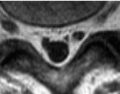
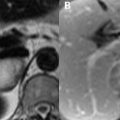
71 Pancreatic Disease Fat saturation is important to improve the differentiation between pancreatic parenchyma and peripancreatic fat, both of which demonstrate high SI on conventional T1WI, the former due to aqueous proteins within acinar cells. Contrast-enhanced T1WI is also performed with FS, the normal pancreas exhibiting enhancement peaking in the arterial phase and fading thereafter. Pancreatic adenocarcinoma is hypointense to parenchyma on such images. Carcinomas with prominent fibrous components, however, will demonstrate progressive enhancement, appearing hyperintense to parenchyma on delayed imaging. The pancreatic head mass (white arrow) in the region of the ampulla illustrated in the axial images of Figs. 71.1A,B demonstrates moderate to low SI on both (A) T2WI and (B) T1WI. This mass obstructs the confluence of the common bile and pancreatic ducts, resulting in dilatation of both structures— the so-called double-duct sign—best seen in the thick-slab MRCP image of Fig. 71.1C. Pancreatic adenocarcinoma and focal, chronic pancreatitis may appear similar. Chronic pancreatitis is less well defined, enhances in the early hepatic venous phase relative to the parenchyma, and is more hyperintense on T2WI due to prominent edema. Pancreatic carcinoma is favored by the presence of lymphadenopathy, distant metastases, or vascular encasement. Optimal sequences for detection of lymphadenopathy vary based on nodal location. Interstitial-phase contrast-enhanced FS T1WI are generally helpful, but porta hepatis nodes are better seen against the background liver on T2WI. Mesenteric and retroperitoneal nodes are well detected against abundant surrounding fat on T1WI. Pancreatic carcinoma metastatic to the liver exhibits an MRI appearance similar to that of colorectal metastases and other adenocarcinomas (See Chapter 66).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree