Karen Rosendahl, Jean-François Chateil, Karl Johnson
Paediatric Musculoskeletal Trauma and The Radiology of Non-Accidental Injury and Paediatric Factures
Fractures account for up to 25% of all injuries in children, being commoner in boys.1 The type and distribution of injuries varies between different age groups in children and adults because of the physiology of the developing skeleton. A child’s bones are more elastic than those of an adult. When a force is applied to a bone, it will generate stresses within that bone, which may be compressive, tensile or shearing. These stresses will result in deformity of the bone, which will progress as the stress increases. When the force is removed, the bone may eventually return to normal. However, at some point, namely the yield stress, the bone enters a phase of plastic deformity, resulting in microscopic fractures on the tensile side of the bone.2 This bone may initially be radiographically normal, but follow-up radiographs may show evidence of a healing periosteal reaction in response to these microfractures. With further increases in the deforming force, the bone’s ultimate stress point will be reached and the bone then fractures.
In adults, the yield point and ultimate stress points are very close together, so plastic deformity is rare. In the younger child, the greater degree of elasticity of the bone means that there can be a significant difference between the yield point and ultimate point, with a greater propensity for plastic deformity. Cortical bone will tolerate compressive stresses better than tensile or shearing forces. Consequently, childhood fractures may be complete or partial (incomplete). A complete fracture occurs when there is complete discontinuity between two or more bone fragments. An incomplete fracture involves trauma and damage to the bone, but a portion of the cortex remains intact due to the increased elasticity of the bone.
Greenstick, buckle and plastic bowing fall into the category of incomplete fractures (Fig. 80-1). Stress injuries can occur due to repeated forces acting upon the bone, which are less than the force needed to fracture the bone (Fig. 80-2). Fractures may also be classified with regards to the fracture line; a simple fracture is where there is only a single fracture line. These fractures can be further described as transverse, oblique or spiral, depending on the appearances of the fracture line with respect to the bone’s long axis. A comminuted fracture is where there are several fracture lines and these include segmental fractures and those with butterfly fragments (Fig. 80-3). Open or compound fractures occur when a wound extends from the skin surface to the fracture. Displacement refers to when there is a space and altered alignment between the fracture fragments.
For the majority of injuries, a good-quality anteroposterior and lateral radiograph is the only imaging which will be required. From these projections, the fracture pattern, along with any shortening or angulation, can be determined. Rotation is best assessed from the relative position of the joints above and below the fracture, which should be included on the radiograph as standard practice. Careful inspection of a fracture may allow the mechanism of injury to be determined, which may have implications as to the stability and hence help determine management.
Physeal Injuries
A cartilaginous physis (growth plate) occurs between a bone and its epiphysis or apophysis. An epiphysis contributes to longitudinal growth while an apophysis does not. In early childhood, not all the epiphysis or apophysis will be ossified and so will not be visible on a radiograph. The transitional zone between the physeal cartilage and the metaphyseal portion of the bone, ‘the zone of provisional calcification’, is the weakest point in the growing skeleton. The physeal cartilage is weaker than bone, which, in turn, is weaker than the surrounding ligaments.
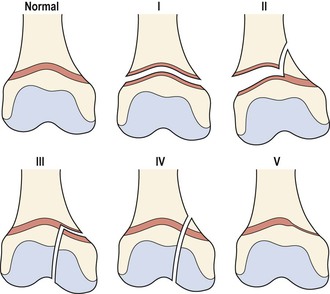
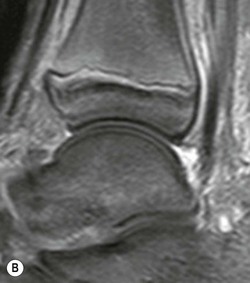
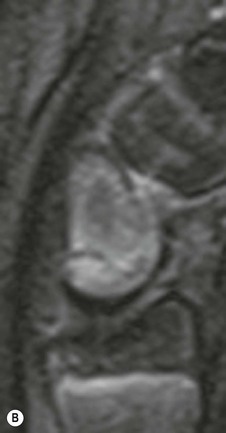
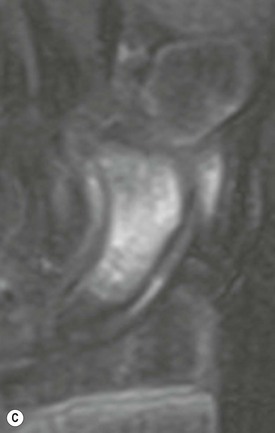
Injuries which may result in a ligamental tear or joint dislocation in an adult are more likely to cause a physeal injury in a child.3 Up to 15% of fractures of the tubular bones in children affect the growth plate and the majority of physeal fractures are due to shearing or avulsion stresses. The classification of physeal injuries typically uses the system of Salter and Harris, which separates fractures into five main types (Figs. 80-4 and 80-5).4 Other fracture types and other categories of injury have been proposed since the original classification.5,6 The importance of the classification system is that for higher grades of injuries, there is an increased likelihood that the growth plate will be damaged, which will result in long-term complications such as malunion, premature fusion (resulting in growth impairment) and avascular necrosis (Fig. 80-6). The latter is most likely to occur in fractures of the femoral or radial neck. Whilst the majority of injuries are clearly shown on standard radiographs, magnetic resonance imaging (MRI) can be used to better visualise the physeal cartilage and the non-ossified portion of the epiphysis (Fig. 80-7).7
The other site of potential physeal damage is at the musculotendinous insertion into an apophysis, particularly following an avulsion injury. In children, the apophyseal physis is the weakest point of the bone, tendon and muscle interface and, consequently, severe traction on the muscle will result in avulsion of a bone or cartilaginous fragment. Avulsion injuries are common sports injuries and most usually seen around the pelvis and elbow (Figs. 80-8 and 80-9).
Low-energy repetitive traction forces can result in microtrauma, causing a chronic apophysitis. Around the medial epicondyle of the humerus, this is eponymously called ‘little leaguer’s elbow’. Radiographs are usually sufficient to diagnose acute avulsion injuries, providing the avulsed fragment is ossified. MR imaging or ultrasound can be helpful in demonstrating soft-tissue swelling, effusion and marrow oedema in the more chronic presentations.
The Upper Limb
Shoulder/Humerus
Fractures of the clavicle can occur from either a direct blow or a fall onto the shoulder or outstretched arm. Typically, they occur in the middle third and there is a high propensity for greenstick injuries due to the plastic nature of the periosteum.8 The clavicle is the commonest site of birth-related fracture and is associated with shoulder dystocia and obstetric brachial plexus palsy. This may cause the neonate to present with reduced arm movement, the differential diagnosis of which includes septic arthritis, osteomyelitis, shoulder dislocation and non-accidental injury (NAI).9
Shoulder dislocation is uncommon under 10 years of age, the presence of the humeral physis appearing to be in some way protective. Displacement is typically anteriorly and the humeral head lies under the coracoid process on the AP radiograph. On the axial view, the humeral head is displaced anteriorly and no longer covers the glenoid.
Proximal humeral fractures are uncommon, with those involving the physis representing just 3% of such injuries. However, the consequences of fractures here may be significant as the physis accounts for 80% of longitudinal growth of the humerus. Care must be taken in reviewing the proximal humerus, as the normal growth plate has an irregular contour which should not be mistaken for a fracture.10
Under 10 years of age, the fractures are typically metaphyseal, whilst in adolescents, they are usually a Salter–Harris type II fracture. Conversely, the proximal humerus is a relatively common site for pathological fractures, typically through a simple bone cyst, creating the ‘fallen fragment sign’, due to a piece of cortical bone lying within the fluid-filled cavity (Fig. 80-10).11
Elbow
There are six separate ossification centres around the elbow joint which appear and fuse in a relatively predictable temporal sequence. These are shown in Table 80-1. Recognition of this sequence is important in determining the presence and type of any injury. While some variation in the appearances can be seen, the internal apophysis should always appear before that of the trochlea, and any deviation from this, with a history of trauma, is suspicious for an avulsed or malpositioned internal apophysis (Fig. 80-11).12
TABLE 80-1
The Ossification Centres around the Elbow Joint
| Age Range at Which The Ossification Centre Becomes Visible Radiographically (Years) | Age Range at Which They Fuse (Years) | |
| Capitellum | 0–2 | 13–16 |
| Radial head | 3–6 | 13–17 |
| Internal (medial) epicondyle | 3–9 | Up to 20 |
| Trochlea | 7–13 | 13–16 |
| Olecranon | 8–10 | 13–16 |
| Lateral (external) epicondyle | 8–12 | 13–16 |
The age at which they appear and then subsequently fuse. In general it occurs earlier in girls than in boys.
A good-quality AP and lateral radiograph is essential for evaluating the elbow joint following trauma, for the important assessment of crucial anatomical landmarks (Figs. 80-12 and 80-13). Fracture, haematoma or effusion into the elbow joint will cause capsular distension and elevation of the fat pads overlying it. A visible posterior fat pad should be regarded as abnormal due to a potential occult injury, particularly a fracture/dislocation of the radial head or undisplaced supracondylar fracture.

A visible anterior fat pad may be a normal finding. The absence of any visible fat pad does not exclude the presence of a fracture. The medial and lateral epicondyles are extracapsular and so are not associated with capsular distension.
Supracondylar fractures are the commonest fractures under the age of 7 years. The majority are the extension type, with posterior displacement of the distal fracture fragment, typically due to a fall on an outstretched arm. Flexion-type fractures with anterior displacement are due to a direct blow on a flexed elbow and are often unstable (Fig. 80-14).13
Complications include nerve entrapment, malunion (leading to either cubitus valgus or varus) and vascular compromise. The absence of the radial pulse may be an indication for arteriography prior to surgical exploration.
Lateral condylar fractures are due to a varus force on an extended elbow. It is important to realise that this fracture may extend through the unossified portion of the capitellum into the joint space (Salter–Harris type IV).14
Forearm/Wrist/Hand
Radial and ulnar fractures can occur together or in isolation, the radius being the commoner single injury site. Forearm fractures may also occur with dislocation at either the elbow or wrist joint, the so-called Monteggia and Galeazzi fractures. To avoid missing a dislocation, it is vital the joints above and below a forearm fracture are visualised properly (Fig. 80-15).

Incomplete fractures of the distal forearm metadiaphysis are common, the mechanism of injury typically being a fall on an outstretched hand. The peak incidence in boys is between 12 and 14 and in girls 10 and 12 years.15 This corresponds to the adolescent growth spurt and relative weakness of the metadiaphysis (Fig. 80-1).
Carpal injuries in childhood are infrequent, the commonest being the scaphoid, which more typically occurs in adolescence. The site of injury is more likely to be the distal third of the scaphoid, compared with the waist in adults, and so the risk of vascular compromise is lower in children. Scaphoid fractures may be radiographically occult, and MR imaging is useful in confirming the diagnosis and expediting appropriate management (Fig. 80-16).16
Metacarpal fractures have an increased incidence in older schoolchildren where the mechanism is usually punching or contact sports. The metacarpal of the little finger is most often injured, with the commonest type of fracture being a Salter–Harris type II.17
The phalanges may fracture from direct trauma or as a result of avulsion forces. Crush injuries of the phalanges are typically seen in the preschool child. It is important that all the ossified phalangeal epiphyses are reviewed, as any avulsed fragments may travel a significant distance proximally.
The Lower Limb
Pelvis
A number of classifications of pelvic fractures have been proposed, with the general aim being to predict the degree of morbidity associated with the injury and to try to assess the mechanism and force vectors involved in the causation. An improved understanding of causation helps plan treatment. In principle, the classification systems all detail the type of fracture and the anatomical sites within the pelvis. Unsurprisingly, the more severe injuries which result in significant disruption of the pelvis are associated with greater long-term morbidity. They are generally associated with high-velocity impacts and often occur with injuries in other anatomical areas, particularly the brain.18–21
The least severe fractures are avulsion injuries, which are common in adolescence and are typically the result of athletic activity. These can occur at a number of sites related to muscle attachments.
Standard AP radiographs are usually the initial investigation and are useful in assessing for avulsion injuries. For higher-grade injuries, CT is a more sensitive investigation and in most circumstances is part of a more general screening of a child following high energy/impact trauma.
Acetabular, Hip and Femur
Acetabular fractures are an uncommon, but significant, injury in childhood, because if the triradiate cartilage is involved, growth and acetabular development may be affected.
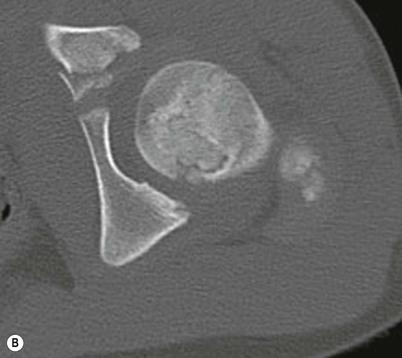
Posterior dislocation of the hip is commoner than anterior, and while dislocation in children is less likely to result in acetabular injury, avascular necrosis of the femoral capital epiphysis is a serious potential complication if the femur remains unreduced for over 24 hours. With dislocations, proper assessment of the acetabular margins is vital to exclude occult fractures and this will be improved with CT or MR imaging (Fig. 80-17).22,23
Femoral head and neck fractures are relatively uncommon and may be associated with femoral head dislocation. They are classified with reference to their location along the femoral neck: namely, transepiphyseal, transcervical, cervicotrochanteric and intratrochanteric. Complications include osteonecrosis (the occurrence of which is increased the more significant the fracture displacement), premature physeal fusion, varus deformity and non-union.24
Femoral diaphyseal fractures may be associated with significant displacement if the fracture line means that there is unopposed muscle traction of the bone fragment. It is vital to check for rotation, as this will not be corrected without manipulation.
Knee
Acute knee trauma is a common childhood symptom. Studies which have been validated in paediatrics have devised rules to determine the need for radiographs within this cohort of patients. Radiographs are only indicated when there is isolated tenderness of the patella and head of the fibula, an inability to flex the knee to 90° or if the patient cannot weight bear. AP and lateral radiographs are standard and the use of the skyline view is arbitrary.25
An effusion within the knee joint will outline the suprapatellar region and obliterate fat planes. A horizontal beam lateral film will show a lipohaemarthrosis due to the different densities of fat and blood within the joint. The presence of a lipohaemarthrosis is suspicious of an intra-articular injury.
Outside of acute trauma, MR imaging is the modality of choice when assessing for pathological conditions of the knee, as it will obviously provide an assessment of ligaments, menisci and cartilage. CT is valuable for detecting intra-articular fracture displacement and detached bony fragments.
In contrast to adults, anterior tibial spine fractures are more likely to occur in childhood compared with anterior cruciate ligament (ACL) ruptures. This occurs when there is forced hyperextension and rotation of the knee. In children, the tensile strength of the ACL is greater than that of the bone, causing avulsion of the tibial spine. The detached bony fragment may be seen on radiographs within the knee joint. Both CT and MRI are more sensitive in assessing the degree of displacement and rotation (Fig. 80-18).
Osteochondral fractures are associated with traumatic lateral dislocation of the patella or axial compressive loading on the femur. Typical sites for injury are the lateral femoral condyle or patella. The fracture is through the subchondral bone and there may be a small bony (loose) fragment within the knee joint.
Osteochondritis dissecans is a defect within the subchondral region of the distal femur, typically occurring on the posterolateral aspect of the medial femoral condyle. Other anatomical sites are the talar dome and capitellum. The full aetiology is unknown, but there is necrosis of the subchondral bone which may be the result of repetitive overloading. On radiographs, there is an oval lucency adjacent to the articular margin.26
The patella is infrequently fractured in children, the commonest types being the comminuted and transverse. Sleeve fractures are avulsion injuries of the inferior pole of the patella with a small amount of detached ossified periosteum, but a large amount of unossified cartilage and retinaculum. This may be difficult to detect on standard radiographs as there is only a small of flake of detached bone, but it is well shown on MR imaging.
Tibia/Ankle/Foot
Tibia
The classical toddler’s fracture is an undisplaced fracture of the middle/distal tibial diaphysis, which may not be initially visible on the convential AP and lateral radiograph (being more discernible on oblique views). The toddler’s fracture is a cause for a child to be non-weight bearing. If there are no other clinical concerns, follow-up imaging is not routinely indicated, due to radiation dose considerations. However, if repeat imaging is performed, periosteal reaction and sclerosis along the fracture line may become visible after about a week (Fig. 80-3).
Stress fractures of the tibia are generally located in the upper third in children aged around 10–15 years and are associated with excessive or continuous physical exercise (Fig. 80-2). Approximately 70% of tibial shaft fractures are isolated, with the remainder also involving the fibula. The tibia shows a reduced tendency to remodel and there may be a risk of varus angulation due to the pull of the long flexors and an intact fibula. Isolated fibular fractures are rare and usually occur from a direct blow.27
Ankle
Most ankle fractures are adequately assessed with standard radiographs (i.e. AP, lateral ± mortice view). Some confusion can occur from the numerous accessory ossification centres which may be visible, particularly adjacent to the malleoli.
Epiphyseal, avulsion and Salter–Harris type I and II fractures of the distal tibia account for the majority of injuries. Injuries are usually caused by indirect trauma with the foot being fixed and forced either into dorsiflexion, plantar flexion, eversion, inversion or rotation (external or internal). The physes of the distal tibia and fibula fuse at the same time, initially centrally followed by medially and then laterally. If only one physis is visible, the suspicion of an epiphyseal injury is raised.
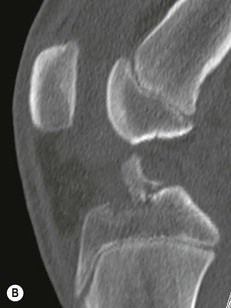
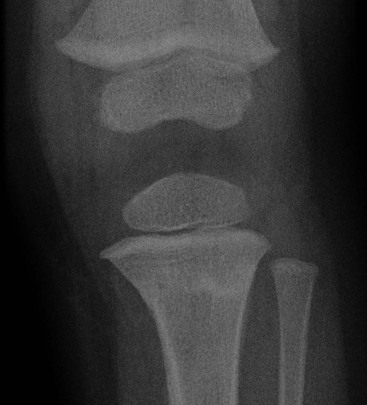
Transitional fractures (triplane and juvenile tillaux) occur in adolescence, as the name implies, as the skeleton becomes more mature (Figs. 80-19 and 80-20). Triplane injuries are fractures caused by external rotation which causes the fracture to extend in the axial, sagittal and coronal planes. If the fibula is also fractured, it suggests a more severe rotational force. The lateral radiograph may suggest a Salter–Harris type II fracture while the AP view demonstrates a type II injury.28
Tillaux fractures are Salter–Harris type III fractures of the epiphysis and the unfused anterolateral portion of the distal tibial physis, due to avulsion of the anterior tibiofibular ligament. The lack of a fracture component in the coronal plane distinguishes it from a triplane fracture.29,30
In all Salter–Harris type III and IV fractures, there will be intra-articular extension of the fracture line and any degree of displacement should be properly evaluated with CT. Displacement greater than 2 mm often requires precise surgical reduction and fixation.
Foot
Foot fractures account for less than 10% of paediatric fractures,31 the majority of which occur in the metatarsals and phalanges, particularly the fifth metatarsal. However, children under 5 years have a higher proportion of first metatarsal fractures, of which greenstick and torus are the commonest types. It is important not to confuse the apophysis of the fifth metatarsal with a fracture (Fig. 80-21).
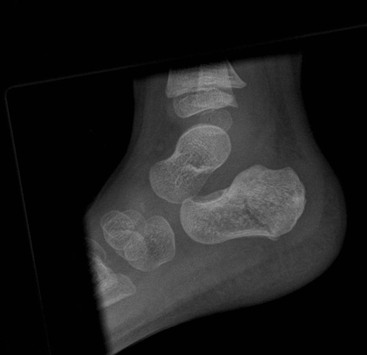
The calcaneum is the commonest tarsal bone to be fractured, classically as a result of a fall from a height (Fig. 80-22). An extra-articular fracture which involves the tuberosity and avoids the posterior facet is commoner in the immature skeleton. There is an association with other injuries to the limb. Bohler’s angle is unreliable under the age of 10 years and a normal Bohler’s angle does not exclude a fracture.32 CT is the imaging modality of choice for all suspected tarsal injuries.
Talar fractures are uncommon, as it is believed that the high cartilage to bone ratio in the young child is protective. Displaced fractures of the talar neck carry the risk of avascular necrosis. Isolated fractures of the cuboid, navicular and cuneiforms are rare and tend to be simple avulsions.
Stress fractures in the athletic child may occur in any tarsal bone.
Cervical Spinal Injuries
Paediatric spinal trauma is uncommon, with childhood injuries accounting for less than 10% of reported spinal injuries. Spinal fractures account for no more than 2% of all paediatric fractures,33 the majority of which are the result of road traffic accidents.
Due to the disproportionate size of a young child’s head and underdeveloped neck musculature, injuries under the age of 12 typically affect the first and second cervical bodies. Younger children are more likely to suffer distraction and subluxation injuries compared with the adult pattern of fractures which occur in the older child.
In children, the spinal column has significantly more flexibility than the spinal cord. Consequently, severe flexion extension injuries may not result in a fracture or ligamental disruption, but will cause significant spinal cord injury. The term ‘spinal cord injury without radiographic abnormality’ (SCIWORA) was described.34 The increased use of MR imaging has been able to demonstrate abnormal cord findings in these patients. However, there is a small group of patients where even the MR imaging is normal despite clinical evidence of cord injury and damage.
It is important that normal anatomical variations are not misinterpreted as possible injuries. The commonest variant is pseudosubluxation at the C2/3 and C3/4 levels. Pseudosubluxation of up to 4 mm is acceptable. A line connecting the anterior aspects of the spinous processes (spinolaminar junction) of C1–C3 should pass within 2 mm of the spinolaminar junction of C2 (Fig. 80-23).
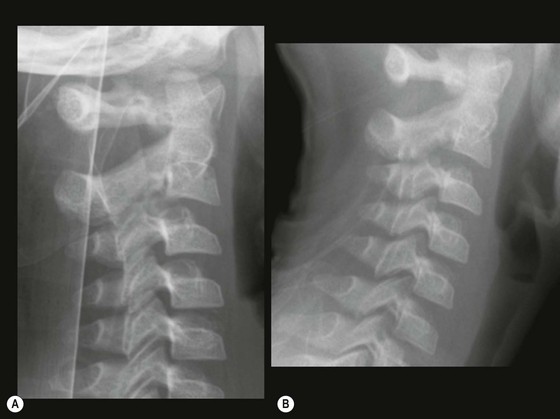
When the C2 spinolaminar junction lies 2 mm or more behind this line then the possibility of a fracture or true subluxation is raised. On an open mouth view, a pseudo-Jefferson fracture may be observed due to ossification of the lateral mass of C1 exceeding that of C2, so that they appear to overhang the axis by up to 6 mm. Pseudo anterior wedging of the vertebral bodies of up to 3 mm can be a normal variation and is particularly common at the C3 level.
Unfused apophyses and ossification centres may cause some confusion with fractures.
Atlantoaxial rotatory fixation (AARF) may or may not follow trauma in children and is a commoner occurrence than in adults.
Four types have been described and CT is the imaging modality of choice. An axial CT is performed in a neutral position, followed by repeat imaging in voluntary, maximal, ipsilateral and contralateral head rotation. In patients with fixation, no rotation of the atlas on the axis is observed while with transient torticollis, a reverse or reduction of rotation occurs.
Thoracic and lumbar injuries are typically the result of hyperflexion, which will result in stable anterior wedge compression fractures, and are commoner in children more than 8 years of age.
Flexion distraction forces causing bone and ligament disruption to the lumbar spine can occur with lap seat-belt restraint. Multilevel injuries are common and warrant imaging evaluation of the entire spinal column. The prognosis for neurological recovery is related to the initial severity of the injury. Some children with significant spinal cord injuries can recover substantial neurological function. Associated injuries within the thorax and abdomen are not uncommon.
Non-accidental injury
The incidence of physical abuse, a subset of child abuse, varies according to age, ethnicity and the specific definition used, and is both under-reported and under-recorded. Common to all definitions is the presence of an injury that the child sustains at the hands of his (or her) caregiver(s) (<http://www.yesican.org/definitions/CAPTA.html>, <http://www.yesican.org/definitions/WHO.html>, <http://www.yesican.org/articles.html>). These injuries are also referred to as inflicted or non-accidental injuries, battered child syndrome35 or shaken baby syndrome.36 When first described in 1946, the shaken baby syndrome included subdural and retinal haemorrhages in conjunction with fractures; however, during the past decade this term has been more and more linked to the abusive head injuries sustained by shaking.
During the past decades, efforts have been made to systematically register the occurrence and nature of child abuse. In the USA, the National Child Abuse and Neglect Data System (NCANDS) has reported annually since 1990 (<http://www.acf.hhs.gov>). For 2010, the unique victim rate was 9.2 per 1000 children in the total population, increasing to around 20 per 1000 for those below 1 year of age. Victimisation was split between the sexes, with boys accounting for 48.5%. As in prior years, the greatest percentage of children was neglected while 17.6% suffered physical abuse. The overall rate of child fatalities was 2.1 deaths per 100,000 children, with nearly 80% being younger than 4 years old. Boys had a higher child fatality rate than girls; 2.5 versus 1.7 per 100,000. Around one-third of child fatalities were attributed exclusively to neglect, while around 40% were caused by multiple maltreatment types, i.e. neglect, physical abuse, psychological maltreatment and/or sexual abuse. More than 80% of duplicate perpetrators of child maltreatment were parents, and another 6% were other relatives of the victim. Of the perpetrators who were parents, more than 80% were the biological parent of the victim. In the USA, child abuse is responsible for approximately 1400 deaths per year37 (<http://www.childwelfare.gov/pubs/factsheets/fatality.cfm>).
The UK does not publish statistics on the number of substantiated child abuse cases recorded every year; however, as at March 2010, there were 46,700 children on child protection registers or the subject of child protection plans, i.e. at risk of abuse (National Society for the Prevention of Cruelty to Children, NSPCC, <http://www.nspcc.org.uk/Inform/research/statistics/statistics_wda48748.html>). A UK-wide study of child maltreatment carried out by the NSPCC in 2009 suggested that one in 14 children (6.9%) aged 11–17 have experienced severe physical violence at the hands of an adult.38
Further, in England, the Department for Education and the Office for National Statistics have collected and reported statistics on children being looked after every year since 1989 (<http://www.education.gov.uk/rsgateway/DB/SFR>). At 31 March 2011, there were 65,520 looked after children in England, an increase of 9% since 2007. Overall, the main reason why social services first engaged with these looked after children was because of abuse or neglect (54%).
In Australia, the 13th annual comprehensive child protection report (Child Protection Australia 2008–09) showed that the number of children subject to a notification of child abuse or neglect increased by 47% from 4.8 to 7.0 per 1000 children over the past 5 years.39
Taken together, the rate of physical child abuse is fairly high in industrialised countries. Infants and young children are at greatest risk, with up to 80% of cases being younger than 5 years and up to half being infants (< 1 year of age).
Clinical Presentation and the Role of the Radiologist
The clinical presentation takes many forms, but the physically abused child typically presents with an obvious injury such as soft-tissue swelling, haematomas, bruises, burns and/or fractures. Fractures are seen in a high proportion of physically abused children and more often in infants.40,41 It is not uncommon, however, for the abused child to present with symptoms of occult injury, particularly in cases of head and abdominal trauma.
Infants with head injuries may present with non-specific symptoms, such as lethargy, irritability, persistent, unexplained vomiting, apnoea, coma or seizures. Abusive head injury is the most common cause of NAI-related death.42 Similar to head injury, severe abdominal trauma may present without visible external signs or history to suggest such an injury.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree