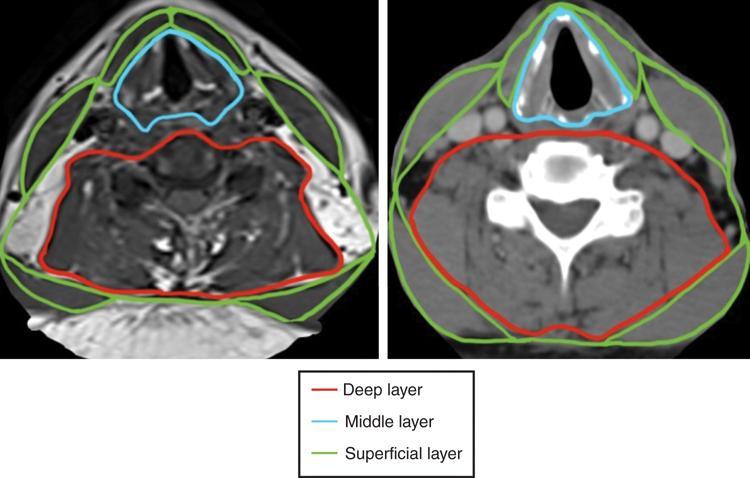
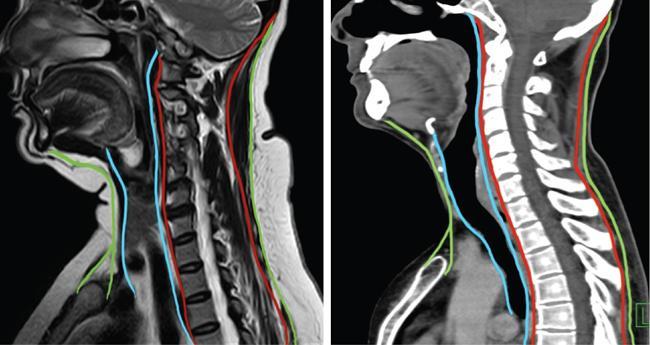
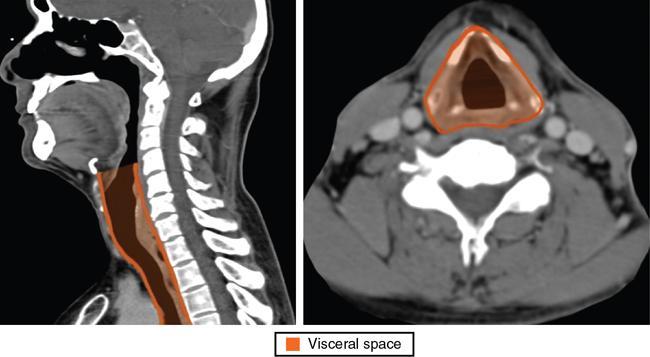
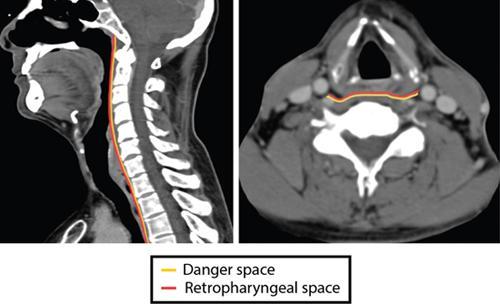
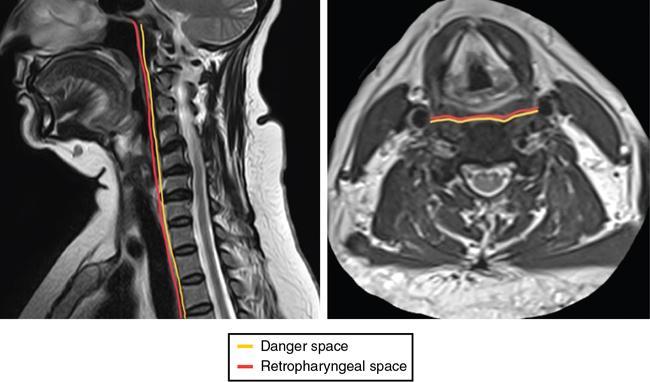
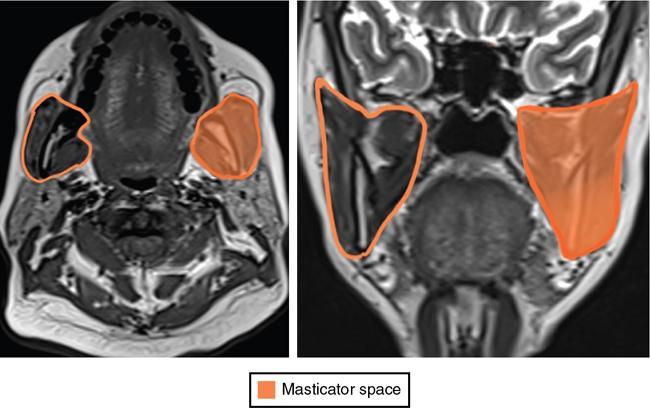
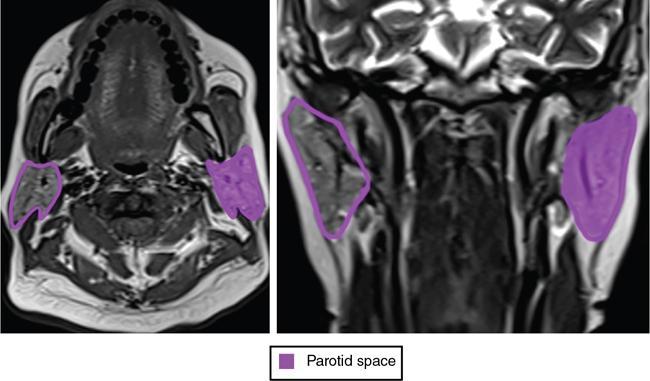
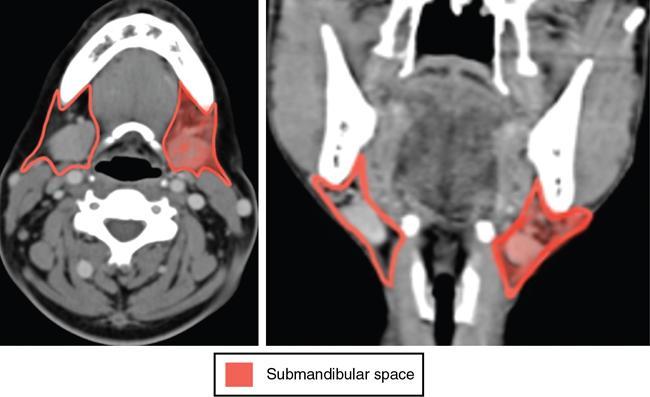
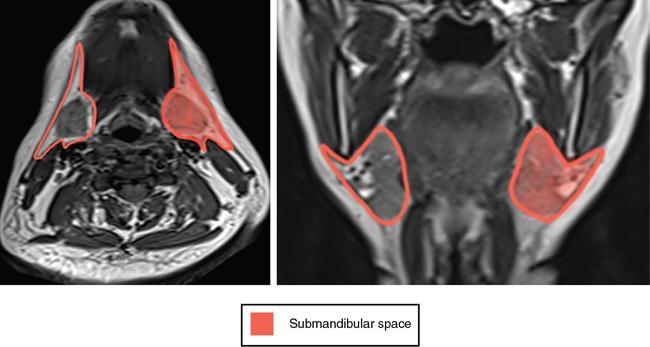
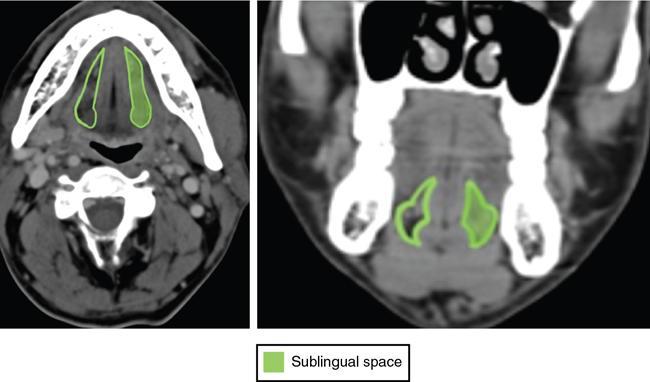
G. Suganya, Seetharaman C, S.P. Rajesh Accurate interpretation of head and neck imaging requires an understanding of fascial layers and its location, extent and span – the superficial and deep cervical fascia. This concept can be used to formulate differential diagnosis, determine the extent of disease and facilitate surgical and therapy planning. The superficial cervical fascia envelops the fat, loose connective tissue, the platysma, the external jugular veins and subcutaneous nerves. The deep cervical fascia is further divided into three layers. The superficial layer of the deep cervical fascia (SLDCF), the middle layer (MLDCF) and the deep layer (DLDCF). The SLDVF also known as the investing layer forms a complete collar around the neck and envelops the sternocleidomastoid and trapezius muscles. It attaches to the skull base superiorly; mandible and hyoid anteriorly; clavicle, sternum and scapula inferiorly. The two halves of the fascia attach posteriorly to the ligamentum nuchae and cervical spinous process (Fig. 3.2.1). The superficial layer of DCF splits to enclose the muscles of mastication forming the masticator space. It also divides to form the capsule of the parotid gland, forming the parotid space. The submandibular space and sublingual spaces are also enclosed by the superficial layer but divided by the mylohyoid muscle (Fig. 3.2.2). The MLDCF is also known as the visceral or pretracheal layer. It continues as the buccopharyngeal fascia in the suprahyoid neck and encloses the nasopharynx and oropharynx. In the infrahyoid neck, it envelops the trachea, esophagus, larynx, thyroid and parathyroid glands (visceral space). The fascia splits anteriorly to enclose the sternohyoid and sternothyroid muscles, and the posterior split encloses the thyroid gland (Fig. 3.2.3). The pharyngeal mucosal space is the area of the nasopharynx and oropharynx on the inner side of buccopharyngeal fascia, and the parapharyngeal space lies lateral to the buccopharyngeal fascia. The retropharyngeal space lies behind the pharynx (buccopharyngeal fascia) and anterior to the prevertebral fascia (DLDCF) and extends from skull base to T4 vertebral level. The DLDCF is also known as the perivertebral fascia. The deep layer splits into two layers – anterolateral alar slip (alar fascia) and posterior pre (peri) vertebral layer, and the space in between the two is the danger space. The prevertebral space lies posterior to the posterior prevertebral slip of the deep layer. Both the retropharyngeal space and the danger space extend from the base of the skull to the mediastinum. The retropharyngeal space ends at the level of T4, while the danger space continues till the level of the diaphragm (Figs 3.2.4 and 3.2.5). There are four distinct spaces between the pharynx and the vertebral bodies from anterior to the posterior – visceral space, retropharyngeal space, danger space and the prevertebral space (separated by three named fascia as described before) (Fig. 3.2.6). The masticator space are paired suprahyoid cervical spaces on each side of the face that extend from the angle of mandible to parietal calvarium. The SLDCF splits to enclose the muscles of mastication and forms the border of this space. The superior extent of the lateral layer attaches to zygomatic arch and then extends to the suprazygomatic area to the parietal calvarium enclosing the temporalis muscle (also called temporalis fascia at this level). The medial layer encloses the pterygoids (pterygoid fascia) and extends superiorly to attach to the skull base, medial to the foramen ovale. The contents of this space are therefore the muscles of mastication, ramus of mandible and third division of the fifth nerve (mandibular nerve). The mandibular ramus, posterior margin of maxilla, pterygoid plates, skull base bones and zygomatic arch are within and closely related to this space (Fig. 3.2.7). Inflammatory conditions of the space are particularly common and are usually odontogenic in origin, in view of close relationship of teeth bearing part of maxilla and mandible. Lymphovascular malformations are also common, particularly in children. Benign and malignant tumours may arise from different contents of the space – nerve sheath tumours, lipomas, mandibular and soft-tissue sarcomas and dental tumours. In children, rhabdomyosarcoma may also arise in this space. Tumours of the pharynx and parotid gland may also invade the masticator space (Fig. 3.2.8). The parotid space is circumscribed by the superficial layer of the deep cervical fascia. It is bounded superiorly by the external auditory canal and apex of mastoid process, inferiorly by the inferior mandibular margin and anteriorly by the masticator space. The contents of this space are the parotid gland, intraparotid lymph nodes, intraparotid facial nerve, retromandibular vein and external carotid artery (Fig. 3.2.9). Evaluation of a mass within the parotid region begins with a determination of the lesion as intraparotid or extraparotid. Intraparotid masses displace the parapharyngeal fat medially and cause widening of the stylomandibular notch. Lesion in the parotid space include – Benign and malignant tumour of parotid glandular tissue, inflammation, infection, calculus and duct-related diseases, autoimmune disorders and pathology related to immunocompromised status. In children, 50% of the parotid lesions are haemangioma, and other lesions include lipoma, first branchial cleft cyst and rarely schwannoma. In view of the late embryological encapsulation of parotid glands, the lymphoid tissue is incorporated, resulting in formation of intraparotid lymph nodes, which drain the parotid and external auditory canal area. Therefore, other disorders such as lymphoma and metastases can also occur within the parotid gland. The submandibular space and the sublingual space are divided by the mylohyoid muscle. Submandibular “space” is actually a muscular triangle. It is bounded superiorly by the mandible, anteriorly by the anterior belly of the digastrics muscle, posteriorly by the posterior belly of digastrics muscle inferomedially by the mylohyoid and hyoglossus muscles and inferiorly by the hyoid bone. The space is enclosed by the SLDCF, except along the posterior margin of the mylohyoid muscle, permitting continuity within the sublingual space and potential communications with the parapharyngeal space (Fig. 3.2.11). The contents of the submandibular space are superficial portion of the submandibular gland, submandibular lymph nodes, fat and anterior belly of digastric muscle. The facial artery, vein as well as a portion of the hypoglossal nerve courses through the space (Fig. 3.2.12). The sublingual space is bounded anteriorly by the mandible, medially by the midline genioglossus/geniohyoid muscle complex, inferolaterally by the mylohyoid muscle and supermedially by the mucosa of the floor of the mouth. Communication of the right and left sublingual space occurs anteriorly under the frenulum of the tongue. Although predominantly fat containing, the sublingual space also contains the sublingual gland and duct, a portion of the hyoglossus muscle, the lingual artery and vein, lingual nerve (branch of CAN 5), branches of glossopharyngeal and hypoglossal nerve as well as the deep portion of the submandibular gland and duct (Fig. 3.2.13).
3.2: Overview of head and neck imaging anatomy
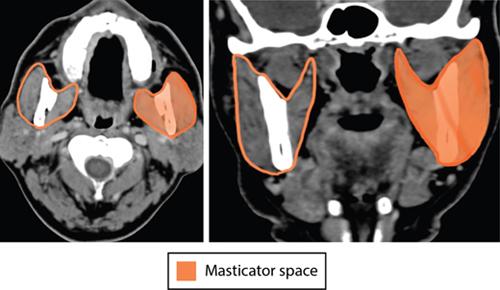
Masticator space
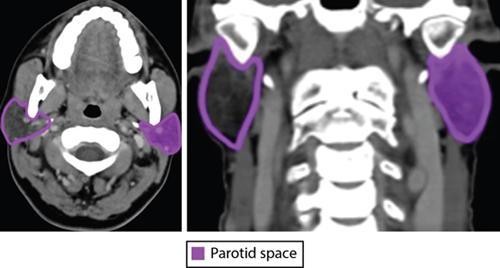
Parotid space
Submandibular space

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








