (Hirschmann et al. 2012b). Mechanical varus alignment showed increased tracer uptake on the medial compartment and a valgus alignment on the lateral side (Hirschmann et al. 2012b). To our knowledge, this is the first study showing a clear relationship between knee alignment and compartment-specific tracer uptake in SPECT/CT.
Based on these findings, SPECT/CT was proposed to be used in clinical practice for twofold: firstly, it should be used as preoperative imaging modality to characterize the pattern of overloading aiming for a better targeted treatment such as nonsurgical therapy, osteotomies and partial or total knee replacements. Secondly, it should also be considered for postoperative follow-up of patients after osteotomies. SPECT/CT could differentiate between optimal, over- or undercorrection (Fig. 30.5) (Hirschmann et al. 2012b).
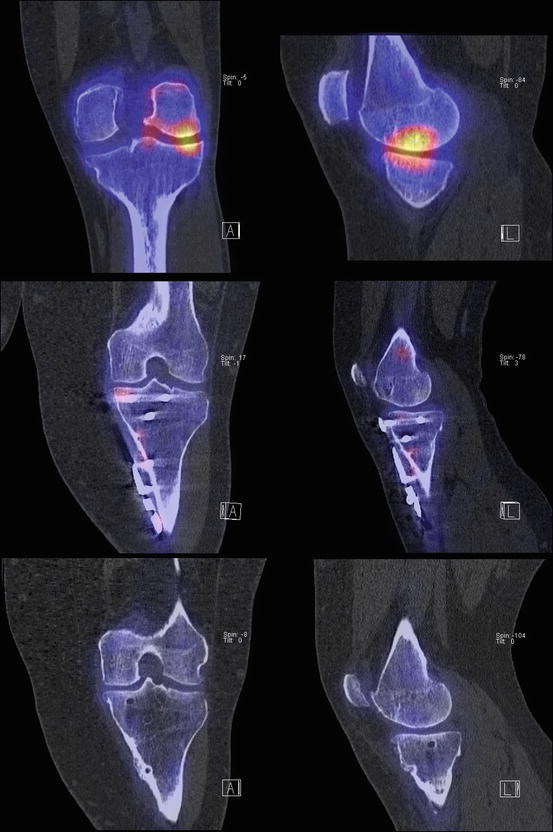
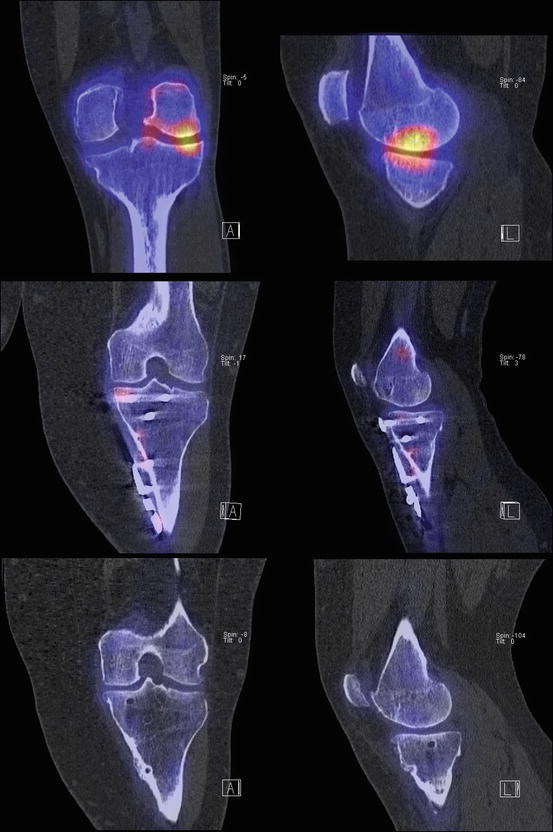
Fig. 30.5
Images of a 42-year-old female patient before and 1 year and 2 years after high tibial osteotomy for correction of varus-deformed knee. 99mTc-HDP preoperative SPECT/CT (upper images) showed increase tracer uptake within the medial femoral knee compartment indicating a mechanical overloading. The 2- and 2-year-follow-up SPECT/CT images showed no tracer uptake anymore indicating an adequate correction of the varus deformity
30.3.5 Ligament Lesions
The radiological diagnostics of ligament lesions such as anterior cruciate ligament tears clearly is the domain of MRI. However, in particular in patients with a retear after ligament reconstruction, MRI could be disturbed by metal artefact splatter. In addition, the evaluation of the tunnel position as well as the assessment of tunnel widening is preferably performed on CT. Numerous authors have emphasized the benefits of 3D-CT for the assessment of tunnel position after ACL reconstruction (Basdekis et al. 2009; Hirschmann et al. 2012a; Purnell et al. 2008).
To date, bone scans or SPECT did not play an important role in the diagnostics of patients with a ligament lesion. However, Even-Sapir et al. correlated the findings of 94 SPECT/CTs of the knee with arthroscopy (n = 74) and MRI (n = 37) or both (Even-Sapir et al. 2002). The patients were suspected to have an ACL lesion or a meniscal tear (Even-Sapir et al. 2002). In 38 patients, an ACL injury was present (Even-Sapir et al. 2002). In these SPECT identified the indirect signs of increased tracer uptake in the posterior lateral tibial plateau (positive predictive value 93 %, negative predictive value 97 % (Even-Sapir et al. 2002). Only in 55 % of these patients, increased tracer uptake was also seen in the lateral femoral condyle (Even-Sapir et al. 2002). On MRI bone bruise was present in 64 %, while all patients had increased tracer uptake in the posterior lateral tibial plateau (Even-Sapir et al. 2002).
In contrast, So et al. reported that an increased SPECT tracer uptake at the ACL attachment site is a primary sign of an anterior cruciate ligament lesion (So et al. 2000). The positive predictive value (PPV) of this primary sign was 94 %, while the PPV of the secondary sign of increased SPECT tracer activity in the tibia or femur was only 81 % (So et al. 2000).
Hogervorst et al. investigated the tibial bone tunnels of 68 patients 2 years after ACL reconstruction using bone scans (Hogervorst et al. 2000b). They found that increased scintigraphic uptake was associated with tibial tunnel enlargement of more than 35 % and a graft length in the tibial tunnel over 14 mm (Hogervorst et al. 2000b). The tracer uptake was also significantly correlated with tunnel enlargement, and tunnel enlargement was significantly correlated with the graft length inside the tibial tunnel (Hogervorst et al. 2000b). They further concluded that return to normal osseous tracer uptake at the tibial tunnel can take more than 2 years when fixation is more than 14 mm below the joint (Hogervorst et al. 2000b).
Just recently the clinical value of SPECT/CT was highlighted for patients after ACL reconstruction (Hirschmann et al. 2012a). We have reported a specific algorithm to analyse and report the position of the tunnels and SPECT/CT tracer uptake in patients after ACL reconstruction (Hirschmann et al. 2012a). High inter- and intraobserver reliability were reported (Hirschmann et al. 2012a). Major advantage is the combined assessment of mechanical alignment, tunnel position and loading of the joint (Fig. 30.6) (Hirschmann et al. 2012a). Its clinical value has to be seen in complex revision cases, in which all these aspects have to be taken into consideration for optimal planning of the subsequent surgical treatment.
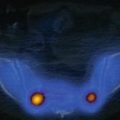
Fig. 30.6
3D reconstructed transparent SPECT/CT images of a 40-year-old patient with a cyclops lesion 1 year after ACL reconstruction (OrthoExpert©)
30.3.6 Osteoarthritis
Bone scintigraphy and SPECT and recently SPECT/CT have proven to be very sensitive for diagnosing osteoarthritis (OA) in early stages, which is the major advantage of nuclear medicine imaging over radiographs, CT or MRI (Hirschmann et al. 2012b). In conventional radiographs as well as CT and even MRI, osteoarthritis can only be diagnosed when the disease already has caused structural damage. SPECT and SPECT/CT open up new vistas into the aspect of biological joint homeostasis. In our experience, SPECT/CT enables the surgeon to precisely characterize the extent and grade of osteoarthritis. This more accurate evaluation of the grade and type of osteoarthritis of the knee could lead to a more targeted and less invasive treatment. Hart et al. found that SPECT helps the surgeon to identify if a patient is instead of total knee arthroplasty suitable for a less invasive procedure such as a high tibial osteotomy or medial unicondylar knee arthroplasty (Hart et al. 2008).
If OA and overloading of the knee joint are identified early, even before any symptoms occur, treatment could be specifically tailored to a more preventive approach. As overloading and overuse injuries are common in sports, SPECT/CT could be used to improve and develop training and prevention programmes, which consider the biological and functional state of the knee joint.
30.3.7 Shin Splint Syndrome, Fractures, Pseudoarthrosis and Osteonecrosis
Bone scans, SPECT and SPECT/CT are very sensitive and specific diagnostic tools for the diagnosis of shin splint syndromes, stress fractures, occult fractures, delayed healing of fractures and pseudoarthrosis (Marks et al. 1992; Ryan and Fogelman 1994).
Yildirim et al. evaluated the knees of 42 active asymptomatic soccer players using bone SPECT to identify stress fractures (Yildirim et al. 2004). In 66 % of patients, increased SPECT tracer uptake indicated a stress fracture (tibia 62 %, femur 5 %).
Etchebehere et al. highlighted that in case of delayed healing of fractures, bone scans are able to differentiate between avascular and hypervascular non-unions and delayed unions (Etchebehere et al. 1998). They further noted that SPECT accurately detects decreased metabolism associated with posttraumatic closure of the physeal plate, which could then lead to growth arrest and leg deformities.
30.3.8 Insertion Tendinopathies (Enthesopathy) and Friction-Related Peritendinous Disease
Insertion tendinopathies are typical overuse injuries, which at the beginning only are symptomatic during and shortly after activity (Adams 2004; Molnar and Fox 1993; Taunton et al. 1987). The iliotibial band friction syndrome is common in runners, that is why it is called runner’s knee (De Geeter et al. 1995; Van Den Eeckhaut et al. 2003). It is caused by friction of the iliotibial tract on the lateral femoral epicondyle (De Geeter et al. 1995; Van Den Eeckhaut et al. 2003). Other common insertion tendinopathies of the knee are the jumper’s and reversed jumper’s knee (Fig. 30.7) (Adams 2004; Molnar and Fox 1993; Taunton et al. 1987).