, Leonid Tiutin2 and Thomas Schwarz3
(1)
Russian Research Center for Radiology and Surgery, St. Petersburg, Russia
(2)
Department of Radiology and Nuclear Medicine, Russian Research Center for Radiology, St. Petersburg, Russia
(3)
Department of Nuclear Medicine Division of Radiology, Medical University Graz, Graz, Austria
Abstract
Ovarian cancer is the fifth most frequent cause of death from oncologic diseases in women. Ovarian cancer is notable for unsatisfactory treatment outcomes due to the asymptomatic course of the disease and, in consequence, late diagnosis. This disease is characterized by rapid growth with subsequent spread to adjacent organs, dissemination through the organs of the small pelvis and abdominal cavity, and extensive lymphogenic and hematogenic metastasis. The probability of tumor recurrence in the third to fourth stages reaches 96% of cases within 6 months to 2 years after the end of primary treatment.
Ovarian cancer is the fifth most frequent cause of death from oncologic diseases in women. Ovarian cancer is notable for unsatisfactory treatment outcomes due to the asymptomatic course of the disease and, in consequence, late diagnosis. This disease is characterized by rapid growth with subsequent spread to adjacent organs, dissemination through the organs of the small pelvis and abdominal cavity, and extensive lymphogenic and hematogenic metastasis. The probability of tumor recurrence in the third to fourth stages reaches 96% of cases within 6 months to 2 years after the end of primary treatment.
Ovarian cancer is observed mainly in women over 40 years old. Among the causes of developing the disease are: hereditary predisposition, continuous inflammatory processes in the uterine appendages or surgeries of benign tumors. Pregnancy decreases the risk of developing ovarian cancer, and infertility, on the contrary, increases the probability of its emergence. Environmental factors matter too.
Ovarian cancer classification is rather complex; it is based on numerous signs: dissemination, histological type, premorbid background, etc. Primary ovarian cancer originates from unchanged epithelial tissue. Secondary cancer develops in consequence of transformation of benign neoplasms. Metastatic cancer results from dissemination of malignant tumors of other localizations (endometrial, mammary or gastrointestinal cancers). Secondary ovarian cancer develops in consequence of malignization of cilio-epithelial cystomas, pseudomucinous cystomas, dermoid cysts, primary sex cord-stromal tumors, including granulosa cell tumors, androblastomas, thecomas.
On the basis of histological signs, three main groups of malignant ovarian tumors are distinguished: epithelial, germinogenic and stromal tumors. The overwhelming majority of malignant ovarian tumors are of the epithelial origin (from the integumentary epithelium of the ovary). They are divided into serous, mucinous, endometrioid, clear cell mesonephroid, Brenner tumors, mixed tumors of the epithelial origin, and undifferentiated tumors. Malignant growth characterizes also virilizing Leydig and Sertoli cell tumors and tumors of germinogenic origin: dysgerminomas, chorionepitheliomas, and immature teratomas. The most aggressive tumors are those of germinogenic origin, most of all chorionepitheliomas, the most rapid-growing and metastasizing tumors.
The FIGO system is a generally accepted classification reflecting stages of the disease. In the first stage, the tumor is confined to the ovary. The second stage is characterized by lesion of the ovaries and injury of their capsule. In the third stage, the tumor spreads through the peritoneum and there are lesions of the retroperitoneal and inguinal lymph nodes, of the surface of the liver and omentum. The fourth stage is characterized by the presence of remote metastases.
Ovarian cancer metastases through the peritoneal leafs, mainly with serous liquid; therefore metastases are most often localized in the interior walls of the abdominal cavity, especially the subphrenic space on the right as well as the greater omentum. Also, tumor dissemination occurs via the lymphogenic route, with tumor spreading to paraaortal and paracaval lymph nodes, those of the uterine broad ligament and pelvis, including the external iliac, obturator and epigastric groups. More seldomly, the tumor may spread to lymph nodes along the round ligament of the uterus, affecting the inguinal lymph nodes. In a late stage of the disease, sometimes secondary lesion of retroperitoneal lymph nodes is observed. Hematogenic metastases of ovarian cancer are observed very seldomly, mainly in the liver and lungs.
In the so-called preclinical stage of cancer development, any symptoms whatsoever are absent. Enlargement of the abdomen in consequence of ascites, pain syndrome, uterine hemorrhage, intestinal and dysuric disorders indicate tumor dissemination. In the preclinical stage, ovarian cancer is often detected accidentally during prophylactic gynecologic examination.
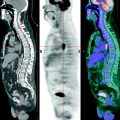
12.1 Methods of Diagnosis
Examining a patient suspected of ovarian cancer begins with internal gynecologic examination, with simultaneous mirror examination of the vagina and uterine cervix. The determination of the tumor marker CA-125 in blood has diagnostic significance, since its content in blood significantly increases in presence of ovarian cancer. US is the widest-spread and most available method of radiologic visualization for ovarian cancer. Use of transabdominal US has significantly increased the efficiency of diagnosis of ovarian masses compared with manual gynecologic examination, and introduction of transvaginal, rectal and intravaginal sensors with high resolving capacity extends the prospects of ultrasonography. The accuracy of US diagnosis is 85–94%. Further, some of its advantages are: rapidity and simplicity of examination, safety for the patients and for the diagnostician, painlessness, and the possibility of repeated dynamic observation. CT and MRI are also applied in this field. They permit assessment of the size of the mass, its relation with adjacent organs and tumor dissemination. The diagnostic value of these visualization methods is roughly the same as that in endometrial and cervical tumors. Unlike CT, the high sensitivity of MRI shows itself in imaging soft tissues.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree