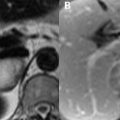
19 Parenchymal Infections Pyogenic abscesses most frequently arise hematogenously, seeding the brain at the gray–white matter junction. They may also occur as sequelae of contiguously spreading sinus infections (see Chapter 20) or trauma. Streptococcus is the most common etiologic organism, followed by staphylococcus and pneumococcus. Abscesses favor the frontal and parietal lobes within the MCA distribution, and their early appearance is one of a diffuse cerebritis, consisting of infiltrating lymphocytes. This infiltrate enhances heterogeneously, and demonstrates high SI on T2WI with low to moderate SI on T1WI. Within the first week, a central necrotic area forms, an area subsequently enveloped by collagen in the second week. This collagen wall appears as a rim of low SI on T2WI and may be surrounded by a disproportionate amount of edema (Fig. 19.1A). The central area is necrotic and typically demonstrates restricted diffusion (Fig. 19.1B) due to its pustulant contents. Central ADC values rise with treatment, and any return in diffusion restriction foretells a recurrence in infection. Similar DWI findings may be seen, although are less common, in necrotic primary or metastatic cancers, which can also demonstrate ring-enhancement thus rendering differentiation from a pyogenic abscess difficult. In pyogenic abscesses, the enhancement (Fig. 19.1C
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree