Nutritional Problems in the Child with Cancer
Jerry Stein
INTRODUCTION
We often associate well-being with good nourishment. We eat comfort foods, follow the growth curves of our children, and espouse the importance of eating right for ourselves, for our families, and for our patients. Notwithstanding the current bout of epidemic obesity (1), we are still a culture that values a healthy diet.
Lay people and medical professionals often picture the child with cancer as a hairless, emaciated, hollow-eyed shadow of normal health, an image that contributes to a common perception that most patients on a pediatric oncology service are severely malnourished. Malnutrition is a common comorbidity in the pediatric cancer ward, and understanding the causes of this problem and the many modalities that are available for its treatment are important components of total care for children with cancer (2). This chapter highlights recent studies on nutritional support for children with cancer, with an emphasis on the specific effects of radiation therapy on the nutritional status of children.
NUTRITIONAL ASSESSMENT OF THE CHILD WITH CANCER
Nutritional status is measured as deviation from population norms by use of a standardized statistic known as the z-score. The z-score measures the number of standard deviations that a measure deviates from the population mean. Because children are dynamically growing organisms whose anthropomorphic characteristics change during the course of development, age-related standards have been generated from population studies. Commonly used anthropomorphic measures of nutritional status include height, weight, body mass index (BMI, weight divided by height squared), weight for height, mid-upper arm circumference, and triceps skinfold thickness. The last two of these measures seem to provide the most reliable indication of malnutrition in children with cancer. BMI is an unreliable tool in the assessment of children with leukemia at risk for malnutrition (3).
In addition to anthropomorphic measures, biochemical markers of nutritional status are often evaluated in children with chronic disease in general and cancer in particular. The ideal biochemical marker should be sensitive, easy to measure, and should have a short half-life so it can reflect recent changes in nutritional status. As opposed to serum albumin, which has a long half-life, prealbumin is an excellent nutritional biomarker. It has a short half-life (2 days as opposed to 3 weeks for albumin), is not an acute phase reactant, and is easily measurable using commercially available kits. Prealbumin is a sensitive tool for measuring the recent nutritional status of children with cancer both at diagnosis and during the course of their treatment (4).
Additional nonanthropomorphic measures of nutritional status in children include determination of whole-body potassium (5), bioimpedence analysis (6), dual energy x-ray absorption (7), and imaging techniques such as MRI (8). Although these techniques are very sensitive, they require specialized equipment and are not available in every center caring for children with cancer. It is not clear if these more sophisticated techniques are substantially better than more universally applicable anthropomorphic measures.
ARE CHILDREN WITH CANCER MALNOURISHED AT THE TIME OF DIAGNOSIS?
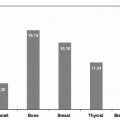
Parents of children with cancer express concern about their child’s nutritional status (9), and children with cancer often show signs of nutritional depletion. A survey of more than 400 children from Central and South America used anthropomorphic parameters to measure malnutrition in children with cancer at diagnosis. The different parameters used in this study identified malnutrition in 16-24% of patients (10). Weir studied 1025 children with acute lymphoblastic leukemia (ALL) in Scotland and found that 35% had a BMI > 0.5 standard deviations below age-adjusted means at diagnosis (11). Other studies have shown variable rates of malnutrition in children diagnosed with cancer, but have not always compared these children with age and socioeconomically matched healthy peers.
CAUSES OF MALNUTRITION IN CHILDREN WITH CANCER
Disease-related Causes of Malnutrition in Children with Cancer
Nutritional status is a reflection of net protein-calorie intake and utilization. Decreased dietary intake is seen in children with cancer at diagnosis, and occurs frequently in the course of therapy. Parents of infants and toddlers often report a decrease in appetite in the days and weeks prior to diagnosis. Space-occupying lesions in the abdomen can cause decreased appetite or early satiety due to physical pressure on the gastrointestinal system, while space-occupying lesions of the central nervous system can lead to decreased appetite and recurrent vomiting (particularly on awakening).
Rapidly proliferating tumor cells have metabolic needs greater than those of normal tissues, and tumors consume substantial amounts of energy both at the time of diagnosis and at the time of relapse (12). The increased metabolic demands of tumor cells are reflected by their avidity for glucose, a phenomenon exploited in positron emission tomography (PET) (13).
On the level of the “whole child,” metabolism is measured as resting energy expenditure (REE), a function of the ratio of oxygen consumption to carbon dioxide generation in patients at rest. The results of REE evaluation in children with cancer are not consistent between studies. Children with high tumor burden (high circulating blast cell counts and organomegaly) at the time of diagnosis of ALL were shown to have high REE values (14), but patients with stage IV metastatic neuroblastoma had surprisingly normal levels of REE despite evidence of malnutrition (15), albeit in a small number of patients who were studied. Another study suggested that children with a variety of solid tumors are in a hypermetabolic state (16). Children in the maintenance phase of therapy for ALL (when tumor burden is low to nearly absent), have REE similar to healthy controls (17), suggesting that chemotherapy of mild intensity does not substantially alter the metabolic needs of children so treated. REE values fall significantly during the first several weeks following stem cell transplantation in children (18). A normal metabolic rate in these children suggests that provision of an adequate caloric intake should restore them to nutritional equilibrium.
If intrinsic rates of tumor metabolism are not to blame for malnutrition among children with cancer, why is malnutrition common in this population? Several theories have been proposed. Tumors often secrete cytokines and hormones that influence metabolism and appetite. In an elegant experiment, Norton and colleagues first demonstrated that a soluble factor was responsible for changes in weight and appetite in response to tumors. In these experiments, circulatory anastomoses were created between pairs of rats where one rat harbored nonmetastasizing tumors, while the other member of the parabiotic pair was a non-tumor-bearing rat. The “healthy” member of the pair subsequently ate less and lost weight. These effects were reversed when the pairs were surgically separated (19). Administration of tumor necrosis factor (TNF) leads to cachexia and other signs of chronic illness in laboratory animals (20). By contrast, injection of TNF did not induce weight loss in humans in one study (21), while administration of TNF in patients described in other studies resulted in symptoms of acute inflammation (22).
Other hormones and cytokines that have been implicated in the cachexia associated with tumors include interleukins 1, 2, and 6, and interferon gamma. These cytokines can cause symptoms of inflammation in animals that are reminiscent of the B symptoms (weight loss, fever, night sweats) experienced by some patients with Hodgkin lymphoma. Although it is reasonable to conclude that these mediators may be responsible for weight loss in patients with Hodgkin lymphoma, studies that have attempted to correlate blood cytokine levels in patients with the presence of B symptoms have shown conflicting results (23).
Elhasid and colleagues demonstrated that although many children have signs of malnutrition at the time of the diagnosis of cancer, nutritional status improves during the course of successful therapy, perhaps in parallel with disappearance of the tumor. This group also demonstrated that the nutritional status of younger children improves more rapidly after the start of therapy as compared with that of older children, reaffirming the notion that younger patients tend to “bounce back” more rapidly than their adolescent counterparts (4).
An unusual cause of malnutrition in children with tumors of the central nervous system (adjacent to the hypothalamus) is the diencephalic syndrome. First described in 1951 by Russell (24), this syndrome consists of severe emaciation, preserved linear growth, together with normal or precocious social and intellectual development. Although classically associated with hypervigilance, euphoria, hyperkinesis, and nystagmus, these findings need not be present to establish the diagnosis, and indeed were absent in a more modern series of patients with this syndrome. The diencephalic syndrome may be the result of acquired growth hormone resistance in patients so affected (25).
Treatment-related Causes of Malnutrition in Children with Cancer
Antineoplastic therapy has dramatic effects on the nutritional status of children. Specifically, radiation and chemotherapy can cause oral and gastrointestinal mucositis, alterations of sense of taste, nausea and vomiting, diarrhea, and infections of the gastrointestinal tract that independently or collectively affect caloric intake and utilization.
Changes in taste and smell perception are reported by many patients during the course of treatment (26). Children have impaired ability to differentiate sour and bitter tastes following total body irradiation (TBI) (27), which may contribute to dysgeusia and aversion for specific foods leading to decreased appetite following stem cell transplantation. Younger children may refuse to eat if their sense of taste is blunted, although older children and adolescents can often be coaxed into eating even if the taste of their food is not “quite right.”
Food aversion is common among children receiving chemotherapy. Pioneering work by Bernstein in the 1970s demonstrated that food aversion develops for specific foods that are ingested prior to the administration of emetogenic chemotherapy. Specifically, children demonstrated an aversion to maple-walnut ice cream 2-4 weeks after they had received chemotherapy only if ice cream of this flavor had been eaten in the hours preceding therapy (28). Food aversion can be easily demonstrated on the pediatric oncology ward as the food cart makes its mealtime appearance and many children immediately cover their noses so as to avoid the “hospitalfood smell.” To many children, the odors that they associate with the hospital can elicit feelings of nausea and can decrease appetite.
Oral and gastrointestinal mucositis are frequent side effects of chemotherapy and radiotherapy. Therapy-induced apoptosis of mucosal epithelial cells and the basal cells that contribute to the constant regeneration of this tissue, results in the local release of intracellular (e.g., NF-κB) and intercellular (e.g., interleukin 1 and TNF) mediators that contribute to inflammation of the mucosa (reviewed in Ref. 29). The resultant inflammation results in ulceration, local bacterial proliferation, a painful mouth, and the
inability to eat. Additionally, antineoplastic therapy causes immune suppression, leading to an increased susceptibility to herpetic oral infection (30), while the antibiotics that children with cancer often receive can predispose to superficial fungal infections of the mouth and esophagus. Blood levels of certain growth factors (e.g., epidermal growth factor) in the saliva of patients receiving radiation therapy to the oral cavity correlate with the severity of radiation-induced mucositis, suggesting a role for cytokine modulation in the evolution and possibly in the treatment of this complication (31).
inability to eat. Additionally, antineoplastic therapy causes immune suppression, leading to an increased susceptibility to herpetic oral infection (30), while the antibiotics that children with cancer often receive can predispose to superficial fungal infections of the mouth and esophagus. Blood levels of certain growth factors (e.g., epidermal growth factor) in the saliva of patients receiving radiation therapy to the oral cavity correlate with the severity of radiation-induced mucositis, suggesting a role for cytokine modulation in the evolution and possibly in the treatment of this complication (31).
Infection of the esophagus with cytomegalovirus, herpes simplex virus (32), or Candida can cause severe dysphagia and chest pain in children with compromised immune systems, and can in turn affect their ability to eat properly. Endoscopy is often required to establish a diagnosis of specific infectious agents that can cause esophagitis (33). Radiation therapy to the mediastinum can induce acute inflammation and of the esophageal mucosa, while esophageal strictures can occur either during therapy or as a late adverse event leading to dysphagia and swallowing dysfunction. This phenomenon can be aggravated by drugs that enhance radiation recall sensitivity such as anthracyclines (34). The cumulative effects of therapy-related mucosal complications result in a child for whom eating (or even the swallowing of saliva) is a painful and unpleasant experience.
Vomiting and nausea are frequent complications of cancer therapy in children, and obviously present a significant obstacle to effective nutrition. Acute abdominal syndromes including severe nausea, vomiting, and diarrhea developed in the majority of children treated with abdominal radiation therapy in the era before effective antiemetics were widely available. The emetogenic effects of abdominal irradiation are probably mediated by local damage to the gastrointestinal mucosa (35). By contrast, chemotherapy causes vomiting in children treated for cancer via stimulation of neurons in the area postrema, the nucleus tractus solitarius, and the dorsal motor neuron of the vagus nerve. Substance P (and its cognate receptor, NK-1) and stimulation of 5-hydroxytryptamine receptors are the dominant biochemical mediators of chemotherapy-induced vomiting.
Other causes of treatment-mediated nausea and vomiting include anticipatory or conditioned nausea, and increased intracranial pressure caused by solid tumors of the central nervous system. Recurrent vomiting results in irritation of the esophagus, and can lead to ulceration and Mallory Weiss tears, exacerbating nutritional problems in children and adolescents.
Radiation and chemotherapy can cause diarrhea either directly (e.g., abdominal radiation or drugs used infrequently in first-line pediatric protocols such as CPT-11) or secondarily (immunosuppression causing gastrointestinal infections and frequent antibiotic use causing overgrowth of gastrointestinal pathogens). Persistent untreated diarrhea that is not successfully treated can lead to malnutrition (36).
Many of the drugs used in cancer therapy induce nutritional deficits as part of their intrinsic mechanism of action. Antimetabolite medications used frequently in the treatment of children with ALL cause depletion of purine nucleotides that are needed for DNA synthesis (37). Asparaginase, a cornerstone of the treatment of lymphoblastic leukemia, causes depletion of asparagine, an amino acid that is needed for the synthesis for many proteins (including insulin and albumin). Corticosteroids induce catabolism, and despite the concomitant hyperphagia that is often seen in children receiving this class of drugs, nutritional status is not improved (38). Corticosteroid use has additional unfavorable effects on calcium deposition in growing bones (39).
DOES NUTRITIONAL STATUS AFFECT TREATMENT TOLERANCE AND OUTCOME OF CANCER THERAPY IN CHILDREN?
There are no large-scale studies of treatment tolerance and nutritional status in children receiving chemotherapy. Pneumocystis carinii (now jevonii) susceptibility, a benchmark infection that reflects the immune-suppressed state of children receiving intense antineoplastic therapy, is enhanced in malnourished laboratory animals (40) and in malnourished children with leukemia (41) suggesting a direct connection between immune function and nutritional status. Children with advanced cancer and malnutrition do not mount immune responses when challenged with recall antigens, but reactivity is restored following several weeks of intravenous alimentation (42). The presence of severe infections hinders the timely administration of scheduled antineoplastic therapy (possibly compromising its efficacy), and of course can endanger the life of the patient (43).
Improved nutritional status may facilitate the administration of dose-intense antineoplastic therapy, as was demonstrated in children receiving a high-risk (more intense) leukemia protocol (44). Several small prospective studies have demonstrated less treatment delays (45) and infections (46) in children with advanced solid tumors who received intravenous hyperalimentation concomitant to their chemoradiotherapy. Studies of dose intensity and nutritional status in children receiving contemporary therapy using high-risk leukemia and solid tumor protocols should be encouraged to explore the role of intense nutritional support in facilitating dose intensity on state-of-the-art protocols.
Nutritional status affects disease-free survival of children with cancer in some but not all studies. A study of children treated in El Salvador and Brazil found no correlation between nutritional status at diagnosis of leukemia or a solid tumor and the outcome of treatment (47). Similarly, no correlation between survival and nutritional status at diagnosis was found in a large cohort of children treated for ALL in the United Kingdom (11). By contrast, studies of children with advanced solid tumors demonstrated improved survival when nutritional interventions such as parenteral hyperalimentation were applied to patients with poor nutritional status at diagnosis (45,46). Surprisingly, children with BMIs at opposite ends of the spectrum (underweight and overweight) suffered an excess of treatment-related mortality and relapse incidence in a recently completed trial involving 768 children with acute myelogenous leukemia, although dose intensity was not affected by BMI (48). By contrast, a study of more than 600 children with ALL enrolled at a single institution on four consecutive treatment protocols did not demonstrate a correlation of BMI and survival. This latter study included extensive
pharmacologic monitoring of systemic exposure to the chemotherapeutic drugs administered throughout therapy, and BMI was not correlated with drug levels (49).
pharmacologic monitoring of systemic exposure to the chemotherapeutic drugs administered throughout therapy, and BMI was not correlated with drug levels (49).
The effect of nutritional status on the quality of life of children with cancer is a current area of interest for many investigators. Issues relating to poor nutrition were common in children and adults with advanced cancer, but issues related to quality of life and nutritional status have not been extensively investigated in children at earlier (and hopefully more successful) phases of antineoplastic therapy (50, 51, 52). A sixitem questionnaire that explores the patient feelings regarding anorexia/cachexia has been designed and validated in children with cancer aged 10-17 years (53). Notwithstanding the relative paucity of extant literature, many parents and some children associate dietary intake with overall well-being, and issues regarding anorexia/cachexia often consume substantial amounts of time and emotional resources in the oncology clinic. Parents can sometimes focus excessively on their child’s dietary intake, leading to stress and conflict between themselves and their child. Clinicians should be alert to this potential flash point and should be prepared to provide the requisite counseling to relieve this source of potential strife.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree