Stefanie C. Thust, Katherine Miszkiel, Indran Davagnanam
Orbit
The Orbit
Introduction
The orbit represents a key element of the visual pathway. Diseases of the orbit, particularly those affecting vision, may be severely debilitating and impact on many aspects of the affected individual’s life. Owing to its complex structure and specialised function, there are several pathologies, which are specific to the orbit. Alternatively, the orbit may be involved in a variety of systemic processes including diseases of the retro-orbital visual pathway.
Orbital Anatomy
The shape of the orbit can be likened to that of an elongated pyramid, whereby the base lies anteriorly and the apex posteriorly. The orbit has four walls: a roof, floor, medial and lateral wall, all of which converge posteriorly at the orbital apex. The medial orbital walls run virtually parallel, but due to the shape of the orbits, their long axes diverge at approximately 45°.1 The roof of the orbit is composed of the frontal bone anteriorly and the lesser wing of sphenoid posteriorly. The orbital roof forms the floor of the frontal sinus and part of the anterior cranial fossa. At the anterior margin of the orbital roof, a small notch or sometimes a complete foramen can be found, which transmits the supraorbital nerve, a branch of the ophthalmic division (V1) of the trigeminal nerve. The floor of the orbit is made up of the zygomatic bone laterally and the maxilla medially, with a small contribution from the orbital process of the palatine bone; it contains a small canal for the infraorbital nerve, a branch of the maxillary division of the trigeminal nerve. The orbital floor forms the roof of the maxillary sinus and is relatively thin, thus susceptible to blow-out fracture or spread of severe sinus infection. The medial orbital wall is composed of several bones (maxilla, frontal, ethmoid, lacrimal and sphenoid) and separates the orbit from the ethmoid air cells. It is a very thin wall, also referred to as the lamina papyracea, and can easily be injured. The lateral wall of the orbit is formed by the frontal and zygomatic bones. It runs obliquely from lateral to medial posteriorly, separating the orbit from the temporal fossa anteriorly and from the middle cranial fossa posteriorly.
The following apertures can be found in the orbit posteriorly: the superior orbital fissure lies between the lateral orbital wall and roof and contains the cranial nerves (CN) III, IV, V1 and VI and the ophthalmic veins, which drain into the cavernous sinus; the optic nerve canal lies at the junction of the roof and medial wall and contains the optic nerve and ophthalmic artery; the inferior orbital fissure lies between the lateral wall and floor of the orbital and contains the infraorbital nerve.
There are six extraocular muscles: namely, four rectus muscles and two oblique muscles. The four rectus muscles arise from the annulus of Zinn, a fibrous tendon ring which surrounds the optic nerve at the orbital apex, and inserts into the globe. The superior oblique muscle runs from the orbital apex to the superior orbital border, where it loops around the trochlea and then passes posteriorly to insert in the globe. The inferior oblique muscle originates anteriorly from the orbital floor and inserts on the back of the globe. The lateral rectus muscle is innervated by the abducens nerve (CN VI) and the superior oblique muscle by the trochlear nerve (CN IV). All other extraocular muscles and also the levator palpebrae are supplied by the oculomotor nerve (CN III). The rectus muscles with their fascial layers form the orbital cone, a landmark which can be used to divide the orbit into three compartments: the extraconal compartment, which comprises all structures peripheral to the cone, the conal compartment and the intraconal compartment, which comprises all structures central to muscle. A compartmental approach is very useful when defining the anatomical location of orbital pathology, as this may significantly narrow the list of potential differentials. Even in cases of a multi-compartmental lesion, defining the epicentre of an abnormality may still be useful.
The orbital septum is an important anatomical boundary, which can be found anterior to the globe. It is an incomplete fibrous membrane continuous with the levator palpebrae superioris superiorly and the tarsus inferiorly and forms a barrier between the orbit and subcutaneous tissues. This can be relevant for the spread of infection.
The globe is divided into three major tissue layers. These are:
The globe is divided by the lens and iris into an anterior chamber filled with aqueous humour and a posterior chamber filled with vitreous humour.
The optic nerve (CN II) consists of four segments: a very short intraocular portion, an intraorbital, intracanalicular and intracranial segment. Embryologically, it is not a true cranial nerve, but rather an extension of brain parenchyma; it is myelinated by oligodendrocytes and not Schwann cells. This explains why pathologies such as gliomas and meningiomas affect the optic nerve, whereas schwannomas and neurofibromas occur in other cranial nerves. Arterial supply to the optic nerve is via the retinal artery (a branch of the ophthalmic artery), which runs inside the nerve to the globe. Further branches of the ophthalmic artery which supply the orbit are the frontal, lacrimal and nasociliary branches. The superior and inferior ophthalmic veins represent the main venous drainage pathways of the orbit.
Imaging of the Orbit
Plain film radiography was historically performed as an initial assessment in suspected bony trauma, but had limited sensitivity and does not reliably assess the intraorbital soft tissues. Ultrasound, including colour Doppler sonography, can be very useful in evaluation of the globe, particularly of the retina and anterior chamber but is also useful in assessing vascularity in ocular tumours and directional flow through the superior ophthalmic veins. However, it has only limited benefit in assessing structures beyond the globe itself.
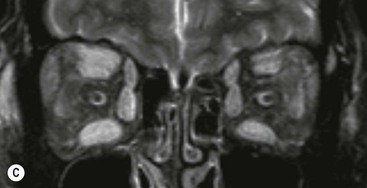
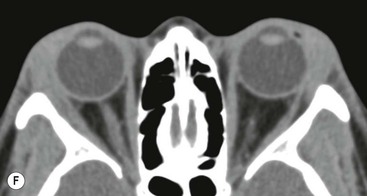
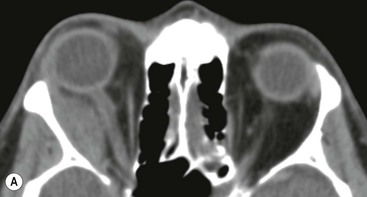
Computed tomography (CT) is readily available at most institutions and offers quick multiplanar orbital imaging. The different densities of orbital structures (bone, fat, muscles and vitreous humour) provide good natural contrast resolution. CT is useful in trauma to identify orbital and periorbital injuries, especially fractures, which are best identified on thin-section multiplanar bone reconstructions. The main role of contrast-enhanced CT of the orbits lies in evaluation of suspected infiltrative, inflammatory and neoplastic disease. Reconstruction is usually performed in the axial, coronal and sagittal planes, both with a soft-tissue and a bone reconstruction algorithm and a slice thickness of 1–3 mm (depending on equipment and local protocol) or less depending on equipment and the clinical question. Axial imaging should be acquired parallel to the orbital axis to allow visualisation of the optic nerve, medial and lateral rectus muscle on a single image. Coronal imaging must be perpendicular to the optic axis.1
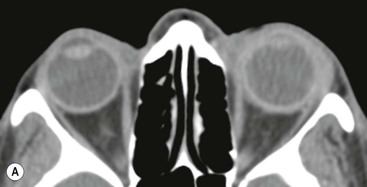
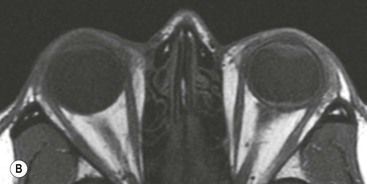
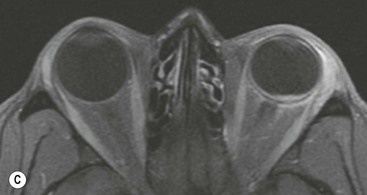
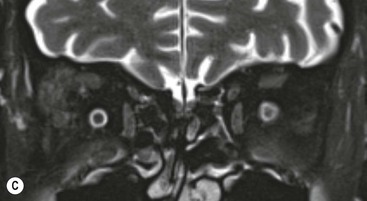
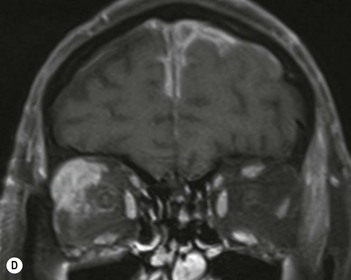
Magnetic resonance imaging (MRI) has superior soft-tissue contrast to CT and is the most accurate technique in characterising orbital mass lesions. Like CT, MRI is capable of multiplanar imaging; however, these require usually separate acquisitions rather than reconstructions in at least two planes (usually axial and coronal). A typical orbital MRI protocol includes pre-contrast T1 and T2 fat-suppressed imaging and post-contrast imaging with at least one fat-suppressed sequence, all at a slice thickness of 3 mm or less. At minimum, a T2 sequence of the whole brain should also be performed to not miss coexisting intracranial pathology.
Orbital Pathology
Congenital Disease
Coats’ Disease
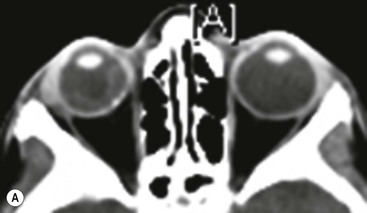
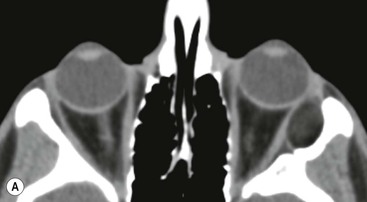
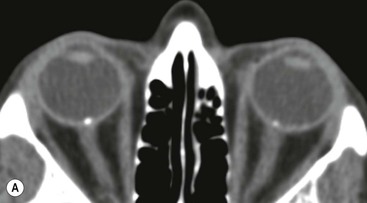
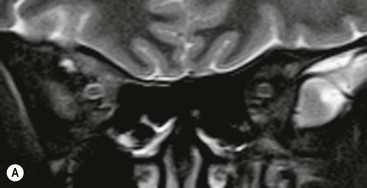
Coats’ disease is a congenital vascular malformation of the retina, which results in telangiectasis and aneurysm formation. Due to endothelial damage, leakage of exudative lipoproteniaceous fluid and blood product into the subretinal space occurs and results in progressive thickening of the retina and subsequent retinal detachment. The disease is usually unilateral and presents in childhood age. The most common presenting feature is leukocoria, but visual impairment, pain, secondary glaucoma and strabismus may occur.2 The nature of the disease is progressive, with loss of vision over a variable length of time. CT findings include increased attenuation along the subretinal space or even filling the entire vitreous. MR imaging may demonstrate increased T1 and T2 signal due to presence of lipoproteinaceous material (Fig. 66-1). There is typically no contrast enhancement.
Persistent Hypertrophic Primary Vitreous (PHPV)
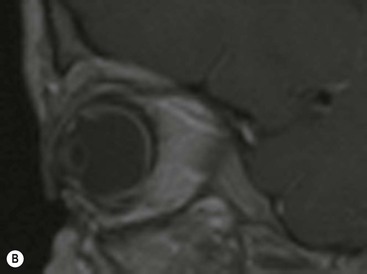
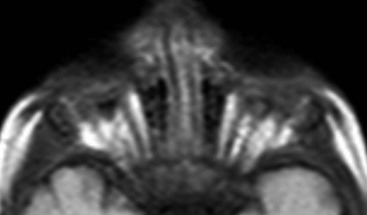
In embryogenesis, the primary vitreous connects the posterior aspect of the lens with the retina. As it is gradually being replaced by the definitive vitreous, the primary vitreous regresses into a band-like fibrovascular structure between the posterior lens surface and retina. A central hyaloid artery can remain present within this. There may be an associated defect in the posterior lens capsule resulting in complications such as lens swelling and destruction or cataract formation. Secondary retinal detachment is common and may appear as a V-shaped structure within the globe on axial imaging (owing to the retina being relatively fixed bilaterally at the ora serrata and posteriorly at the optic disc). Recurrent haemorrhage or glaucoma are indications for enucleation surgery.2 On imaging, PHPV demonstrates a cone or band-shaped structure at the posterior aspect of the lens and is usually associated with microphthalmia. Blood product including fluid–fluid levels within the globe can be present if there has been recent haemorrhage. The presence of a linear septum extending from the lens to the retina is diagnostic (Fig. 66-2). The primary vitreous may demonstrate contrast enhancement. Surgical intervention with preservation of the eye is an option in patients with disease confined to the anterior portion of the globe, but not infrequently PHPV progresses to phthisis bulbi or requires enucleation.
Retinopathy of Prematurity
This has also been termed retrolental fibroplasia and represents a condition which occurs secondary to excessive oxygen therapy to treat premature lungs. This results in the arrested development of the retinal vasculature, which then recommences in a disorganised fashion with the growth of new vessels and fibrous tissue that may contract to cause retinal detachment. With the introduction of surfactant therapy to aid lung maturation, retinopathy of prematurity is becoming less common. Simultaneous periventricular leukomalacia may be encountered on brain imaging.
Coloboma
Congenital coloboma represents an anomaly of the optic nerve head, occurring during development of the eye. This may take the form of small optic pits to colobomas which involve the entire optic disc, the latter known as ‘morning-glory papilla’, and may involve the retina, the choroid/iris and the lids. Diagnostic imaging plays no direct role in the assessment of optic nerve coloboma; however, it may represent an associated finding in CHARGE, Patau’s, Joubert’s or Warburg’s syndrome.
Dermoid
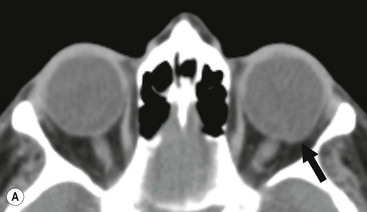
Dermoid cysts are the most common congenital mass lesion of the orbit3 and are usually situated within the extraconal space. They result from inclusion of ectodermal components within the developing orbit and demonstrate slow growth over time with associated bony remodelling or focal erosion. Dermoids are most commonly found at the superolateral orbital margin in the region of the frontozygomatic suture and medially near the frontoethmoidal suture.3,4 They may be an incidental imaging finding; however, symptomatic presentation occurs particularly following rupture. Fatty elements are a useful diagnostic feature on CT and MR imaging; fat-fluid levels or calcification may also be observed (Fig. 66-3).
Disorders of Globe Size or Shape
When assessing ocular size, it is necessary to determine which is the abnormal side taking into account the possibility of bilateral pathology. Macrophthalmia is defined as generalised enlargement of the globe, which can be congenital or acquired. This is most commonly due to myopia, i.e. axial elongation of the globe resulting in convergence of light anterior to the retina with the patient being shortsighted. Macrophthalmia also occurs in collagen vascular disorders such as Marfan’s, Ehlers-Danlos syndrome and homocystinuria.
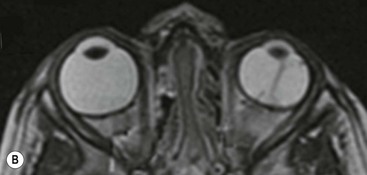
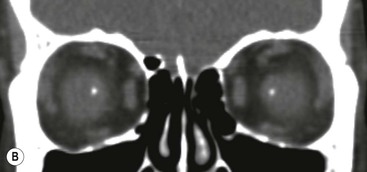
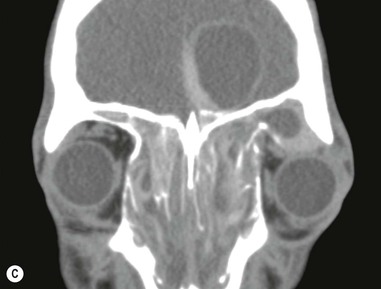
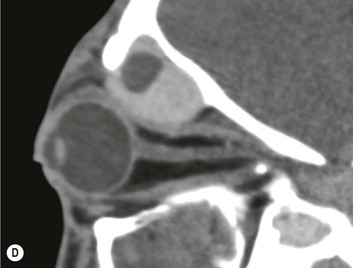
Microphthalmia is defined as a small globe; if this is congenital or acquired in early childhood an associated small bony orbit will be evident on imaging. Causes include PHPV, Coats’ disease, coloboma, previous infection, trauma or radiotherapy and syndromes associated with hemifacial hypoplasia. Anophthalmia refers to complete absence of the embryological formation of an optic vesicle globe in the presence of ocular adnexae, although ‘clinical anophthalmia’ refers to the absence of a clinically identifiable globe on examination or imaging (Fig. 66-4). In some cases, there may be remnants of globe tissue in the orbit only detectable on histological examination.
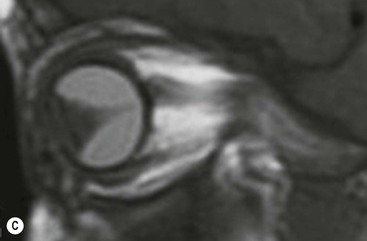
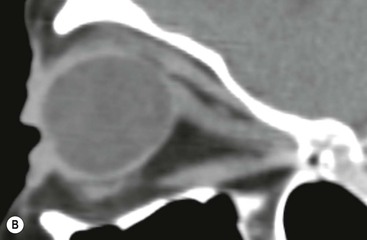
Buphthalmos (bous = Greek for ox, cow) refers to generalised globe enlargement due to increased intraocular pressure, which is typically seen in children rather than adults as the infantile sclera is relatively elastic, allowing the globe to expand under pressure.5 Buphthalmos occurs in paediatric glaucoma and is also seen in association with neurofibromatosis 1 (NF1). Apparent globe enlargement may also be due to exophthalmos secondary to an intraorbital mass; therefore imaging should be mandatory, especially if symptoms are rapidly progressive. Staphyloma is a term used to describe a focal protrusion in the sclera, which can occur anywhere along the globe surface, but is most commonly seen posteriorly on the temporal side of the optic disc.5 The latter is frequently associated with myopia, but staphyloma can also be idiopathic, caused by previous infection, trauma or surgery (Fig. 66-5).
Degenerative Disease
Drusen
Drusen are deposits of lipoproteinaceous material between the basal lamina of the retinal pigment epithelium and the inner collagenous layer of Bruch’s membrane. They are commonly asymptomatic and found as a normal feature in aging eyes but also in association with age-related macular degeneration.6 On funduscopy, drusen can be a cause of blurring of the optic disc margin and hence may be mistaken for papilloedema. The classic CT appearances are those of small punctate and often bilateral calcific foci at the optic nerve heads (Fig. 66-6).
Orbital Inflammatory Disease
Idiopathic Orbital Inflammation
Idiopathic orbital inflammation (also known as idiopathic orbital pseudotumour) is a non-infective disease of unknown cause. Pseudotumour can affect individuals of any age with no clear sex predilection, but most commonly occurs around the fifth decade. It is the most common cause of a painful orbital mass in adults and represents approximately 10% of all orbital mass lesions.7,8 An immune-modulated aetiology has been postulated, and although orbital pseudotumour mostly occurs in isolation, it can be associated with systemic autoimmune inflammatory conditions such as vasculitis and collagen-vascular disorders. Pseudotumour is usually a diagnosis of exclusion, which relies on a combination of clinical and radiological findings. Patients may present with proptosis, chemosis, painful restricted eye movements, diplopia and occasionally associated cranial nerve palsy. The disease often presents acutely, but can be more insidious. Approximately 80% of patients show good response to first-line treatment with steroids.9 Recurrent or chronic pseudotumour may result in fibrosis, which has a worse prognosis. Radiotherapy may be useful in patients who poorly respond to steroids or in those with rapidly progressive disease. Methotrexate is an option in patients who are refractory to conventional treatment.
The anatomical pattern of orbital pseudotumour may vary significantly between individuals. Any orbital structure can be affected; however, the lacrimal gland is most frequently involved.3 A classic feature is tubular enlargement of the extraocular muscles, including the tendon, an important distinction from thyroid orbitopathy, in which the tendon is spared. Unilateral involvement of a single muscle is most common (Fig. 66-7) and in order of frequency this typically affects the medial rectus, superior rectus, lateral rectus and inferior rectus. Manifestation of pseudotumour at the orbital apex and in the cavernous sinus may be indistinguishable on imaging from Tolosa–Hunt syndrome.
CT is mostly sufficient in demonstrating features of orbital pseudotumour such as muscle enlargement, lacrimal gland involvement and infiltration of the orbital fat. However, MRI may be useful in complex cases, particularly if there is concern regarding intracranial extension and to delineate fibrosis, which is characterised by reduced T1 and T2 signal.7
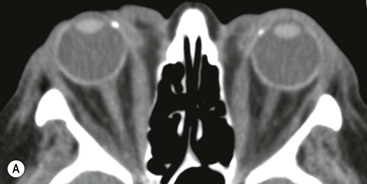
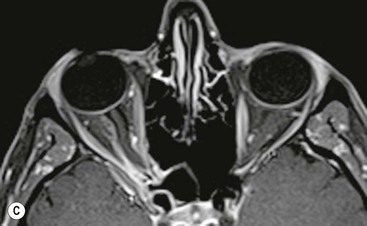
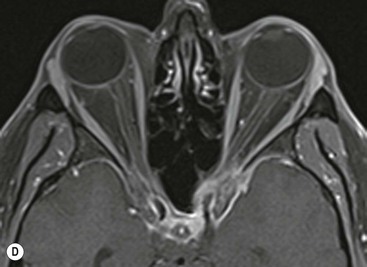
Thyroid Orbitopathy
Thyroid eye disease is an immune-mediated disorder, which most commonly presents in association with hyperthyroidism in Graves’ disease. However, it may be seen in euthyroid or even hypothyroid individuals. Importantly, orbitopathy may precede the actual thyroid disease. Thyroid orbitopathy occurs with a female-to-male ratio of 4 : 1 and a peak in the fourth to fifth decade.4 It is the most common cause of bilateral or unilateral proptosis. Bilateral involvement is the most frequent presentation; in fact in some individuals, ‘unilateral’ proptosis may represent bilateral asymmetrical disease. Histologically, there is deposition of mucopolysaccharides, namely hyaluronic acid, within the extraocular muscles. This results in a classic imaging appearance of fusiform muscle enlargement with sparing of the muscular tendon. In descending order of frequency, the inferior, medial, superior and lateral recti are most commonly affected. Isolated lateral rectus involvement is rare and should prompt consideration of an alternative diagnosis.3 There may be an increase of intraorbital fat, and fat stranding with a ‘dirty’ appearance on imaging (Fig. 66-8).
Systemic Inflammatory Diseases with Orbital Involvement
A variety of systemic autoimmune conditions such as vasculitides, sarcoidosis, connective tissue disorders and inflammatory bowel disease may show associated ocular inflammation. Episcleritis is a benign idiopathic condition which represents inflammation of the superficial sclera layer only. This is usually self-limiting and does not require imaging.10 Scleritis, however, is more serious and can occur either in isolation or associated with a host of autoimmune conditions as listed above. Posterior scleritis may be evident on imaging as scleral thickening (Fig. 66-9) and can result in complications such as necrosis, retinal or choroidal detachment. Uveitis represents inflammation of the vascular layer of the globe and can be seen in both autoimmune disease, for example rheumatoid, seronegative arthropathies and sarcoid but also in infection.10 Retinal vasculitis may result in ischaemia, microaneurysm formation and haemorrhages.11 The majority of pathologies confined to the globe may be more readily appreciated on ophthalmological examination rather than cross-sectional imaging. However, there may be imaging evidence of inflammation in the form of fat infiltration, necrotising features or inflammatory masses.
Sjögren’s syndrome, either in isolation or on a background of rheumatoid arthritis, involves the lacrimal gland and clinically results in dry eyes. Sarcoidosis is a disorder of multisystemic inflammation which commonly affects the respiratory tract, skin and eyes. Ocular involvement occurs in as many as 50–80% of patients and may present as non-caseating granulomas of the conjunctiva, uveitis or lacrimal gland infiltration.12,13 Orbital sarcoid is typically bilateral and tends to respond to steroid treatment. Imaging features may be non-specific, ranging from diffuse infiltration to mass-like appearances (Fig. 66-10). Lacrimal gland enlargement with enhancement is a typical feature.13 Chest imaging may provide a hint to the underlying sarcoidosis, but not infrequently histological sampling is required to conclusively establish the diagnosis.
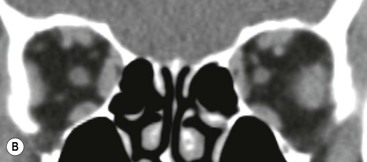
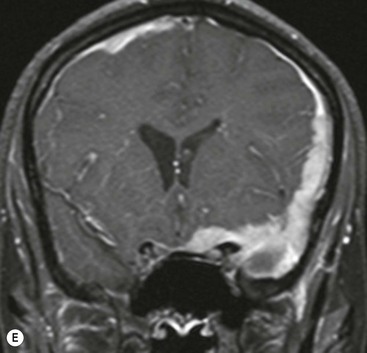
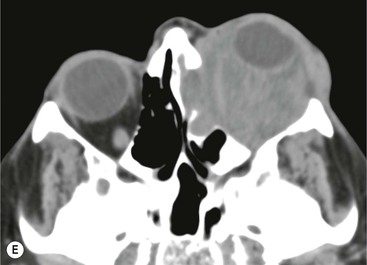
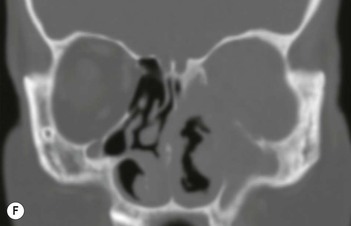
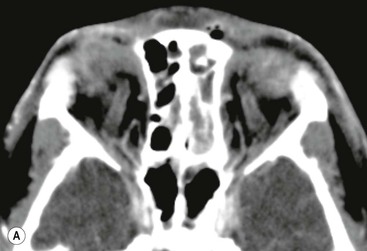
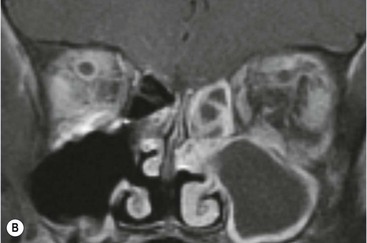
Wegener’s granulomatosis (now known as granulomatosis with polyangiitis) is a multisystem small-vessel necrotising granulomatous vasculitis. This most commonly involves the respiratory tract and the renal system of patients. Involvement of ocular and orbital structures may be present 40–50% of patients.14 Orbital disease is commonly associated with sinus disease with bony erosions (Fig. 66-11). As with other granulomatous disease, orbital disease may appear hypointense on T2 MRI.
Orbital Infection
Toxocara endophthalmitis (also known as ocular larva migrans) results from infection with the nematode Toxocara cani or T. cati via ingestion of eggs in faecally contaminated soil or sandboxes. The source is from domestic dogs or cats. Larvae hatch from the ingested eggs and transgress the human intestinal wall into the bloodstream, whereby they reach various end organs such as the liver, lungs, brain and eyes.15 Infection typically occurs in childhood and ocular disease tends to present between the ages of 5 and 10 years. Toxocara endophthalmitis is the result of a granulomatous immune response to retinal infiltration with larvae. Loss of vision due to retinal detachment is the most common presenting complaint; other non-specific signs include pain, leukocoria and a red eye. Imaging features are mostly non-specific, but the absence of calcification can be a helpful distinguishing feature from retinoblastoma. CT may demonstrate increased attenuation within the vitreous, representing protein leakage from retinal and choroidal vessels.10 MRI signal is variable, especially on T2 sequences, where both hyper- and hypointensity can occur depending on the degree of fibrosis with contrast enhancement usually present.16 Untreated, Toxocara invariably leads to blindness.
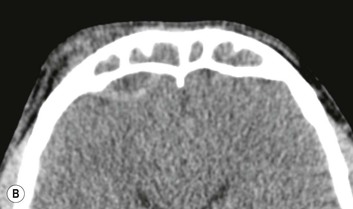
Endophthalmitis can also be fungal (Candida sp.) or bacterial in aetiology with Staphylococcus aureus, Staphylococcus epidermidis, Streptococcus sp. representing the most common pathogens.10 Infectious uveitis may be bacterial, viral, fungal or parasitic (e.g. toxoplasmosis, Lyme disease, leptospirosis) in nature. Orbital tuberculosis is rare, even in endemic areas, and most commonly occurs in children. Clinically, the disease may be indolent with non-specific symptoms, only mild pain and proptosis. The lacrimal gland and orbital walls are most commonly affected, extending from adjacent paranasal sinus inflammatory/infective disease, and can be associated with simultaneous intracranial disease.17 Imaging features include inflammatory soft-tissue masses and retrobulbar or subperiosteal abscess formation (Fig. 66-12).
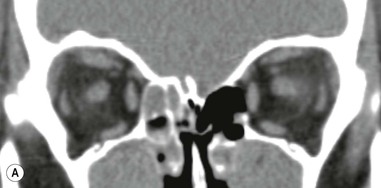
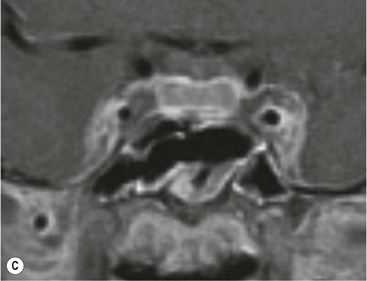
A serious complication of intraorbital infection spread usually via paranasal sinus infection is superior ophthalmic vein thrombosis, which can be further complicated by cavernous sinus thrombosis (Fig. 66-13).
Benign Neoplasms and Mass-Like Lesions
Pleomorphic Adenoma
Pleomorphic adenoma is the most common tumour of the lacrimal gland, comprising over half of all epithelial gland tumours.18 Imaging findings may vary from a homogeneous mass to a more heterogeneous appearance with cystic or necrotic elements. On MRI, small lesions tend to be of relatively uniform low T1 and high T2 signal, whereas larger lesions typically show heterogeneous signal, sometimes also containing haemorrhagic elements (Fig. 66-14). Similar to its behaviour in the parotid gland, lacrimal pleomorphic adenoma has a propensity for malignant transformation, making excision desirable.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree