In the clinical assessment of orbital trauma, visual acuity and extraocular muscle motility are critical for rapid evaluation of injury severity. However, assessment of these parameters may be limited by edema and concomitant injuries. Imaging may further delineate the trauma pattern and extent of injury. This review focuses on orbital soft-tissue injuries that can exist with or without orbital fracture. Imaging techniques and soft-tissue injuries, including those involving the anterior chamber, iris and ciliary body, lens, globe, posterior segment, and optic nerve, are reviewed, in addition to intraocular foreign bodies and cavernous-carotid fistulas.
Key points
- •
Significant morbidity is associated with orbital trauma, including permanent visual loss.
- •
In the clinical assessment of orbital trauma, visual acuity and extraocular muscle motility are critical for rapid evaluation of injury severity.
- •
Assessment of these parameters may be limited by edema and concomitant injuries.
- •
Imaging may further delineate the trauma pattern and extent of injury, and is performed early and often in patients with significant orbital trauma.
Imaging techniques
In patients with orbital trauma, physical examination and history should focus on rapid evaluation of injury severity. Mechanism and timing of injury may provide valuable clinical information in the workup of such patients. Visual acuity testing, intraocular pressure, slit-lamp examination with fluorescein and fundoscopy are helpful for assessment, but may be limited if severe trauma is present or globe rupture is suspected. Visual acuity and extraocular motility are the 2 most important functions to be evaluated emergently. Evaluation of these clinical parameters may be limited by edema and concomitant injuries. Imaging may further delineate the trauma pattern and extent of injury, and is performed early and often in patients with significant orbital trauma.
Imaging techniques
In patients with orbital trauma, physical examination and history should focus on rapid evaluation of injury severity. Mechanism and timing of injury may provide valuable clinical information in the workup of such patients. Visual acuity testing, intraocular pressure, slit-lamp examination with fluorescein and fundoscopy are helpful for assessment, but may be limited if severe trauma is present or globe rupture is suspected. Visual acuity and extraocular motility are the 2 most important functions to be evaluated emergently. Evaluation of these clinical parameters may be limited by edema and concomitant injuries. Imaging may further delineate the trauma pattern and extent of injury, and is performed early and often in patients with significant orbital trauma.
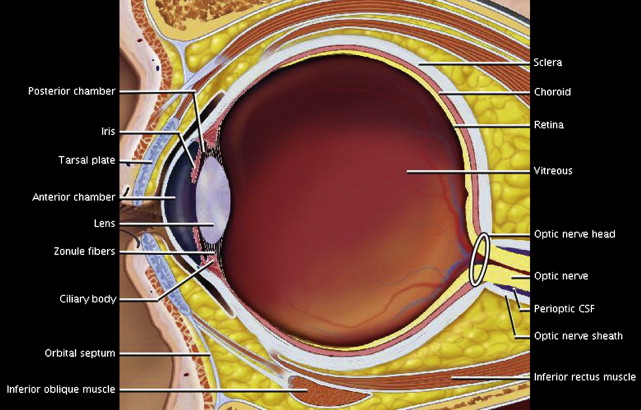
Orbital anatomy
Familiarity with normal orbital anatomy is important for the interpretation of trauma studies ( Fig. 1 ). The globe is a spherical 2- to 3-cm structure with 3 concentric layers: the outer sclera, the vascular choroid, and inner retina, continuous with the optic nerve. The sclera blends into the cornea and is covered by the translucent conjunctiva ventrally. The uvea describes the middle layer and consists of the choroid, ciliary body, and iris. The globe can be separated into the anterior and posterior segments by the lens. The anterior segment is further subdivided into the anterior and posterior chamber by the iris; aqueous humor is produced by the ciliary body and flows to the anterior chamber. The lens is suspended by zonule fibers, and muscular contractions of the ciliary body result in lens deformity. The posterior segment contains gelatinous vitreous humor.
Choice of imaging
Radiology plays a critical role in the diagnosis and treatment planning of traumatic orbital injuries. Imaging may be indicated if the posterior chamber is not visualized on ophthalmologic examination, or if there is clinical concern for orbital fracture, intraocular foreign body, or occult globe rupture. Computed tomography (CT) is typically the first-line modality, given its rapid acquisition and availability; however, other modalities may have distinct advantages.
Radiography
The role of conventional radiographs has diminished significantly, given the current availability of CT. Standard Caldwell (orbitofrontal view; beam tilted 15–20° caudal) and Waters (occipitomental view; chin raised) views have sensitivities ranging from 64% to 78% for detection of orbital fractures, with false-negative findings in 9% to 29%. Given the moderate sensitivity and false negatives, plain films have limited clinical utility.
Computed Tomography
CT has become the first-line imaging study in patients with ocular trauma. Rapid acquisition and thin-section multiplanar reformations of CT allow for accurate assessment of orbital fracture and associated injuries. CT demonstrates a high sensitivity for fracture detection that is optimized by thin-section acquisition, multiplanar reformations, and 3-dimensional modeling. Furthermore, for polytrauma cranial evaluation can be performed concurrently with CT imaging.
Although CT is very sensitive for detection of orbital fracture, its accuracy in soft-tissue injuries may be more limited. In a study from 2000, CT demonstrated 73% sensitivity and 95% specificity for the detection of open-globe injury. Magnetic resonance (MR) imaging holds significant advantages for the assessment of retinal and choroidal detachments and nonradiopaque foreign bodies.
The lens is a radiosensitive organ, and efforts should be made to limit the radiation delivered. Modern multidetector helical CT scanning techniques demonstrate significant benefit in dose reduction over older single-detector setups. There is evidence that limiting the tube current to 100 mA instead of the conventional 300 mA setting may decrease the effective dose by 70% without compromising detection of traumatic injury.
Ultrasonography
Ultrasonography can be performed rapidly at the bedside, and appears to provide accurate detection of retrobulbar hemorrhage, foreign body, lens dislocation, and retinal detachment. However, it is contraindicated in the setting of globe rupture because of the pressure applied during sonographic assessment, possibly exacerbating an unstable globe. Although ultrasonography is limited in the assessment of complex facial fractures, it appears to provide accuracy comparable with that of CT in the detection of fractures of the infraorbital rim and orbital floor.
MR Imaging
In the acute presentation of ocular trauma, MR imaging has limited utility because of its longer acquisition time and decreased sensitivity for fracture in comparison with CT. Furthermore, MR imaging is contraindicated if a metallic ocular foreign body is suspected. MR imaging holds significant advantages in the detection of organic foreign bodies (eg, wood).
Anterior chamber injuries
The anterior chamber is located between the cornea and iris and contains aqueous fluid. Clinically and by imaging, the anterior chamber should be assessed for the presence of abnormal material (eg, blood, foreign body) and abnormal depth. Deepening of the anterior chamber may result from lens dislocation, scleral rupture, or iridodialysis (rupture of the iris–ciliary body attachments). The anterior chamber may be abnormally shallow as a result of lens dislocation, corneal injury, choroidal hemorrhage, or acute angle closure.
Anterior chamber depth (ACD) on CT appears to correspond with open-globe injury. An asymmetric difference in ACD of 0.4 mm or greater has 73% sensitivity and 100% specificity for detection of open-globe injury. Corneal laceration may result in decreased ACD ( Fig. 2 ) and may be accompanied by iris prolapse. Anterior lens dislocation may mimic traumatic corneal laceration, and the lens should be carefully examined.
Traumatic Hyphema
A traumatic hyphema is caused by bleeding in the anterior chamber secondary to disruption of blood vessels in the iris or ciliary body. A blood-aqueous level may be apparent on inspection, and increased intraocular pressure may result. Rebleeding may occur in 20% of patients, typically 2 to 5 days following injury when the initial clot retracts. Clinically it is important to assess for a bleeding diathesis, such as sickle cell disease, which can significantly increase the severity of the hyphema and the likelihood and rate of rebleed. Hyphema may be classified in 4 grades, the most significant being an “8-ball hyphema” resulting from an anterior chamber completely filled with hemorrhage. More than half of traumatic hyphemas are the result of sports-related injuries. Imaging is not required for the diagnosis of traumatic hyphema but is frequently performed to assess for more significant injury. The hyphema is manifested on orbital CT by increased attenuation in the anterior chamber. Disruption of these same iris and ciliary vessels may result in bleeding into the posterior chamber, a vitreous hemorrhage (see later discussion).
Subconjunctival Hemorrhage
Subconjunctival hemorrhage may occur from minor trauma such as sneezing, coughing, or Valsalva, and results from tearing of small subconjunctival blood vessels. The dramatic appearance may bring patients to medical attention when a painless, red conjunctival lesion is evident. The area should not be raised, and visual acuity should be preserved. Cross-sectional imaging is not necessary, and the hemorrhage is self-limited.
Injury to iris and ciliary bodies
Injuries to the iris and ciliary bodies are typically assessed on clinical examination. Thorough evaluation of the iris and ciliary body is performed with a mirror/prism (gonioscope) in conjunction with a slit lamp to evaluate the iridocorneal angle. Cross-sectional imaging may be normal, unless associated vascular injury is present with anterior and/or posterior chamber hemorrhage.
Traumatic iridocyclitis results from blunt trauma to the iris and ciliary body that may cause spasm and blurry vision. This condition is typically self-limited; short-term cycloplegic (dilating and paralyzing) therapy may be given. Traumatic mydriasis and miosis result from similar traumatic injury to the iris sphincter. Although this condition is self-limited, imaging may be performed to exclude cranial nerve injury as the underlying cause. Traumatic iridodialysis is the result of a tear in the peripheral iris resulting in separation of the iris and ciliary body.
Glaucoma can result from traumatic obstruction of aqueous outflow from blood (hyphema), disruption of the trabecular meshwork, or lens dislocation. Delayed-onset glaucoma can occur from angle recession, lens dislocation, or various hemolytic manifestations. Delayed glaucoma is also seen following open-globe injury, owing to formation of synechiae.
Lens injuries
Subluxation and Dislocation
The zonule fibers responsible for holding the lens in place may be disrupted by blunt trauma, resulting in lens detachment. Patients will clinically display blurred vision, monocular diplopia, or distortion if partial lens dislocation is present. Most commonly the lens will dislocate posteriorly because the iris prevents anterior translation. However, anterior lens dislocations can occur, and may mimic decreased ACD caused by corneal laceration. Anterior lens dislocation may also result in acute angle closure glaucoma by mechanical obstruction of aqueous outflow, a condition requiring emergent ophthalmologic attention.
With complete dislocation, the lens is typically displaced posteriorly and lies dependently within the vitreous humor ( Fig. 3 ). When the zonule fibers partially tear, there is asymmetric displacement of the lens away from the ruptured ciliary attachments and posterior displacement into the vitreous humor ( Fig. 4 ).
Trauma is the most common cause of lens dislocation, but bilateral nontraumatic subluxations may be seen with Ehlers-Danlos syndrome, Weill-Marchesani syndrome, aniridia, homocystinuria, and Marfan syndrome.
Traumatic Cataract
The lens capsule normally maintains a dehydrated environment. When the capsule is disrupted, the lens may absorb fluid and swell. This condition manifests clinically as a cloudy edematous lens and is demonstrated on CT by unilateral lens hypoattenuation, a finding specific for traumatic cataract ( Fig. 5 ). A decrease in attenuation of 30 HU may be seen in the abnormal lens. Treatment is surgical lens replacement. The pathophysiology of traumatic cataract is similar to that of osmotic cataract seen with hyperglycemia, in which elevated glucose in the aqueous humor creates an osmotic gradient that draws fluid into the lens; however, this finding is bilateral in diabetic hyperglycemia.
Globe injuries
Globe Rupture
Open-globe injury, or globe rupture, is a surgical emergency because of the risk of endophthalmitis and the associated high rate of monocular blindness. The standard practice of ophthalmologists worldwide is to undertake a primary surgical repair to restore the structural integrity of the globe. This action is best undertaken at the earliest opportunity, regardless of the extent of the injury and the presenting visual acuity. Although diagnosis of an open-globe injury is obvious when intraocular contents are visualized on ophthalmologic examination, it can be challenging when a patient is unable or unwilling to cooperate, or if severe facial injuries make examination unsafe.
CT is the imaging test of choice for the diagnosis of an open-globe injury and assessment for associated injuries. Findings include a change in globe contour with an obvious loss of volume (“flat-tire” sign), scleral discontinuity, intraocular air, and intraocular foreign body ( Figs. 6 and 7 ). Absent or dislocated lens, vitreous hemorrhage, and retinal detachment are additional predictors of open-globe injury. In a review of 46 patients who underwent surgical exploration, moderate to severe change in globe contour (flattening or concavity of the sclera in at least 1 quadrant), obvious volume loss, total vitreous hemorrhage, and absence of lens were seen only in eyes with globe rupture.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree