This article reviews the importance of particular radiologic findings related to facial trauma and their implications for clinical and surgical management. An emphasis is placed on critical imaging signs that warrant immediate surgical attention.
Key points
- •
Knowledge of typical patterns of facial fractures is important because each pattern may be associated with its respective functional complications.
- •
Three-dimensional images are commonly used by surgeons for operative planning in restoration of alignment and correction of cosmetic deformities, but can be occasionally useful to the radiologist as a summary view of complex midface fractures.
Introduction
Traumatic facial fractures are caused most often by motor vehicle accidents, falls, and assaults. At our level I trauma center, the interpretation of facial fractures is routine in daily imaging. By far the most common injuries are the fractures of the midface, followed by fractures of the lower face (mandible) and the upper face (frontal bone and superior orbital rim). The partition of the face into thirds (upper, middle, and lower) has particular relevance for surgical intervention. This article reviews, from cranial to caudal, the most common fracture patterns and the clinical relevance of the imaging findings as they impact patient management.
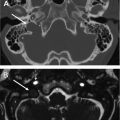
Multidetector computerized tomography (CT) is the imaging study of choice currently used to evaluate acute and nonacute facial trauma. Axial submillimeter bone algorithm images with sagittal, coronal, and three-dimensional reformations are routinely obtained. Occasionally, such as in the detailed evaluation of the orbit, oblique reformations are useful. The three-dimensional images are particularly helpful for the assessment of complex facial deformities, preoperative planning, and patient consultation.
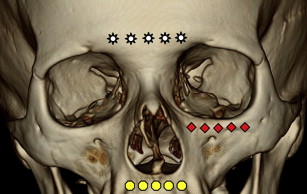
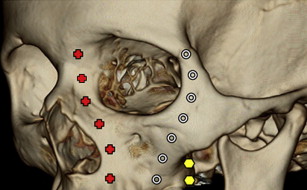
It is well known that traumatic collapse of the face has a “cushion” or “bumper” effect that helps dissipate the impact force and thereby protect the neurocranium and cervical spine. However, the distribution of forces via the areas of thicker bone (facial buttresses) may still be transmitted to the cranial vault and cervical spine. Awareness of the facial buttresses ( Figs. 1 and 2 ) helps with the understanding of the fracture patterns and the identification of osseous segments that require surgical reconstruction for restoration of the normal facial skeleton.
Introduction
Traumatic facial fractures are caused most often by motor vehicle accidents, falls, and assaults. At our level I trauma center, the interpretation of facial fractures is routine in daily imaging. By far the most common injuries are the fractures of the midface, followed by fractures of the lower face (mandible) and the upper face (frontal bone and superior orbital rim). The partition of the face into thirds (upper, middle, and lower) has particular relevance for surgical intervention. This article reviews, from cranial to caudal, the most common fracture patterns and the clinical relevance of the imaging findings as they impact patient management.
Multidetector computerized tomography (CT) is the imaging study of choice currently used to evaluate acute and nonacute facial trauma. Axial submillimeter bone algorithm images with sagittal, coronal, and three-dimensional reformations are routinely obtained. Occasionally, such as in the detailed evaluation of the orbit, oblique reformations are useful. The three-dimensional images are particularly helpful for the assessment of complex facial deformities, preoperative planning, and patient consultation.
It is well known that traumatic collapse of the face has a “cushion” or “bumper” effect that helps dissipate the impact force and thereby protect the neurocranium and cervical spine. However, the distribution of forces via the areas of thicker bone (facial buttresses) may still be transmitted to the cranial vault and cervical spine. Awareness of the facial buttresses ( Figs. 1 and 2 ) helps with the understanding of the fracture patterns and the identification of osseous segments that require surgical reconstruction for restoration of the normal facial skeleton.
Frontal sinus
Fractures of the fronto-orbital bar (frontal boss, tuber frontalis) usually involve the outer table of the frontal bone and sinus ( Fig. 3 ), but they may also involve both tables ( Fig. 4 ). Extension of a frontal sinus fracture into the posterior sinus wall results in communication with the anterior cranial fossa and may be associated with a dural tear and cerebrospinal fluid (CSF) leak. Potential intracranial spread of a pre-existing sinus infection may occur. In addition, these fractures are frequently associated with intracranial hemorrhage.
Isolated fractures of the inner table are uncommon and usually result from an occipital impact. Fractures through the medial aspect of the floor of frontal sinus typically involve the cribriform plate and fovea (roof) ethmoidalis and may result in a dural tear and/or chronic sinusitis. Fractures through the lateral aspect of the frontal sinus floor often involve the orbital roof (see Fig. 4 A), depending on the lateral extent of frontal sinus pneumatization.
Frontal Sinus (Nasofrontal) Outflow Tract
Nasofrontal outflow tract injury is strongly suspected when the CT examination demonstrates involvement of the base of the frontal sinus, the anterior ethmoids, or both ( Fig. 5 ). The posteromedial position of the nasofrontal outflow tract within the sinus makes it particularly susceptible to injury.
Injury to the outflow tract can result in a frontal sinus mucocele and creation of an anaerobic environment with subsequent osteomyelitis and possible intracranial extension leading to a brain abscess. These complications may develop in delayed fashion, years after the inciting trauma.
Management of Frontal Sinus Fractures
A patent frontal sinus outflow tract deems the frontal sinus salvageable and the comminuted outer table is then repaired with plates and screws. If normal frontal sinus drainage pathway cannot be restored, the frontal sinus is surgically eradicated by obliteration or cranialization (ie, the cranial cavity is expanded into the former sinus space). The nasofrontal outflow tract is eliminated with a graft. These procedures are best performed within 2 weeks posttrauma.
Frontal sinus obliteration is best achieved if, after the sinus mucosa is exenterated, the cavity is filled with vascularized pericranial flap (rather than devascularized abdominal fat, muscle, or bone graft). The sinus mucosa is removed to prevent mucocele and subsequent mucopyocele formation.
Fractures that cause significant displacement of the posterior table and/or compromise of the dura are cranialized. The posterior wall of the sinus is removed, the mucosa is meticulously stripped, and the dura and brain are brought to rest against the surgically repaired outer table of calvarium.
The management of frontal sinus fractures has become increasingly conservative because of the accumulated experience and the advent of endoscopic sinus surgery. In the future, follow-up CT to ensure the absence of complications of conservatively managed fractures may likely be more frequently used.
- 1.
Fracture through the frontal sinus base and/or anterior ethmoid implies possible involvement of nasofrontal outflow tract. If sinus patency cannot be restored, the sinus is sacrificed.
- 2.
Involvement of frontal sinus posterior table increases the risk of CSF leak and intracranial infection.
Orbital trauma
Blow-Out Orbital Fractures
An injury involving mainly the orbit is considered at higher risk of ocular trauma and optic nerve injury than orbital involvement by adjacent facial trauma. Isolated orbital fractures most commonly involve the weak medial orbital wall or floor, sparing the orbital rim, lead to enlargement of the orbit, and are known as blow-out fractures ( Fig. 6 ). Enophthalmos can occur with large fragment blow-out fractures and its extent is best appreciated and repaired in delayed fashion, after the edema has resolved.
On CT evaluation, the presence of soft tissue herniation through the defect and the fracture size are important predictors of persistent diplopia. Somewhat surprisingly, small and medium size floor fractures with soft tissue herniation are more likely to cause entrapment than large floor fractures. Any soft tissue incarceration at the fracture site may cause restriction as fibrous septa unite orbital tissue to the sheaths of the inferior rectus and oblique muscles making the diagnosis of entrapment a clinical one. Relatively large orbital floor fractures ( Fig. 7 ) are at less risk for entrapment and, again, operative repair may be delayed.
Blow-In Orbital Fractures
The far less common blow-in fractures occur when the fractures fragments buckle within the orbit leading to a decrease in the orbital volume ( Fig. 8 ). The decreased orbital volume, commonly aggravated by an intraorbital hematoma, leads to proptosis and poses risk of damage to the optic nerve.
Proptosis and Optic Nerve Injury
Orbital fractures are commonly accompanied by a subperiosteal intraorbital hematoma ( Fig. 9 ) and less commonly associated with extensive orbital emphysema ( Fig. 10 ), but both complications can result in proptosis. A large blow-out fracture results in actual decompression of the orbit and obviates the need for surgical hematoma evacuation. Severe proptosis with posterior globe tenting is an ophthalmologic emergency ( Fig. 11 ).
Patients with fractures involving the optic canal ( Fig. 12 ) require vigilant evaluation of the optic nerve because the edema and hematoma can rapidly result in vision loss. In most cases, traumatic optic neuropathy represents a nerve contusion caused by a blow to the superior orbital rim with the force transmitted to the optic canal.
The clinical challenge lies in the timely diagnosis of optic nerve injury to ensure rapid intervention. An afferent pupillary defect may be the only clinically reliable sign of traumatic optic neuropathy because many of these patients have suffered concomitant traumatic brain injury and routine ophthalmologic testing (ie, visual acuity, color vision, and visual field) cannot be easily performed.
Endoscopic surgical decompression is usually reserved for an obvious optic canal hematoma or bone fragment impinging on the nerve. The International Optic Nerve Trauma Study concluded that decompression should be reserved for worsened or not improving visual acuity. In addition, at our institution, the use of steroids for treatment of optic nerve trauma has been abandoned given the questionable benefit and the known morbidity associated with steroid administration.
Complications of Orbital Roof Fractures
Immediately posttrauma, intraorbital herniation of contused brain parenchyma may mimic a subperiosteal hematoma ( Fig. 13 ). Follow-up imaging may reveal a traumatic meningoencephalocele that can be misinterpreted as an orbital neoplasm ( Fig. 14 ).
- 1.
Proptosis resulting in posterior globe tenting is an ophthalmologic emergency.
- 2.
Large fragment blow-out fractures can lead to enophthalmos after the edema subsides.
- 3.
Smaller fragment orbital blow-out fractures are more likely to cause entrapment.
- 4.
Clinical entrapment may occur even in the setting of normal extraocular muscle position and morphology on CT.
- 5.
Fractures involving the optic canal imply a high risk for optic nerve injury. Fragments into the optic canal need to be emergently removed to salvage vision.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree