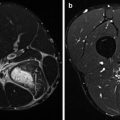
Fig. 27.1
An example of the added value of bone scintigraphy SPECT/CT. Female athlete (rowing) with pain complaints in the left hip region. Flow (a) and blood pool (b) normal. Late static images (c, d) showing slightly elevated uptake in the neck of the left femur. SPECT/CT (e) showing focal intense uptake in the neck of the left femur. Conclusion: small stress fracture of the left collum femoris
27.2.2 Pelvic Avulsion Injury
An apophysis is a secondary ossification centre. It first appears anterolaterally on the iliac crest, later developing posteriorly. The average age of closure of this secondary ossification centre is 16 years for males but may be as late as 20 years. In females, the apophysis usually closes at 14 years, although closure may be delayed until 18 years (Risser 1958). The external oblique abdominal muscle, the transversus abdominis muscle, the gluteus medius muscle and the tensor fascia lata all originate or insert on the anterior iliac crest.
The process of overuse injury starts when repetitive activity weakens a tendon or bone. With sufficient recovery, the tissue adapts to the demand and is able to undergo further loading without injury. DiFiori (1999) reports on the body’s inflammatory response in consequence of microtrauma developing when there is no adequate recovery. Consequently, local tissue can be damaged by the release of vasoactive substances, inflammatory cells and enzymes. Doral et al. (2005) found scintigraphic detection of the injured site to be useful when clinical findings are atypical, when the fracture is not apparent radiographically or when the clinician remains unsure of the precise diagnosis and needs confirmation. A high tracer accumulation at the fracture site in all three phases of the bone scan is seen in a similar way as seen in stress fractures. SPECT/CT can depict the precise anatomical localisation and aid in further differential diagnosis.
27.2.3 Apophyseal Avulsion
Sanders and Zlatkin (2008) report that avulsion injuries usually present as an avulsion of the non-fused apophysis at the level of tendon attachment resulting from violent muscular contractions. Acute apophyseal avulsion injuries are usually easily detected with radiographs, but occasionally MRI or CT is required to detect and fully delineate the extent of injury. Familiarity with the location of various tendon attachment sites on the osseous pelvis can aid in the differentiation between aggressive and chronic lesions. Valdes et al. (2000), Sundar and Carty (1994) and Fernbach and Wilkinson (1981) describe avulsion injuries of the anterior superior iliac spine, the anterior inferior iliac spine and the ischial tuberosity in children and adolescent soccer players. The fracture was caused by a sprint or sudden flexion of the hip during the kicking phase. In bone scintigraphy, a high tracer accumulation at the fracture site in all three phases of the bone scan is seen in a similar way as seen in pelvic avulsion fractures.
27.2.4 Avulsion Injury of Iliac Crest
Rockett (1990) mentioned that radiographs usually show avulsion of the apophysis of the anterior superior iliac crest. Radiographs may appear normal if the avulsed fragment is only minimally displaced or if the injury occurs before ossification of the apophysis. In bone scintigraphy, a high tracer accumulation at the fracture site in all three phases of the bone scan is seen in a similar way as seen in all (avulsion) fractures.
27.2.5 Ischial Tuberosity Avulsion Fracture Versus Apophysitis
Kocis et al. (2003) reported on the ischial tuberosity avulsion injury. The apophysis of the ischial tuberosity usually becomes united with the hip bone by the age of 25. The highest incidence of avulsion in this region as result of overuse injuries occurs between 15 and 17 years in young active persons. Generally, strong muscles are inserted on to the apophyses (Tüzüner et al. 2003).
Apophysitis should be differentiated from an avulsion fracture of the ischial tuberosity. Concannon et al. (2011) showed a case study about the role of bone scintigraphy combined with SPECT in the detection of spondylolysis combined with apophysitis of the posterior superior iliac spine in a young adolescent athlete. The bone scan with SPECT revealed increased uptake at both injury sites. MRI showed oedema at the injury sites. There is a lack of consensus in the medical literature on the optimal approach to diagnose spondylolysis in adolescent athletes. For diagnosis, a number of authors favour the use of a bone scan with SPECT of the lumbar spine followed by CT if the SPECT is positive (Standaert and Herring 2007). Other authors advocate for the primary role of MRI in diagnosis (Masci et al. 2006). and Harvey et al. (1998) show that this approach is inferior to SPECT/CT in identifying stress reactions in the pars interarticularis.
Apophysitis describes a chronic traction injury at the tendon insertion site in chronic excessive sports activities in young persons experiencing gradual onset of pain in the region involved without clear history of injury. Apophysitis is normally confirmed by radiographic findings. However, bone scintigraphy also shows an increased uptake of isotope in the region of the acromion in case of an acromial apophysitis. Increased uptake at the ischial tuberosity may be seen in case of a fracture but also in case of an apophysitis. Kujala et al. (1997) reported in their study population of young athletes a lower mean age of the patients with apophysitis (14 years) than that of the subjects with avulsions (19 years). Apophysitis of the ischial tuberosity usually heals well without complications. Avulsions often cause more prolonged pain with referral pain to the posterior parts of the thigh which often requires operative interventions.
An apophyseal avulsion fracture of the ischial tuberosity occurs usually acute, with a displaced bony or cartilaginous fragment. Patients report usually a sudden movement during sports activities, associated with immediate pain. Radiology confirms diagnosis. Radionuclide bone scanning shows a high uptake at the fractured site and mimics normal fracture uptake patterns at the site of the anatomic substrate in hybrid imaging as in SPECT/CT.
Tendinous avulsion fractures typically occur in soccer and football players, sprinters and jumpers (Cochran 1982). A sudden violent or sustained muscle contraction across an open apophysis is the usual mechanism of injury of an avulsion fracture. Avulsion injuries are common in athletes younger than 25 (Waters and Millis 1988, Watts 1976). If conventional radiological investigation is negative, SPECT/CT can help to find the precise location of the fractured site by showing a high tracer uptake, due to increased osteoblastic activity at the fracture site.
27.2.6 Sacroiliitis
Knowledge of the anatomy and function of the sacroiliac joint, along with an understanding of running athletes’ forces on the joint, is imperative to properly diagnose and treat the runner athlete. Sacroiliitis appears as erosions, sclerosis and joint space narrowing, eventually leading to ankylosis. Tuite (2008) stated that sacroiliitis-like changes of the joint can be caused by several disorders, including repetitive shear-stress injuries in athletes. The radiographic findings of sacroiliitis are often indeterminate because of difficult profiling on the images. CT usually reports the findings of sacroiliitis earlier than radiographs. MRI is mentioned as the imaging technique of choice when very early sacroiliitis is suspected and also for following treatment response. 99mTc-diphosphonate bone scans are more sensitive than MRI or CT scans. In athletes, they demonstrate focal high round uptake confined to the alae. This pattern differs usually from the classic “H” or “Honda sign” pattern, which is diagnostic for sacral insufficiency fractures, which is consistent with bilateral vertical fractures in association with a transverse fracture across the sacrum. Sacral insufficiency fractures are typically found in the elderly. Sacral stress fractures can also be seen in pregnant or postpartum recreational runners. Osteoporosis of pregnancy is reviewed and guidelines on the diagnosis and management of sacral stress fractures are discussed by Lin and Lutz (2004). Blake and Connors (2004) showed that similar bone scintigraphic patterns as in sacral insufficiency fractures are produced by sacroiliac joint dysfunction, sacroiliitis and malignancy.
27.2.7 Groin Pain
Sports injuries in the hip and groin have been noted in 5–9 % of high school athletes (Morelli and Espinoza 2005, Morelli and Weaver 2005). Sports injuries to the hip and groin region occur most commonly in athletes participating in sports that require specific (over) use of the proximal musculature of the thigh and lower abdominal muscles, such as sports that involve kicking, quick accelerations and decelerations and sudden directional changes. Because forces generated through athletic performance are transferred through the hip, injuries to these areas may limit athletes with mild pain or lead to career-ending injuries. Some of these common sports are rugby, skiing, hurdling, (ice) hockey, running and soccer (Verrall et al. 2005, Macintyre et al. 2006, Morelli and Weaver 2005). Symptoms may range from intermittent episodes of mild discomfort to severe and chronic career-ending pain. Groin injuries may result from causes in that same area (e.g. the groin hernia) or indirect groin pain caused by injuries in the hip or lumbar spine or pelvis (the hip-spine dilemma). The differential diagnosis can cover a rather broad area of possibilities. Most common groin injuries are soft tissue injuries, such as (adductor) muscular strains, tendinitis or contusions. More difficult areas to pinpoint are entities as osteitis pubis, obturator nerve entrapment, avulsion fractures and the so-called sports hernia (Anderson et al. 2001, LeBlanc and LeBlanc 2003). Other examples are hip osteoarthritis and femoroacetabular impingement (Tammareddi et al. 2013, Morelli and Weaver 2005).
Kirkendall and Dvorak (2010) stated that 10 % of all soccer injuries occur in the thorax, back, trunk, abdomen, groin and pelvis. They reported that traumatic injuries in soccer included fracture, contusion or haematoma, laceration and muscle, tendon, joint or ligament sprains. Other injuries were caused by overuse. An overuse injury is caused by prolonged repetitive microtrauma without an identifiable event responsible for the injury (Fuller et al. 2006 and Longo et al. 2012). Bone scintigraphy will reflect changes in bone remodelling in response to underlying disease, whereas the diphosphonate compound will accumulate at newly formed bone sites. The manifestation of the type of injury in combination with the thorough history and clinical differential diagnosis determines whether radionuclide bone scan will be of use.
27.2.7.1 Groin and Hip Pain in Musculoskeletal Causes
Groin injury and recurrent groin strains (muscle or tendon injuries) are also common, both in football and hockey players. Groin injury leading to chronic pain is often referred to as a sportsman’s hernia (Fon and Spence 2000). The anatomy of groin hernias is well described in standard surgical textbooks. The many causes of groin pain are described by Zimmerman (1988), Hughes and Maguire (1988) and Corrigan and Stenstone (1985). Rarer causes are bone and joint disease, for example, stress fractures, snapping hip syndrome, spondylolisthesis, early osteoarthritis and slipped upper femoral epiphysis. The differential diagnosis of groin pain can cover also soft tissue injuries, such as muscular strains, tendinopathy or contusions. Athletic pubalgia or avulsion fractures are more difficult areas to pinpoint. Recurrent problems occur when treatment therefore is inadequate.
In general 10–15 % of patients presenting with hip disease also have coexisting lumbar spine disease. Patients with lower back pain frequently have limited or altered hip range of motion, and these patients routinely improve after surgical intervention for hip disease (Redmond et al. 2014). Lower back pain accounts for 5–9 % of athletic injuries (Harvey and Tanner 1991). Spondylolysis is one of the major causes of lower back pain in young athletes (Congeni et al. 1997, Sward 1992, Harvey and Tanner 1991). Micheli and Wood (1995) reported spondylolytic stress fractures or acute spondylolysis of the pars interarticularis in 47 % of 100 adolescent athletes.
At present, there is a paucity of literature examining the hip-spine dilemma in general, and there are no publications about this dilemma in sportsmen. Therefore, imaging should not only be focussed on the hip and pelvis but also include the lower back. Bone scintigraphy including SPECT/CT can be helpful in examining the lower back and the hip region, for example, in athletes with spondylolysis. In interpreting the scan, the clinical context is important. A comprehensive assessment of each patient and in particular of the complex comprising the spine and the pelvis is essential for understanding each individual’s adaptation to the imbalance induced by disorders of the spine or lower limbs (Lazannec et al. 2011).
LeBlanc and LeBlanc (2003) and Hiti et al. (2011) stated that the evaluation of such patients includes a familiarity with the sport and possible mechanisms of injury, including taking a careful history and physical examination. Diagnostic investigations may or may not prove helpful in formulating a final diagnosis. The bone scintigraphy, which can particularly be useful in avulsion fractures and osteitis pubis, reflects the degree of bone remodelling that occurs at the injured site.
MRI has become the standard imaging modality for activity-related groin pain. Lesions, including rectus abdominis/adductor aponeurosis injury and osteitis pubis, are termed athletic pubalgia (Khan et al. 2013).
The diagnosis of a sportsman’s hernia is difficult. The condition must be distinguished from the more common osteitis pubis and musculotendinous injuries. The sportsman’s hernia is an occult “hernia” caused by weakness or tear of the posterior inguinal wall (mostly the external oblique muscle), without a clinically recognisable hernia, that leads to a condition of chronic groin pain. The most common finding at surgery is a deficient posterior wall of the inguinal canal. MRI appears to have excellent diagnostic potential for sports hernia. Most of the time, imaging is normal (Farber and Wilckens 2007, Swan and Wolcott 2007). The role of nuclear medicine imaging techniques is not defined in the sportsman’s hernia. Disorders of the os pubis, stress fractures and various hip pathologies are also causes of groin pain. In osteitis pubis, triple-phase bone scanning can be positive (Morelli and Espinoza 2005).
27.2.7.2 Osteitis Pubis and Osteomyelitis
The symphysis pubis is a non-synovial amphiarthrodial joint situated at the confluence of the two pubic bones, consisting of an intrapubic fibrocartilaginous disc sandwiched between thin layers of hyaline cartilage (Gamble et al. 1986). Bony infection or inflammation of the pubic area is rare. Athletic osteitis pubis is a chronic painful inflammatory overuse injury due to repetitive avulsive trauma of the parasymphyseal pubic bone and/or pubic symphysis, involving the adductor muscles or gracilis (Verrall et al. 2005, Morelli and Smith 2001). Pyogenic osteomyelitis of the pubis in an otherwise healthy athlete can be the differential diagnosis. It is typical in sports with a lot of sprinting and sudden changes of direction, such as running, basketball, soccer, ice hockey and tennis (Fricker et al. 1991, Karpos et al. 1995 and Barry and McGuire 1996). Pauli et al. (2002) showed that both osteitis pubis and osteomyelitis pubis can appear in one patient at the same time. If there is a clinical suspicion of skeletal abnormality, radiography can be performed. Standard anteroposterior radiographs and CT scans are useful to show irregularities of the pubic bone including widening of the symphysis, sclerosis or a decrease in the bone density at the symphysis, cystic changes and marginal erosions in the subchondral bone. MRI is best to image osteitis pubis as it allows visualisation of soft tissue abnormalities and can also demonstrate bone marrow oedema.
There is an absolute role for bone scintigraphy at these indications. In osteitis pubis, the early phases in bone scanning may be or may not be tracer avid, depending on how long the osteitis pubis exists and if there is a low-grade or a high-grade infection. Bone scintigraphy may settle the diagnosis of osteitis pubis, but a negative bone scan does not fully exclude the diagnosis. In osteomyelitis, bone scintigraphy usually shows a combination of focal hyperperfusion, focal hyperaemia and focally increased bone uptake, which is virtually diagnostic for osteomyelitis in patients with nonviolated bone. This triple-phase bone scanning has an accuracy of 90 % and is always been the radionuclide procedure of choice for diagnosing osteomyelitis in bone not affected by underlying conditions (Palestro and Torres 1997, Mandell et al. 1998). Amongst bone scan, white blood cell scan and 18F-FDG PET/CT scan, the bone scan showed greatest numbers of lesions. It has been previously reported that a bone scan is able to detect many asymptomatic lesions (even radiographically obscure foci of the disease). However, keep in mind that abnormalities at radionuclide bone imaging reflect increased bone mineral turnover in general, not infection specifically. It is therefore very important to combine all diagnostic and clinical information for narrowing differential diagnosis. Strobel and Stumpe (2007) reported that 18F-FDG PET scan may be helpful in imaging musculoskeletal infection and might play an important role in the evaluation of chronic osteomyelitis. On the basis of a cumulated reported accuracy (>85 %) and expert opinion, vertebral osteomyelitis is one of the major indications for 18F-FDG PET/CT (Jamar et al. 2013, Chong et al. 2014). 18F-FDG PET is highly effective in excluding osteomyelitis, according to Zhuang et al. (2000). 18F-FDG PET showed promising results for diagnosing both acute and chronic infections of the axial and appendicular skeleton.
27.2.8 Greater Trochanteric Pain Syndrome
Greater trochanteric pain syndrome has expanded to include a number of disorders of the lateral, peritrochanteric space of the hip. This includes trochanteric bursitis, tears or tendinopathy of the gluteus medius and minimus, piriformis tendinopathy and external coxa saltans (snapping hip) (Voos et al. 2007, Strauss et al. 2010, Keung Ho and Howard 2012).
During activities that require repetitive flexion, extension and abduction, an audible and potentially painful snapping of the hip is described as coxa saltans by Strauss et al. (2010). The external variety of snapping hip syndrome involves the soft tissues overlying the greater trochanter, most typically the iliotibial band but also the anterior border of the gluteus maximus.
Trochanteric bursitis is a self-limiting disorder in the majority of patients and typically responds to conservative measures. Patients have a painful hip due to snapping of the iliotibial band over the greater trochanter, resulting in trochanteric bursitis (Zoltan et al. 1986).
Diagnostic imaging in the workup of suspected abductor tendon pathology usually starts with plain radiographs of the affected hip looking for evidence of loose bodies or synovial chondromatosis, which can be causes of the internal variety of coxa saltans. However, similar to cases of trochanteric bursitis or abductor tendon pathology, plain radiographs are typically negative; however, calcification may be seen at the insertion site on the greater trochanter. Ultrasound can also be used to evaluate the abductor tendons, identifying thickening and fluid consistent with tendinosis or the presence of partial- or full-thickness tears (Rask 1980, Sarkis and Chicote–Campos 1978). MRI was shown to be an effective diagnostic tool for excluding intra-articular causes of suspected pathology of the gluteus medius and minimus tendons. Intra-articular causes of a “snapping” hip include synovial chondromatosis, loose bodies, osteocartilaginous exostosis and subluxation of the hip. Extra-articular causes include stenosing tenosynovitis of the iliopsoas tendon sheath near its insertion on the femur (Michelli 1983). Bone scintigraphy shows (mostly slightly) increased tracer accumulation at the site of the trochanteric bursa in bursitis. In literature, radionuclide imaging techniques are rarely mentioned in the workup of the greater trochanteric pain syndrome.
27.2.9 Muscle and Tendon Injury
Strains of the muscle-tendon unit of the adductors (especially tendon of musculus adductor longus, rectus femoris and abdominis) and other muscle groups occur mainly at the proximal end of the tendon itself or to the musculotendinous junction in the muscle belly. The history is important in guiding muscle and tendon injury. Brandser et al. (1995) showed the superiority of MRI to CT, due to better characterisation of muscular or musculotendinous injuries as better in outlining the extent of injury within the muscle group. Sonography is as useful as MRI in depicting acute hamstring injuries and may be the preferred imaging technique because of lower costs. However, MRI is more sensitive for follow-up imaging of healing injuries (Connell et al 2004). The role of radionuclide imaging is not clearly defined in muscle and tendon strains such as hamstring and quadriceps strains or ruptures.
27.2.10 Obturatorius Tendinopathy and Piriformis Muscle Syndrome
Petchprapa et al. (2010) describe entrapment neuropathies such as piriformis muscle syndrome as an underrecognised cause of pain and functional impairment caused by acute or chronic injury to peripheral nerves. Rohde and Ziran (2003) report on obturatorius tendinopathy as a cause of chronic hip pain.
In piriformis muscle syndrome, sciatic pain reproduced on passive internal rotation/adduction of a flexed hip is considered suggestive of the syndrome. The general consensus is that it is caused when hypertrophy, inflammation, injury or anatomical variation of the piriformis muscle result in compression of the sciatic nerve as they both exit the pelvis through the greater sciatic notch. Normally, the sciatic nerve typically passes immediately anterior to the piriformis muscle. This relationship is variable, however, as the nerve occasionally passes through the muscle or splits early, with part of it passing through the muscle. Additionally an accessory piriformis muscle which arises from the more medial part of the sacrum can be implicated. Aetiology could be a narrowed sciatic foramen (in accessory piriformis muscle, muscle hypertrophy, lumbar lordosis), spasm (such as seen in athletes, cerebral palsy) and bursitis and inflammation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree