Chapter 13 Optic Nerve Diseases
Diseases of the optic nerve are difficult to assess, as tissue diagnosis is usually unavailable. Therefore, various subjective functional tests, such as visual acuity, visual fields and color testing; and objective tests, such as afferent pupillary defect or electrophysiologic evaluation are relied upon to achieve a differential diagnosis. Imaging modalities such as magnetic resonance (MR) imaging and computerized tomography (CT) are utilized to further clarify the diagnosis. Ultrasonographic imaging provides a readily accessible and inexpensive means for diagnosing and monitoring optic nerve disorders.1
Technique
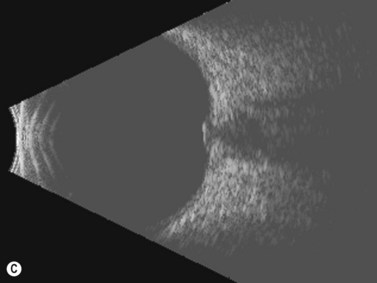
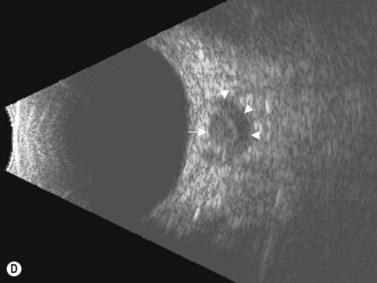
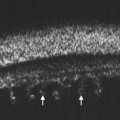
The details of ophthalmic ultrasonographic technique were described elsewhere (Chapter 3). The basic B-scan imaging technique used for the globe is the same for the optic disc and retrobulbar optic nerve.2,3 Specialized A- scan techniques, are used for measuring and evaluating the retrobulbar optic nerve.
Normal retrobulbar optic nerve measurements
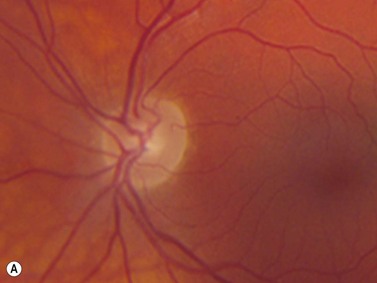
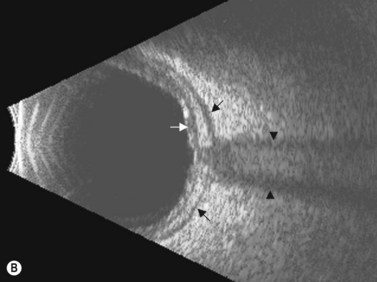
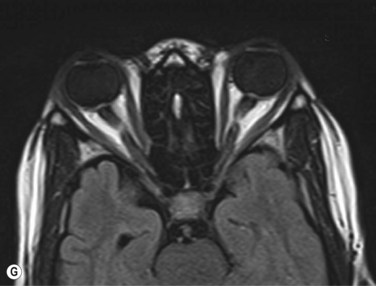
The optic nerves are usually symmetric and measure the same thickness both anteriorly and posteriorly.4 Utilizing ultrasound the optic nerve sheath diameter is measured in two locations, 3 mm posterior to the optic nerve head and as close as possible to the orbital apex (Figure 13.1). Normal retrobulbar optic nerves in an adult measured at the optic nerve sheath are 2.2 to 3.3 mm in diameter.5 Significant variation, can occur in the general population, and it is advised to compare the diameters in both eyes. A difference of 0.5 mm between eyes frequently indicates an abnormal thickness in one eye and should raise suspicion for optic nerve pathology (Figure 13.2).6 There are no significant changes in optic nerve sheath diameter when measured in the Trendelenburg or reverse Trendelenburg position as compared with the supine position in healthy adults.7
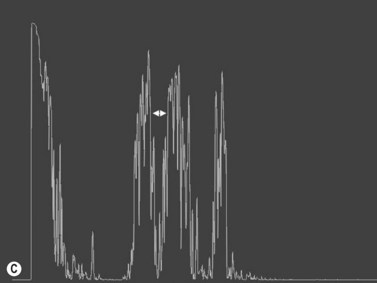
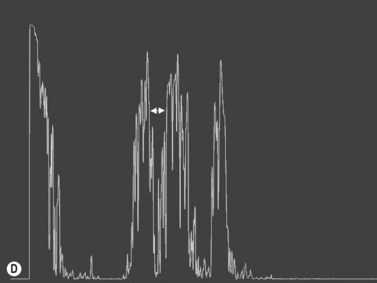
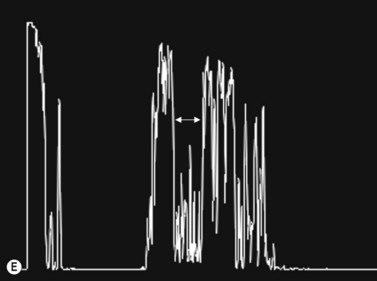
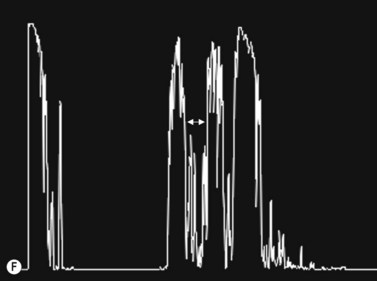
30° test
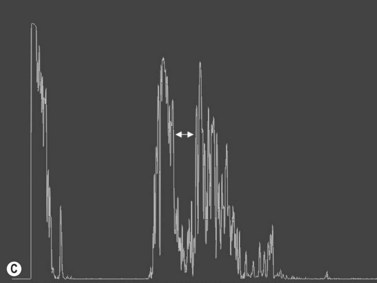
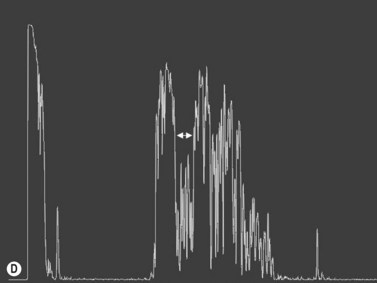
Increased subarachnoid fluid can be differentiated from thickening of the parenchyma or perineural sheaths with a 30° test.8 The patient fixates in primary gaze (straight ahead position), and the optic nerve perineural sheaths are measured anteriorly and posteriorly. The patient’s gaze is then directed 30° laterally, and the perineural sheaths are measured again. The test is based on the premise that when the eye is fixated laterally, the optic nerve sheaths are stretched and the subarachnoid fluid is spread over a larger area. A decrease in sheath diameter of greater than 10% in lateral gaze, as compared with primary gaze, is considered a positive 30° test and thus indicative of increased subarachnoid fluid.
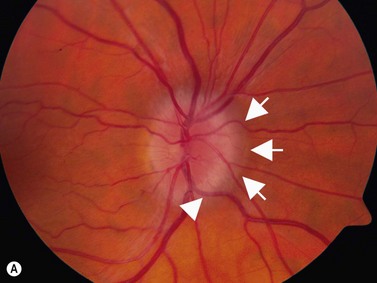
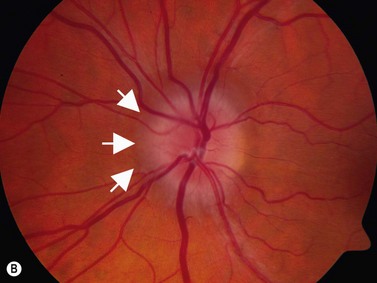
Papilledema
Adults
Blaivas5 performed a prospective observational study on emergency department patients suspected of having elevated intracranial pressure from various intracranial disorders.6 He correlated ultrasonographic measurements of optic nerve sheath diameter with CT scan findings. All cases exhibiting a midline shift of 3 mm or more, collapse of the third ventricle, hydrocephalus, abnormal mesencephalic cisterns, or sulcal effacement were considered to have raised intracranial pressure.6 Such patients were predicted correctly by optic nerve sheath diameters of greater than 5 mm. The ultrasonographic measurements were correlated more closely to the intracranial pathology than the clinical examination. Mean optic nerve sheath diameter for those not meeting CT criteria for raised intracranial pressure was 4.4 mm. Several studies have also shown the efficacy of optic nerve diameter for following hospitalized patients with increased intracranial pressure, regardless of the underlying etiology.6,9–11
Kimberly correlated optic nerve sheath diameters (measured by operators blinded to the measurements) with directly measured intracranial pressure in patients who had invasive intracranial monitors placed as part of their treatment.12 In an adult, optic nerve sheath diameters greater than 5 mm correlated with intracranial pressure greater than 20 cmH2O, with sensitivity of 88% and a specificity of 93%.
Trauma
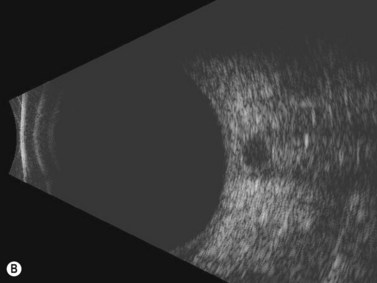
CT scan is the gold standard for evaluating acute head trauma. This, however, is not always available or feasible in the immediate evaluation of trauma. Ophthalmic ultrasonography, combining B-scan and use of the 30° test, can provide a means to triage those who may need surgical intervention for acute increased intracranial pressure (Figure 13.3).
In a year-long, prospective, blinded observational study, Goel evaluated 100 consecutive head trauma patients who presented at an emergency department of a tertiary care institution.13 Their median Glasgow Coma Scale score was 11. Optic nerve sheath diameter using a 7.5 MHz probe was compared with CT scan of the head for evaluation of acute intracranial pressure elevation. Optic nerve sheath diameter of greater than 5 mm was considered to be indicative of increased intracranial pressure. The mean optic nerve sheath diameter in those without increased intracranial pressure was 3.5 ± 0.75 mm. Of 74 patients who had an optic nerve sheath diameter of greater than 5 mm, 59 patients had intracranial hematoma requiring urgent surgical evacuation. Overall, ultrasonography yielded a sensitivity of 98.6% and a specificity of 92.8% for detection of elevated intracranial pressure in this situation.
In another study, Karakitsos observed that optic nerve diameter greater than 5.9 mm at presentation and an increase in nerve diameter of 2.5 mm between repeated measurements was associated with a poor clinical prognosis. Optic nerve monitoring, had a low predictive value for brain death.14
Children
The normal range of optic nerve diameter has also been established for infants and children up to 15 years of age.2,3,10,15,16 In a prospective study of nerve measurements in 102 children admitted to the hospital for diagnoses related to orbital or intracranial disease, but not increased intracranial pressure, range of measured optic nerve sheath diameter was 2.2–4.3 mm (mean 3.08 mm).1 Analysis revealed that the most rapid change in nerve sheath diameter occurred over the first 2 months of life. There was no significant difference between right and left eyes or between the sexes. Analysis of the results found that a sheath diameter of greater than 4 mm in infants under 1 year of age and of greater than 4.5 mm in children age 1 to 15 years should be considered abnormal. Similar normative data have been observed by others.15,16 In those over 15 years of age, mean diameter of greater than 5 mm is considered abnormal and correlates with an intracranial pressure of greater than 20 cmH2O.
Malyeri performed a case-controlled study of 456 hospitalized children between the ages of 1 and 13 years.15
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree