Presentation and Presenting Images
( ▶ Fig. 84.1, ▶ Fig. 84.2, ▶ Fig. 84.3, ▶ Fig. 84.4, ▶ Fig. 84.5, ▶ Fig. 84.6, ▶ Fig. 84.7, ▶ Fig. 84.8, ▶ Fig. 84.9)
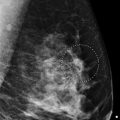
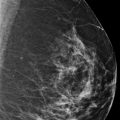
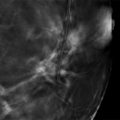
A 39-year-old female presents for a second opinion of the palpable mass in her right breast. Prior to these evaluations, she has had no other mammograms. The palpable area was not marked.
84.1.1 Breast Tissue Density
The breasts are heterogeneously dense, which may obscure small masses.
84.1.2 Imaging Findings
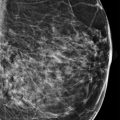
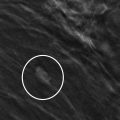
The diagnostic imaging confirms the irregular mass with spiculated margins and grouped amorphous calcifications in the right breast at the 11 o’clock location, 3 cm from the nipple ( ▶ Fig. 84.1, ▶ Fig. 84.2, ▶ Fig. 84.3, ▶ Fig. 84.4, and ▶ Fig. 84.5). The calcifications appear to be confined to the mass and not located beyond the mass ( ▶ Fig. 84.8 and ▶ Fig. 84.9). This mass corresponds to the recently reported palpable finding (area of concern was not marked with a skin marker). The digital breast tomosynthesis (DBT) images better define the margins and determine that the mass is a portion of the dense tissue located in the upper outer quadrant ( ▶ Fig. 84.6 and ▶ Fig. 84.7). Although it is ill-defined mammographically, the mass measures approximately 3 × 3 cm. An ultrasound is recommended.
84.2 Key Images
84.2.1 Imaging Findings
The ultrasound localizes the 2.4 × 2 × 2.4 cm irregular hypoechoic mass with angular and indistinct margins at the 11 o’clock location, 3 cm from the nipple ( ▶ Fig. 84.10 and ▶ Fig. 84.11). Within the mass, there are several echogenic microcalcifications.
84.3 BI-RADS Classification and Action
Category 5: Highly suggestive of malignancy
84.4 Differential Diagnosis
Breast cancer: The irregular shape with angular and indistinct margins and associated amorphous calcifications suggest that this mass is suspicious. On biopsy this mass was a grade 3 invasive ductal carcinoma (IDC).
Fibroadenoma: typically fibroadenomas are more circumscribed. A biopsy yielding a fibroadenoma result would be discordant.
Pseudoangiomatous stromal hyperplasia (PASH): PASH can have variable appearances including no mammographic findings, focal asymmetry, and circumscribed and partially circumscribed masses. PASH can often be palpable but rarely is it associated with calcifications and a mass with irregular margins such as this case demonstrates.
84.5 Essential Facts
Although this lesion was not misinterpreted, it has factors that could easily lead to the reader missing the cancer.
Steps that radiologists can take to increase their accuracy in mammographic interpretation are interpreting both screening and diagnostic mammograms, reviewing pertinent clinical data, adhering to proper positioning and technical requirements, and using ultrasound for palpable findings.
When available, it is important to evaluate a mammogram with comparisons. Subtle changes, including developing asymmetries, can easily be missed.
It is important to be alert for subtle signs of malignancy: areas of architectural distortion, small groups of amorphous calcifications, focal asymmetries, and relatively well-circumscribed masses.
Only 39% of nonpalpable cancers demonstrate the classic signs of spiculated masses and linear calcifications.
It is important to judge a lesion by it most malignant feature.
84.6 Management and Digital Breast Tomosynthesis Principles
A synthesized mammogram is an image that is reconstructed from the images acquired during DBT.
The synthesized mammogram differs from the conventional two-dimensional full-field digital mammogram (2D FFDM). It is meant to be read in conjunction with the DBT images and not as a standalone image.
Early studies suggest that a synthesized 2D mammogram with DBT images is comparable to a conventional 2D FFDM with DBT images.
The benefit of the synthesized 2D mammogram over FFDM is the dose reduction for the combination exam. No additional radiation is required for the synthesized mammogram.
Computer-aided detection (CAD) can be applied to the synthesized mammogram.
There is a learning curve to adjusting to the new look of the synthesized mammogram compared to the conventional FFDM.
84.7 Further Reading
[1] Majid AS, de Paredes ES, Doherty RD, Sharma NR, Salvador X. Missed breast carcinoma: pitfalls and pearls. Radiographics. 2003; 23(4): 881‐895 PubMed
[2] Skaane P, Bandos AI, Eben EB, et al. Two-view digital breast tomosynthesis screening with synthetically reconstructed projection images: comparison with digital breast tomosynthesis with full-field digital mammographic images. Radiology. 2014; 271(3): 655‐663 PubMed
[3] Zuley ML, Guo B, Catullo VJ, et al. Comparison of two-dimensional synthesized mammograms versus original digital mammograms alone and in combination with tomosynthesis images. Radiology. 2014; 271(3): 664‐671 PubMed

Fig. 84.1 Right craniocaudal (RCC) mammogram.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree