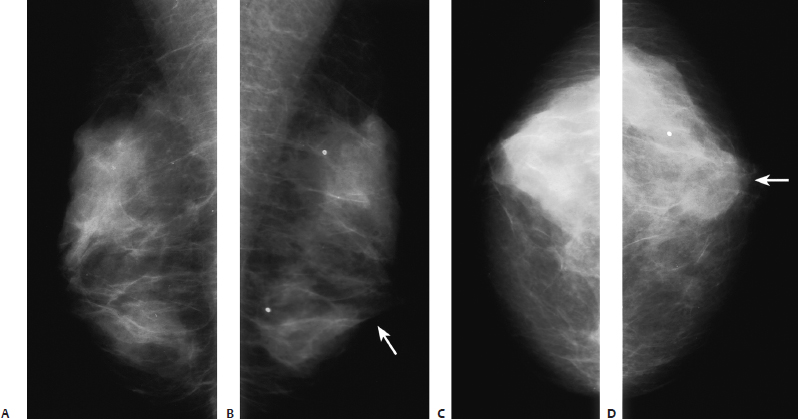
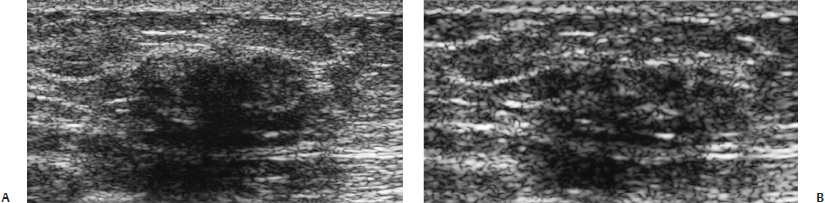
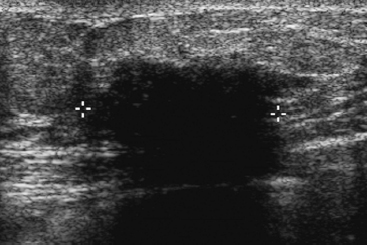
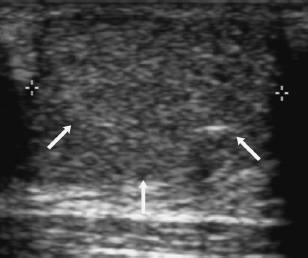
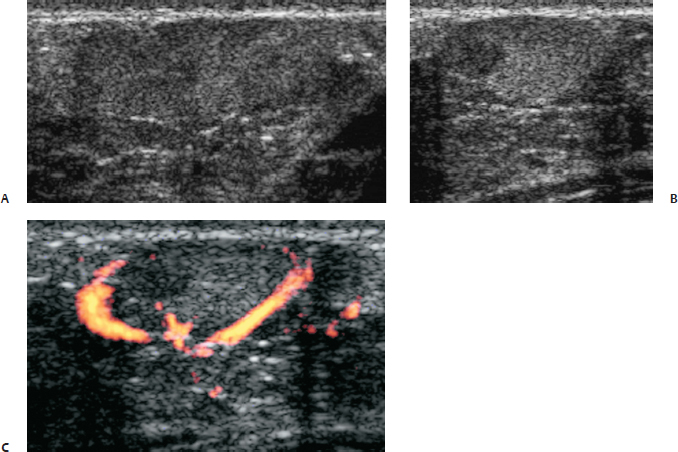
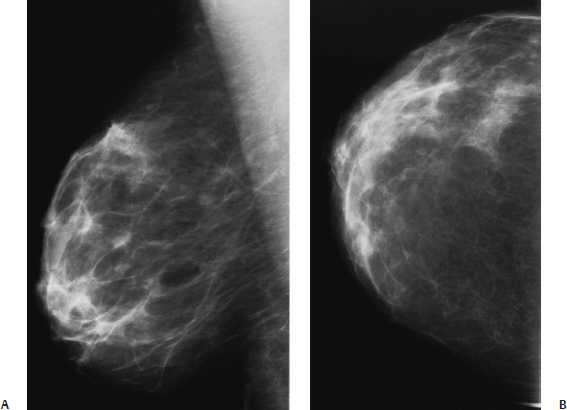
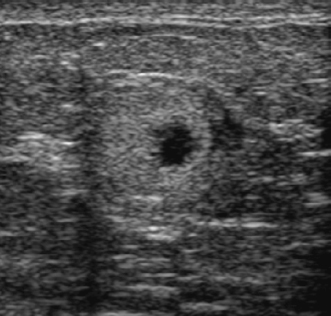
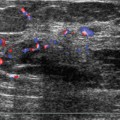
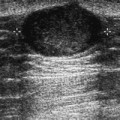
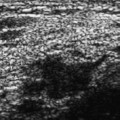
30 Palpable Masses A 74-year-old woman presents with a left breast lump. She was identified with type 1 diabetes 40 years ago and is on an insulin pump. • Left breast: firm 2 cm palpable mass at the 6 o’clock position • Right breast: normal exam Fig. 30.1 The left palpable mass is marked with an arrow. No focal mass is identified. Bilateral mammograms are normal. (A) Right MLO mammogram. (B) Left MLO mammogram. (C) Right CC mammogram. (D) Left CC mammogram. Low Frequency Frequency • 6 MHz Mass (Fig. 30.2) • Margin: ill defined • Echogenicity: hypoechoic • Retrotumoral acoustic appearance: severe shadowing, mass completely obscured • Shape: irregular Fig. 30.2 Because the mass is obscured with the high-frequency examination, lower frequencies were applied. With 8 MHz (A), the mass is mildly hypoechoic. However, normal parenchymal lines are identified running through the mass. With 6 MHz (B), the hypoechogenicity and mass almost disappear. (A) Left antiradial breast sonogram (8 MHz). (B) Left antiradial breast sonogram (6 MHz). High Frequency Frequency • 11.5 MHz Associated Findings (Fig. 30.3) Fig. 30.3 Left antiradial breast sonogram. The palpable mass corresponds to a hypoechoic mass with severe shadowing. • Diabetic mastopathy • BI-RADS assessment category 4, suspicious; biopsy should be considered. • Diabetic mastopathy is identified in less than 1% of benign breast biopsies but represents approximately 13% of benign biopsies in women with type 1 diabetes. Clinically, this abnormality affects young women between the ages of 25 and 40 years who have had a long history of diabetes (usually more than 10 years). This patient is much older than most patients who present with this problem. The mastopathy presents as a painless, hard, irregular mass. About 50% of patients will have multiple masses. • Mammographically, these masses are commonly not identifiable. Sometimes there is an asymmetric focal density or ill-defined mass. • Sonographically, these masses highly attenuate sound. Therefore, when using a high-frequency transducer, the mass will appear as a focal area of heavy shadowing. With lower frequencies, the shadowing and hypoechogenicity will decrease, and no definite mass is evident. Sonographically, these findings do not prevent a biopsy. However, if the biopsy result is diabetic mastopathy, there is good sonographic and pathologic correlation. Boullu S, Andrac L, Piana L, Darmon P, Dutour A, Oliver C. Diabetic mastopathy, complication of type 1 diabetes mellitus: report of two cases and a review of the literature. Diabetes Metab 1998;24:448–454 Hunfeld KP, Bässler R. Lymphocytic mastitis and fibrosis of the breast in long-standing insulin-dependent diabetics: a histopathologic study on diabetic mastopathy and report of ten cases. Gen Diagn Pathol 1997;143:49–58 Logan WW, Hoffman NY. Diabetic fibrous breast disease. Radiology 1989;172:667–670 A 14-year-old girl presents with new left breast lump. • Left breast: 3 cm smooth mass extending from the 10 o’clock to the 2 o’clock positions along the areolar margin • Right breast: normal exam Frequency • 7 MHz • Margin: well defined • Echogenicity: hypoechoic • Retrotumoral acoustic appearance: no shadowing • Shape: ellipsoid Fig. 30.4 Left radial breast sonogram. The palpable mass corresponds to a well-defined, hypoechoic mass with a thin, lucent rim (arrows). • Juvenile fibroadenoma • BI-RADS assessment category 3, probably benign; short-interval follow-up • Fibroadenoma is the most common mass in adolescent girls. Most of these fibroadenomas are the adult type of histology. However, some adolescents have juvenile fibroadenomas, which are variants of the adult type. These patients commonly present with a rapidly growing mass. Microscopically, the tumor demonstrates a pericanalicular growth pattern, as opposed to the usual intracanalicular pattern of adult fibroadenomas. Furthermore, the stroma is more cellular than the adult type. • Because these masses are palpable and occur in young women, they are generally initially identified sonographically. Their appearance is identical to adult fibroadenomas. They are generally well-defined oval or lobulated hypoechoic masses. Because these lesions tend to be large and growing, they are commonly biopsied even though their appearance is sonographically relatively benign (as in this case). Ashikari R, Farrow JH, O’Hara J. Fibroadenomas in the breast of juveniles. Surg Gynecol Obstet 1971;132:259–262 Devitt JE. Juvenile giant fibroadenoma of the breast. Can J Surg 1974;17:205–207 Tavassoli FA, Fattaneh A. Pathology of the Breast. 2nd ed. Stamford: Appleton and Lange; 1999:583–586 A 37-year-old woman who is 9-months postpartum presents with a new right breast lump. She recently had symptoms of right breast mastitis that have improved on antibiotics. She is still nursing her baby. • Right breast: smooth, soft, mobile mass at the 6 o’clock position • Left breast: normal exam Frequency • 10 MHz Mass • Margin: well defined • Echogenicity: heterogeneous • Retrotumoral acoustic appearance: no shadowing • Shape: ellipsoid (Fig. 30.5) Fig. 30.5 The palpable lump corresponds to a well-defined, oval mass with heterogeneous echogenicity. (A) Right radial breast sonogram. (B) Right antiradial breast sono-gram. (C) Right antiradial color power Doppler breast sonogram. • Lactating adenoma • BI-RADS assessment category 4, suspicious; biopsy should be considered. • Adenomas are benign tumors consisting of epithelial and myoepithelial lined tubules. Adenomas differ from fibroadenomas because adenomas have little stroma. In fibroadenomas, stromal cells are the dominant feature. • Lactating adenomas occur in young women who are either pregnant or nursing. Of an Armed Forces Institute of Pathology (AFIP) series of 88 lactating adenomas, the oldest woman was 38 years. • Because lactating adenomas present as palpable masses in young pregnant or nursing women, these masses are commonly imaged only with sonography. They are generally well-defined, oval or lobulated masses that are hypoechoic or heterogeneous in echogenicity. They are sonographically similar to fibroadenomas. Bassett LW, Ysrael M, Gold RH, Ysrael C. Usefulness of mammography and sonography in women less than 35 years of age. Radiology 1991;180:831–835 Hertel BF, Zaloudek Kempson RL. Breast adenomas. Cancer 1976;37:2891–2905 Tavassoli FA, Fattaneh A. Pathology of the Breast. 2nd ed. Stamford: Appleton & Lange; 1999:157–165 A 49-year-old woman presents with a red spot on her right breast. • Right breast: tender mass present at the 1:30 clock position; diffuse erythema of the upper inner quadrant • Left breast: normal exam Fig. 30.6 Right breast mammogram is normal. (A) Right MLO mammogram. (B) Right CC mammogram. Frequency • 7 MHz Mass (Fig. 30.7) • Margin: ill defined • Echogenicity: heterogeneous • Retrotumoral acoustic appearance: no shadowing • Shape: ellipsoid Fig. 30.7 Right radial breast sonogram. The palpable mass corresponds to a complex, thick-walled mass that has fluid and solid components. • Abscess • BI-RADS assessment category 4, suspicious; biopsy should be considered. • About 0.2 cc of yellow purulent material was aspirated, and the patient’s symptoms resolved with antibiotics. • Abscesses are most commonly the result of mastitis from either Staphylococcus aureus
Case 30.1: Young Women—Diabetic Mastopathy
Case History
Physical Examination
Mammogram (Fig. 30.1)
Ultrasound
Pathology
Management
Pearls and Pitfalls
Suggested Reading
Case 30.2: Young Women—Juvenile Fibroadenoma
Case History
Physical Examination
Ultrasound
Pathology
Management
Pearls and Pitfalls
Suggested Reading
Case 30.3: Pregnant or Lactating Women—Lactating Adenoma
Case History
Physical Examination
Ultrasound
Pathology
Management
Pearls and Pitfalls
Suggested Reading
Case 30.4: Scattered Heterogeneous or Extremely Dense Mammogram—Abscess
Case History
Physical Examination
Mammogram (Fig. 30.6)
Ultrasound
Pathology
Management
Pearls and Pitfalls
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Radiology Key
Fastest Radiology Insight Engine