Chapter 10 Oxytocin and fetal heart rate changes
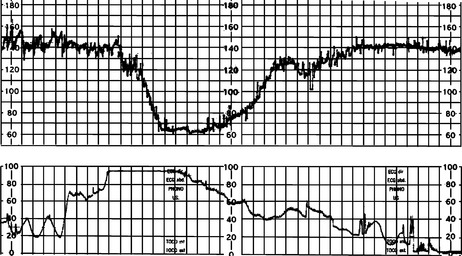
Oxytocin is commonly used for induction and augmentation of labour. Many medico-legal cases relate to the misuse of oxytocin. Oxytocin does not have a direct influence on the fetal heart rate (FHR) or on the controlling cardiac centres in the brain, as is the case with some anaesthetic and antihypertensive drugs. Its influence is indirect via increased uterine activity, mostly due to increased frequency of contractions or baseline pressure (hypertonus). Increase in duration or amplitude of contractions can also lead to FHR changes. The NICE guidelines define hyperstimulation as more than five contractions in 10 min (some literature defines it as polysystole) and if it is associated with FHR changes it is defined as ‘hyperstimulation syndrome’.98 Figure 10.1 shows fetal bradycardia due to ‘tetanic’ or sustained contractions lasting for 3–4 min, caused by oxytocin hyperstimulation. Because the subject was a healthy fetus with a normal reactive FHR prior to the episode, the transient bradycardia returned to normal once the oxytocin infusion was reduced and the abnormal contractions ceased.
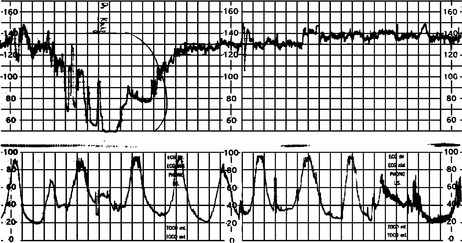
Figure 10.2 shows fetal bradycardia due to ‘hypertonic’ uterine activity. The baseline pressure was elevated by 15 mmHg for 3 min despite regular contractions. The raised baseline pressure reduced the perfusion in the retroplacental area leading to FHR changes, which returned to normal once the baseline pressure settled to normal levels, restoring normal perfusion.
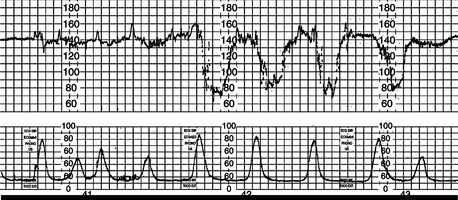
Figure 10.3 shows a reactive trace with one contraction in 3 min. An oxytocin infusion was commenced 10 min from the start of this segment at a rate of 1 mU per min. This resulted in the late decelerations and changes seen in the latter part of the trace. The contraction recording shows no increase in frequency or duration of contractions nor increase in baseline pressure, but shows an increase in amplitude of contractions. Discontinuation of the infusion resulted in return of the FHR trace to normal.
The FHR changes associated with oxytocin infusion may be caused by compression of the cord with contractions or by the reduction in placental perfusion due to increased intrauterine basal pressure and frequent contractions cutting off the blood supply to the placenta. Pressure on the head or supraorbital region of the fetus can also give rise to variable decelerations. The rate of increasing hypoxia would be shown by a deteriorating trend of the FHR. The rate of decline of pH depends on the FHR pattern observed and the physiological reserve of the fetus.99 A rapid decline would be anticipated in post-term and growth-restricted fetuses and those with reduced amniotic fluid with thick meconium, infection or intrapartum bleeding. Fortunately, in the vast majority of patients who are given oxytocin, FHR changes of a worrying nature are not encountered and most changes, even when they occur, are transient and resolve spontaneously, or with reduction of the dose or transient cessation of the infusion. It is good practice to run a strip of cardiotocograph prior to commencing oxytocin to make sure of good fetal health as reflected by a normal reactive FHR pattern: if the trace is pathological then oxytocin should not be used, as it can cause further hypoxia to the fetus by reducing the perfusion to the placenta by additional contractions.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree