Clinical Presentation
The patient is a 69-year-old female with a several-year history of progressive gait difficulty. She presently uses a wheelchair for longer distances outside the home and also a single point cane. She tends to lean on objects when she is walking because of her unsteadiness. Her gait problems have been evolving over the last 5 to 7 years. She reports acute hemiparesis involving the left face and upper and lower limbs. She says that she was diagnosed as having had a stroke and that similar recurrent spells have happened since then, lasting up to 2 hours. She has a continuing sense of tightness involving the right lower extremity that began in the distal leg and foot and now extends up to the knee with intermittent pins-and-needles sensation in the right lower limb. Sensory symptoms do not occur in the left lower extremity. She also feels that the right lower extremity is weak and that, in general, the lower extremity weakness bilaterally has gradually worsened.
Imaging Presentation
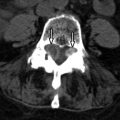
Sagittal T1- and T2-weighted images demonstrate flowing intermediate T1/decreased, T2 signal intensity along the posterior aspect of the vertebral bodies from C3-C7 causing moderate narrowing of the central spinal canal in the midline ( Fig. 53-1 ) .

Discussion
Ossification of the posterior longitudinal ligament (OPLL) is a condition in which there is pathologic ossification of this ligament in the cervical and/or thoracic spine. If this ossification occupies enough of the spinal canal, then this condition can result in myelopathy and/or radiculopathy secondary to chronic pressure on the spinal cord and nerve roots.
The posterior longitudinal ligament (PLL) is a band of collagen and elastin fibers that extends along a line along the posterior margins of the vertebral bodies from the atlas to the sacrum. The PLL is narrower and weaker than the anterior longitudinal ligament (ALL), which extends along the anterior margins of the vertebral bodies, also from the atlas to the sacrum. The fibers of both of these ligaments are firmly attached to the annulus of the intervertebral discs and the corner of the vertebral bodies. The ligament is widest at the disc spaces and narrowest at the mid-vertebral levels. The ligament is also thicker centrally and progressively thins out laterally.
With OPLL, there is initial hypertrophy of the ligament secondary to fibroblastic hyperplasia, which is followed by an increase in collagen deposition. Progressive mineralization and cartilaginous ingrowth form ossification centers that eventually result in formation of haversian canals.
OPLL usually occurs in patients over 40 years of age and is very rare until the third decade. OPLL has been well studied in East Asian countries with an incidence of 2% to 4%. The prevalence of OPLL in other countries has not been well studied. OPLL has been estimated to have a prevalence of 0.12% in a radiology review. One quarter of North Americans and Japanese patients with cervical myelopathy exhibit OPLL. Most often, OPLL is found in the upper cervical spine (70%, C2-C4) and less often in the upper thoracic spine (15%, T1-T4). Cervical OPLL occurs twice as often in males as in females.
OPLL can be divided into four different patterns: (1) focal ossification at the posterior margin of the vertebral body; (2) segmental ossification, where each ossification does not extend beyond the adjacent disc level; (3) continuous or flowing ossification across several levels; and (4) mixed ossification, where there is a combination of segmental and continuous OPLL.
Most patients with OPLL are asymptomatic. Matsunaga and colleagues followed 359 patients with documented OPLL for 10 years. Of those, 323 patients at the onset of the study had no myelopathic symptoms and the remaining 36 did. Seventeen percent of those without myelopathy were treated conservatively and developed myelopathy during the follow-up period. Sixty-four percent of the patients who began with a myelopathy and declined surgery worsened. The authors concluded that if a patient was discovered to have OPLL without myelopathy, that prophylactic surgery was not necessary because of the slow progression of OPLL.
Imaging Features
Plain radiographs can demonstrate the ossification of OPLL behind the vertebral bodies; however, it can easily be overlooked and/or masked by the superimposed facet joint complex on the lateral radiograph ( Fig. 53-2 ) . Advanced imaging (computed tomography [CT], magnetic resonance [MR] imaging) is necessary to depict the degree of spinal canal stenosis and the effect of OPLL on the spinal cord. CT scanning with sagittal reformats demonstrates the dense cortical bone of OPLL ( Fig. 53-3 ) . A lower density marrow cavity may also be evident. On axial imaging, the ossification may have a “bow-tie” or “upside down T” appearance ( Fig. 53-4 ) . Although CT can depict the degree of central canal narrowing, MR is necessary to demonstrate the effect of OPLL on the spinal cord if there are any signal changes in the spinal cord to suggest cord compromise ( Fig. 53-5 ) . CT is often performed in conjunction with MR if surgery is contemplated because MR can overestimate the actual degree of spinal canal compromise. MR can demonstrate the flowing ossification of OPLL on sagittal images as well as the “bow-tie” or “upside down T” appearance. The dense cortical bone of mature OPLL is of decreased T1 and T2 signal intensity. However, increased T1 and T2 signal intensity will be seen where OPLL has acquired a marrow cavity. Furthermore, there may be increased signal intensity on T2-weighted acquisitions within the spinal cord secondary to spinal cord edema, ischemia, or infarction.