Orbital Spaces | |
| globe: | subdivided into anterior + posterior segments by lens |
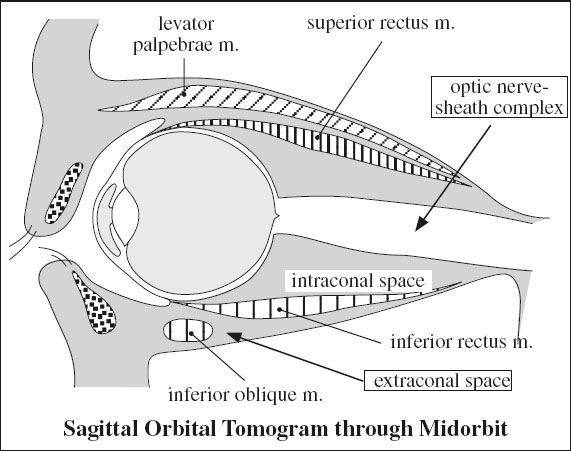
optic nerve-sheath complex: | optic nerve surrounded by meningeal sheath as extension from cerebral meninges |
| intraconal space: | orbital fat, ophthalmic a., superior ophthalmic v., nerves I, III, IV, V1, VI |
| conus: | incomplete fenestrated musculofascial system extending from bony orbit to anterior third of globe, consists of extraocular muscles + interconnecting fascia |
| extraconal space: | between muscle cone + bony orbit containing fat, lacrimal gland, lacrimal sac, portion of superior ophthalmic v. |
B. POSTERIOR COMPARTMENT
= RETROBULBAR SPACE = cone consisting of extraorbital muscles + envelope of fascia divides retrobulbar space into
(a) intraconal space
(b) extraconal space
GLOBE
Ocular globe diameter: 22–25 mm
Wall: composed of 3 layers:
(a) fibrous outermost layer
Function: maintaining shape + pressure of globe
1. Sclera = collagenous tissue layer continuous anteriorly with cornea posteriorly with dura mater
2. Cornea
(b) Uvea = pigmented vascular middle layer
[uvea, Latin = grape]
3. Iris
4. Ciliary body (anteriorly)
5. Choroid (posteriorly) = most vascular structure of globe
Attachment: tethered to sclera by arteries + veins
◊ Most frequent site of intraocular metastases!
(c) innermost sensory layer
5. Retina = light-sensitive (sensory) inner layer
Attachment: firm at anterior margin (= ora serrata) and posteriorly at optic disc
√ various layers of globe are NOT discernable at imaging, especially CT
√ sclera may be separated from choroid at high-res MRI
√ individually visualized in ocular (choroidal / retinal) detachments
Contents: (a) anterior segment containing
1. Aqueous humor subdivided by iris into:
› anterior chamber
› canal of Schlemm (see below)
› posterior chamber
(b) posterior segment containing
2. Vitreous humor
Potential ocular spaces:
(a) between retina + choroid → retinal detachment
(b) suprachoroidal space between choroid + sclera → choroidal detachment
(c) between vitreous + posterior hyaloid membrane → hyaloid detachment
Canal of Schlemm
[Friedrich Schlemm (1795–1858), German anatomist, sentenced for grave robbing, eventually professor at the University of Berlin]
= SCLERAL VENOUS SINUS [misnomer – not a blood vessel]
= circular ringlike endothelium-lined tube lymphatic tube resembling a lymphatic vessel
Location: adjacent to outer angle of anterior chamber in pectinatum iridis (= periphery of cornea) between cornea + iris
Function: collects aqueous humor from anterior chamber and delivers it into the venous system
OPTIC NERVE SHEATH
= extension of dura mater
Content:
1. Optic nerve
2. Ophthalmic artery
3. Small veins
OPTIC NERVE (CN II)
Histo: CN II is an extension of brain = retinal ganglion cell axons myelinated by oligodendrocytes + enveloped within meninges
Segments:
A. Retinal segment leaves ocular globe through lamina cribrosa sclerae
B. Orbital segment travels in center of fat-filled orbit
√ surrounded by dural sheath containing CSF
C. Canalicular segment lies in optic canal below ophthalmic artery; frequently overlooked on radiologic images
D. Cisternal segment in suprasellar cistern leading to optic chiasm
√ anterior cerebral a. passes over superior aspect of nerve
OCULOMOTOR NERVE (CN III)
Exit: from brainstem anteriorly between posterior cerebral (PCA) + superior cerebellar arteries
Segments:
(1) cisternal segment courses through prepontine cistern
(2) cavernous sinus segment along cephalad portion of the lateral dural wall
(3) orbital segment through the superior orbital fissure
(4) division into superior + inferior branches
Function:
(a) motor fibers to
› levator palpebrae muscle
› all extraocular muscles except lateral rectus and superior oblique mm.
(b) parasympathetic fibers to
› internal eye muscles (pupillary sphincter and ciliary muscles) → constriction of pupil via Edinger-Westphal nucleus
Location: periphery of CN III → subject to compression by extrinsic masses
Disturbed function:
(1) “pupil-sparing” oculomotor palsy = loss of motor function in extraocular muscles with relative sparing of pupillary parasympathetic innervation ← compromised blood flow to central microvessels
(2) compression by posterior communicating artery aneurysm ← close association with posterior cerebral (PCA) + superior cerebellar arteries
(3) compression during transtentorial uncal herniation ← course over petroclinoid ligament
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree