Presentation and Presenting Images
( ▶ Fig. 85.1, ▶ Fig. 85.2, ▶ Fig. 85.3, ▶ Fig. 85.4, ▶ Fig. 85.5, ▶ Fig. 85.6, ▶ Fig. 85.7)
A 63-year-old female with a history of treated right breast cancer presents for evaluation of a palpable thickening in the left breast found 2 months ago. The area of concern is marked with a BB.
85.1.1 Breast Tissue Density
There are scattered areas of fibroglandular density.
85.1.2 Imaging Findings
The area of thickening marked with a BB is in the subareolar region. The conventional digital mammograms and the additional spot-compression mammograms do not reveal any focal finding ( ▶ Fig. 85.1, ▶ Fig. 85.2, ▶ Fig. 85.3, ▶ Fig. 85.6, and ▶ Fig. 85.7). The complexity of the subareolar region can easily obscure lesions. The digital breast tomosynthesis (DBT) images suggest an area of architectural distortion at the12 o’clock location in the subareolar region ( ▶ Fig. 85.4 and ▶ Fig. 85.5). An ultrasound was recommended for further evaluation.
85.2 Diagnostic Images
( ▶ Fig. 85.8, ▶ Fig. 85.9, ▶ Fig. 85.10, ▶ Fig. 85.11, ▶ Fig. 85.12)
85.2.1 Imaging Findings
The targeted ultrasound of the thickening located at 12 o’clock reveals multiple irregular hypoechoic masses with angular margins with the epicenter 5 cm from the nipple ( ▶ Fig. 85.8 and ▶ Fig. 85.9). The masses span an area of 4 cm, larger than noted on DBT. The largest mass in this group measures 12 × 9 × 11 mm. Due to the suspicious nature of these masses and their extent, an axillary ultrasound was performed. In the axilla 13 cm from the nipple, there was an oval hypoechoic mass measuring 3.2 × 1.9 cm ( ▶ Fig. 85.10). Both areas were biopsied with ultrasound guidance. The ribbon clip is located in the area corresponding to where the patient noted thickening ( ▶ Fig. 85.11 and ▶ Fig. 85.12).
85.3 BI-RADS Classification and Action
Category 4C: High suspicion for malignancy
85.4 Differential Diagnosis
Invasive ductal cancer (IDC) with axillary metastases: The mammographic and ultrasound presentation is not typical for cancer. The large area of involvement with the abnormal appearing axillary node raises suspicion and a biopsy is warranted. On biopsy, this lesion was a grade 3 IDC with axillary nodal metastases.
Multiple abscesses with inflamed axillary lymph node: Typically, for this diagnosis, there would be additional signs of skin thickening and edema within the parenchyma, which are not present,.
Papillomatosis: This lesion typically presents as multiple small masses in a segmental distribution. It is not typical that they are accompanied by an enlarged and pathologic-appearing axillary lymph node.
85.5 Essential Facts
This lesion was essentially mammographically occult. DBT suggested a small area of architectural distortion; however, this greatly underestimated the size of the lesion.
In this case, the patient’s clinical symptoms contributed most to detection of the lesion.
Of breast cancers that are mammographically occult, 9 to 16% are detected only by palpation. Distinguishing between benign and malignant lesions on palpation alone is limited. Only 20% of surgical biopsies for palpable lesions detect malignancy.
Patients with clinical symptoms and no overt signs on mammography that correlate to the symptoms warrant further evaluation with ultrasound.
If mammogram and ultrasound are negative for a palpable mass, then the evaluation should be based on clinical symptoms. This may include close observation, patient reassurance, or a palpated-guided biopsy.
85.6 Management and Digital Breast Tomosynthesis Principles
Some lesions will be occult on DBT, just as they can be occult on mammography.
Most studies to date have compared DBT to FFDM. Larger studies are needed to determine the proportion of cancers detected by DBT that are mammographically occult, and what proportion of cancers are occult on DBT.
Some cancers that have been reported occult on DBT can been seen on contrast-enhanced magnetic resonance (MR) imaging. Some of these lesions have been large. The reason why these lesions may not have been detected on DBT is the lack of, or missed, architectural distortion or the lack of distinct mass margins.
85.7 Further Reading
[1] Conant EF. Clinical implementation of digital breast tomosynthesis. Radiol Clin North Am. 2014; 52(3): 499‐518 PubMed
[2] Georgian-Smith D, Taylor KJ, Madjar H, et al. Sonography of palpable breast cancer. J Clin Ultrasound. 2000; 28(5): 211‐216 PubMed
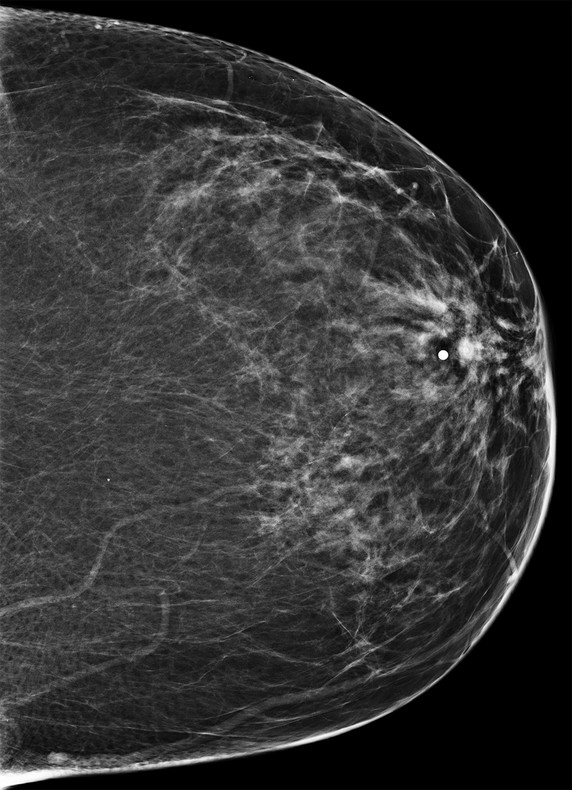
Fig. 85.1 Left craniocaudal (LCC) mammogram.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree