13.2 Interoperability
Information systems do not function independently. All systems should be interconnected and work in close cooperation. When linking to other systems, many department systems (e.g., the TPS, treatment delivery system, and treatment management system) require proprietary protocols and connection methods. These proprietary structures restrict selection and lead to high cost and huge effort during system upgrades and/or replacement.
Figure 13.1 illustrates the interoperability of the OIS. Patient demographic data should be exchanged between the HIS and the TMS by using the Health Level 7 (HL7) standard [4]. Worklists and the progression of radiotherapy orders should be transmitted in Digital Imaging and Communications in Medicine (DICOM) Unified Worklist and Procedure Step (UPS) [5] format. Radiation therapy dose calculation push workflow and radiation therapy pull workflow are explained in the UPS document. Treatment planning information should be stored in DICOM radiotherapy (DICOM-RT) object format and communicated using DICOM transfer protocols.
Interoperability also supports medical safety and operational efficiency. Particle therapy departments utilize many information systems. For medical safety purposes, patient demographic information and treatment data should be shared among these systems.
13.2.1 Electronic Medical Records, Electronic Healthcare Records, and Personal Health Records
The OIS must be connected with other HISs (such as electronic medical records (EMR) [6, 7], electronic healthcare records (EHR) [8, 9], and personal health records (PHR) [10, 11]) and communicate with data on basic patient information, treatment information, medical practices, and treatment results. All HISs should share radiation treatment information. This information may be transmitted transparently by each device. We have to consider the method and functionality of this cooperation. As the de facto standard, the HL7 format should be used for electronic data transfer between the EMR, EHR, and PHR and the OIS.
13.2.2 Clinical Database
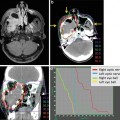
When particle therapy proceeds in a clinical trial, data analysis is very important. The OIS will include functions to summarize and analyze results. Treatment data processed in the EMR, TPS, and TMS will be stored in the clinical database and analyzed by calculating survival curves. The HIS and TMS are connected to the clinical database that generates patient lists specified by treatment protocols and calculates survival ratios. Figure 13.2 shows the relationship between the HIS, TMS, and clinical database.
Fig. 13.2
Clinical database: the clinical database is connected to the HIS and TMS and processes patient and treatment data including results and follow-up information. The patient list and survival curves are also generated
13.3 Treatment Summary and Radiation Oncology Registry
When radiation therapy is completed, radiation oncologists evaluate treatment results and follow up with patients. Therefore, the OIS needs to store clinical data, treatment plans, delivery dosages, radiation effects, and side effects to facilitate comprehensive treatment evaluation. These treatment data should be carefully maintained and summarized within a clinical database system.
Evaluating and improving the quality of radiation therapy requires complete information on cancer stage and treatment results. Hospital-based registries are a key tool. To determine the completeness of registry data, a nationwide cancer database is expected [12, 13]. The National Radiation Oncology Registry (NROR) [14] pilot program was presented as the basis for the creation of a nationwide electronic registry in the USA. This will be supported by an innovative information technology infrastructure that will maximize efficiency through the automated collection and electronic transfer of data. The NROR is supported by the Radiation Oncology Institute and the American Society of Radiation Oncology (ASTRO). Similar nationwide registries have also been planned and established in other countries. The automated collection and electronic transfer of data is a key issue to reduce physician workload and maximize efficiency. In Japan, the Japanese Society for Therapeutic Radiology and Oncology (JASTRO) [15] is planning to develop a similar radiation oncology database.
This registry should be developed with the careful selection of items. The items registered in the database should be standardized and anonymized to protect patient privacy. Moreover, security must be considered when determining the method to link patient data between the registry and hospital identification numbers.
13.4 Standardization
In a radiation oncology system, multiple devices and subsystems are connected to each other. The transfer of information depends upon the coordination between devices. Further, the development of information systems requires standardization for rapid development and ease of integration. Standardization also facilitates preparation and reduces the test time. When standardized devices are used, it is much simpler to replace systems as needed and create request for proposal (RFP) documents.
There are several arguments in favor of standardization:
Easy creation of RFP documents
Shortening of preparation and test times for systems integration
Simple replacement by standardized systems
Increased connectivity between the HIS, PACS, and departmental systems
13.4.1 DICOM-RT
DICOM [16, 17] is widely used in the field of medical imaging and has been extended for use in various subspecialties; DICOM-RT [18, 19] was created for use with radiation therapy. DICOM-RT objects consist of radiotherapy (RT) images (digitally reconstructed radiographs, portal images, and simulation images), RT doses (dose matrix, dose points, isodoses, and dose-volume histograms), RT structure sets (VOIs, dose reference points, and observations/characterizations), RT plans (external and brachytherapy plans, tolerance tables, fractionation, schemes, and patient setup), RT treatment records (beam and brachytherapy session/summary recording information), and RT treatment summary records. DICOM-RT was originally designed for photon radiotherapy but was adopted for particle therapy by Radiotherapy Extensions for Ion Therapy [20].
13.4.2 Integrating the Healthcare Enterprise
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree