Part 1 Airway, Cardiac, and Chest Imaging
Case 1

Key Imaging Finding
Narrowing of the airway.
Top Three Differential Diagnoses
Croup (laryngotracheobronchitis). Croup is the most common cause of upper airway obstruction in children between 6 months and 3 years of age, with peak incidence around 1 year. The radiographic hallmark is symmetrical subglottic airway narrowing manifested by loss of normal shouldering of the upper airway on the frontal projection, referred to as the “steeple” sign. The lateral view commonly demonstrates overdistention of the hypopharynx, as well as narrowing of the subglottic airway.
Epiglottitis. This potentially life-threatening disease affects older patients than those with croup. When the diagnosis is suspected, a provider capable of managing the child’s airway should be immediately available during imaging. The radiographic hallmark is epiglottic enlargement (thumb sign) on the lateral view, as well as thick aryepiglottic folds. Epiglottitis may mimic croup on a frontal view.
Retropharyngeal abscess. Space-occupying processes in the prevertebral and retropharyngeal soft tissues may exert mass effect on the airway, causing dyspnea and stridor. The differential diagnosis of widened prevertebral soft tissues includes abscess, hemorrhage, lymphadenopathy, and pseudothickening. If physiological pseudothickening is suspected, a repeat inspiratory exam with the neck fully extended or airway fluoroscopy may resolve the dilemma.
Additional Differential Diagnoses
Bacterial tracheitis. Bacterial tracheitis is characterized by exudative plaques that adhere to the tracheal wall. Because of their flat, longitudinal configuration, they may be seen only on one view. Asymmetrical subglottic airway narrowing may resemble the radiographic appearance of croup. However, patients with bacterial tracheitis are typically older (6–10 years old) and more toxic. Adherent mucus in the airway mimics the plaques of bacterial tracheitis but should clear on repeat examination after coughing.
Aspirated foreign body. Both aspirated and ingested foreign bodies may cause an abnormal airway contour on radiographs, and both may present with dyspnea and stridor. It is easy to determine the location of disk-shaped radiopaque foreign bodies (such as coins) on a frontal neck radiograph. Those in the trachea align in the sagittal plane, since the cartilaginous rings of the trachea are incomplete posteriorly, whereas those in the esophagus align in the coronal plane. Radiographic diagnosis of the more common radiolucent foreign bodies is problematic. Direct visualization is the next step in evaluation.
Hemangioma. Hemangiomas tend to cause variably asymmetrical airway narrowing and are commonly detected before the age of 1 year. When subglottic, the patient’s symptoms may mimic other more common etiologies of stridor. Radiographs show asymmetrical mass effect narrowing the airway.
Diagnosis
Croup.
Pearls
Croup is most common in children under 3 years of age; the “steeple” sign is seen on frontal radiographs.
Lateral X-ray of epiglottitis shows epiglottic thickening (thumb sign) and thickened aryepiglottic folds.
Retropharyngeal abscess demonstrates prevertebral soft-tissue swelling.
Foreign body aspiration must always be considered in a child with stridor.
Suggested Readings
John SD, Swischuk LE. Stridor and upper airway obstruction in infants and children. Radiographics. 1992; 12(4):625–643, discussion 644 Yedururi S, Guillerman RP, Chung T, et al. Multimodality imaging of tracheobronchial disorders in children. Radiographics. 2008; 28(3):e29Case 2

Key Imaging Finding
Contrast material in the trachea.
Top Three Differential Diagnoses
Aspiration. Oropharyngeal coordination is critical and if disrupted may lead to aspiration in apparently normal children as well as in those with a history of prematurity, neurological impairment, and craniofacial malformations. Patients may be asymptomatic or present with poor feeding, apnea, cough, wheezing, reactive airway disease, and lower respiratory tract infections. If aspiration is suspected, patients are often evaluated with video fluoroscopy performed with a speech pathologist. This allows detailed assessment of the phases of swallowing and delineation of barium pooling in the valleculae and piriform sinuses as well as laryngeal and subglottic penetration. Patients with clinically occult aspiration show similar findings on esophagrams performed for other purposes. It is important to note at what point the contrast enters the trachea, since that is essential for determining whether it resulted from laryngeal penetration or from abnormal tracheoesophageal communication.
H-type tracheoesophageal fistula (H-TEF). H-TEF is usually diagnosed on esophagrams performed after the immediate newborn period, whereas TEF with esophageal atresia is diagnosed in utero or in newborns due to the esophageal atresia. H-TEF accounts for only 5% of all TEFs. It has an oblique course, passing upward from the low cervical or upper thoracic esophagus to the trachea. Young infants present with cyanosis, cough, and choking with feeds, whereas older children more likely have recurrent lower respiratory infections. X-rays may show gas in the lower esophagus, scattered parenchymal opacities due to aspiration, and gaseous bowel distension. Diagnosis rests on the esophagram, performed with isotonic water-soluble contrast due to risk of aspiration. However, H-TEF may be difficult to identify and diagnosis delayed, perhaps due to intermittent esophageal occlusion. Repeat esophagrams are often needed. Just before the fistula fills with contrast, a small out-pouching from the anterior esophageal wall may be seen. If contrast is seen in the trachea, it is important to identify the fistulous tract to exclude aspiration. If the tract cannot be identified, a tube esophagram may be performed with gradual pullback of an esophageal catheter.
Laryngeal cleft. This rare congenital anomaly consists of communication between a defect in the posterior wall of the larynx and the anterior hypopharynx or esophagus. Clefts above the level of the vocal cords may present in adults. Lower clefts extending into the cervical or thoracic trachea usually present in infants with severe respiratory symptoms. Over half of patients with laryngeal clefts have other malformations of the gastrointestinal (GI) tract, including esophageal atresia, TEF, and imperforate anus; anomalies elsewhere are also common. Diagnosis is difficult. Clefts may be visualized on esophagrams as a thin tract of contrast extending to the larynx or trachea, or as contrast appearing in the trachea without laryngeal penetration. Final diagnosis relies on direct visualization of a defect in the posterior wall of the airway.
Diagnosis
H-type tracheoesophageal fistula.
Pearls
It is essential to determine whether contrast has entered the trachea due to aspiration or due to an abnormal tracheoesophageal communication.
H–tracheoesophageal fistula is usually diagnosed in infancy and is often located near the cervicothoracic junction.
Laryngeal cleft is commonly accompanied with other malformations of the GI tract.
Suggested Readings
Durvasula VS, O’Neill AC, Richter GT. Oropharyngeal dysphagia in children: mechanism, source, and management. Otolaryngol Clin North Am. 2014; 47(5):691–720 Laffan EE, Daneman A, Ein SH, Kerrigan D, Manson DE. Tracheoesophageal fistula without esophageal atresia: are pull-back tube esophagograms needed for diagnosis? Pediatr Radiol. 2006; 36(11):1141–1147 Ng J, Antao B, Bartram J, Raghavan A, Shawis R. Diagnostic difficulties in the management of H-type tracheoesophageal fistula. Acta Radiol. 2006; 47(8):801–805 Windsor A, Clemmens C, Jacobs IN. Rare upper airway anomalies. Paediatr Respir Rev. 2016; 17:24–28Case 3

Key Imaging Finding
Soft-tissue mass in the airway.
Top Three Differential Diagnoses
Aspirated foreign body. The most common intraluminal airway abnormality in a young child is aspirated foreign body. Most aspirated foreign bodies are found on the right, since the course of the right mainstem bronchus is straighter than that of the left. The child may have nonspecific symptoms or present with choking, cough, and unilateral wheezing. The diagnosis is easier when the foreign body is radiodense, but most foreign bodies are radiolucent food material—usually peanuts. Radiographs are often normal. A partially obstructing foreign body may cause lobar or segmental hyperinflation due to air trapping from the ball-valve effect. This suggests the diagnosis even when the foreign body cannot be seen. Larger foreign bodies may completely obstruct the airway, causing atelectasis. The next step is direct visualization of the airway.
Subglottic hemangioma. These are typically seen in the upper trachea of infants younger than 6 months presenting with stridor. Airway narrowing is often asymmetrical, but sometimes the lesions cause circumferential narrowing that mimics croup or subglottic stenosis. CT shows a mass with intense early enhancement. MRI (magnetic resonance imaging) appearance depends on the state of evolution and resembles hemangiomas elsewhere. Most regress spontaneously, but treatment is needed if there is significant airway compromise.
Carcinoid. Primary endobronchial tumors are rare in children. Most, including carcinoid, are malignant. Carcinoid tumors grow slowly and tend to present with wheezing, recurrent pneumonia, and hemoptysis. Findings on chest radiographs mimic those of an aspirated foreign body, but atelectasis is more common than hyperlucency. CT and/or direct visualization with bronchoscopy help differentiate endobronchial carcinoid from aspirated foreign body. The tumors enhance intensely and may be partly calcified. They are ovoid, and their long axis parallels the bronchovascular bundle.
Additional Differential Diagnosis
Papilloma. Airway papilloma is typically seen in the setting of juvenile papillomatosis, acquired from perinatal transmission of human papilloma virus or as a result of tracheostomy. One or more lobulated masses may be seen, usually in the larynx but sometimes in the lower trachea and bronchi. Endobronchial lesions may cause atelectasis or air trapping. Patients with papillomas are more likely to have multiple areas of air space abnormalities than are those with aspirated foreign body or carcinoid.
Diagnosis
Papillomatosis with endotracheal and parenchymal lesions.
Pearls
Hyperinflation and/or hyperlucency of one lobe or lung suggest an endobronchial lesion.
Most aspirated foreign bodies are not visible on radiographs.
Subglottic hemangiomas are usually eccentric but may be circumferential.
Primary endobronchial tumors are rare in children and most often carcinoid tumors.
Suggested Readings
Amini B, Huang SY, Tsai J, et al. Primary lung and large airway neoplasms in children: current imaging evaluation with multidetector computed tomography. Radiol Clin North Am. 2013; 51:637-657 Pugmire BS, Lim R, Avery LL. Review of ingested and aspirated foreign bodies in children and their clinical significance for radiologists. Radiographics 2015; 35:1528–1538 Roby BB, Drehner D, Sidman JD. Pediatric tracheal and endobronchial tumors: an institutional review. Arch Otolaryngol Head Neck Surg. 2011; 137:925-929 Yedururi S, Guillerman RP, Chung T, et al. Multimodality imaging of tracheobronchial disorders in children. Radiographics 2008; 28:e29Case 4

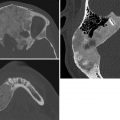
Key Imaging Finding
Vascular anomaly with esophageal and tracheal compression.
Top Three Differential Diagnoses
Aberrant right subclavian artery (RSCA). Aberrant RSCA is a common isolated arch anomaly (1% of the population) that is rarely symptomatic. In this anomaly, the RSCA is the last branch of the left aortic arch. It courses behind the esophagus toward the right upper chest, causing posterior indentation on the esophagus during an esophagram. It is not considered a complete vascular ring.
Double aortic arch. This is the most common symptomatic arch anomaly. Two aortic arches are present in this isolated anomaly. The right arch is higher and larger in 75% of cases. The two arches join posteriorly to form the (usually left-sided) descending aorta. The arches thus encircle and may compress the esophagus and trachea, resulting in stridor or problems with feeding. The esophagram will show posterior and bilateral lateral indentation on the esophagus, as well as narrowing of the trachea. MRI and contrast-enhanced CT are excellent modalities to define this vascular anomaly and its effects on surrounding structures.
Right aortic arch with aberrant left subclavian artery (LSCA). In this anomaly, the LSCA arises from the Kommerell diverticulum off a right aortic arch and passes posterior to the esophagus to the left upper extremity. The ductal ligament extends from the LSCA to the left pulmonary artery, completing this often-symptomatic vascular ring.
Additional Differential Diagnoses
Pulmonary sling. In this anomaly, the left pulmonary artery arises from the right pulmonary artery and passes between the trachea and esophagus on its way to the left lung. Esophagrams show an anterior indentation on the esophagus and a posterior indentation on the trachea. Associated tracheobronchial anomalies, such as complete tracheal rings, are common and may contribute to respiratory symptoms.
Innominate artery compression syndrome. Compression of the trachea by the crossing innominate artery is a rare cause of respiratory compromise in infants. The innominate artery origin or course may be anomalous in these cases. The patients have a normal left aortic arch. It is uncertain whether this constitutes a real entity, or whether symptoms result from underlying abnormal tracheal development. Surgical reimplantation or suspension may help relieve tracheal narrowing.
Diagnosis
Double aortic arch.
Pearls
Aberrant right subclavian artery is a common anomaly that is rarely symptomatic and is not considered a complete ring.
Double aortic arch and right arch with aberrant LSCA are the most common symptomatic vascular rings.
An aberrant left subclavian artery (from a right aortic arch) arises from the diverticulum of Kommerell.
Pulmonary sling (aberrant origin of the left pulmonary artery) is associated with complete tracheal rings.
Suggested Readings
Castañer E, Gallardo X, Rimola J, et al. Congenital and acquired pulmonary artery anomalies in the adult: radiologic overview. Radiographics. 2006; 26(2):349–371 Hernanz-Schulman M. Vascular rings: a practical approach to imaging diagnosis. Pediatr Radiol. 2005; 35(10):961–979 Kellenberger CJ. Aortic arch malformations. Pediatr Radiol. 2010; 40(6):876–884 Oddone M, Granata C, Vercellino N, Bava E, Tomà P. Multi-modality evaluation of the abnormalities of the aortic arches in children: techniques and imaging spectrum with emphasis on MRI. Pediatr Radiol. 2005; 35(10):947–960Case 5

Key Imaging Finding
A cyanotic infant with decreased pulmonary flow.
Top Three Differential Diagnoses
Tetralogy of Fallot. Tetralogy of Fallot is the most common cyanotic heart condition in children. The four components that define this anomaly are: right ventricular outflow tract obstruction (pulmonic stenosis), ventriculoseptal defect (VSD), overriding aorta, and right ventricular hypertrophy, all resulting from malalignment of the conal septum. Deficiency of the main pulmonary artery segment and elevation of the cardiac apex due to right ventricular hypertrophy lead to the classic radiographic appearance of a boot-shaped heart. Pulmonary vascularity is usually decreased, but severity varies. The aortic arch is on the right in 25% of patients.
Pulmonary atresia. The primary anatomical defect is underdevelopment of the right ventricular outflow tract and pulmonary valve. When present with a VSD, this anomaly is considered a severe variant of tetralogy of Fallot, with similar radiographic findings. When the ventricular septum is intact, there is an obligatory right-to-left shunt at the atrial level. Although the radiographic appearance varies, severe cardiomegaly is common. Pulmonary vascularity is normal to decreased and dependent on a patent ductus arteriosus (PDA).
Tricuspid atresia. In tricuspid atresia, there is no direct path for blood flow between the right atrium and right ventricle. However, there is a right-to-left shunt at the atrial level, usually through a patent foramen ovale. Pulmonic blood flow depends on the presence of a VSD and/or PDA. Associated anomalies occur in up to 30% of affected patients (most commonly transposition of the great arteries). In isolated tricuspid atresia with a small VSD, chest radiographs demonstrate a normal or small heart with decreased pulmonary blood flow. However, when a large VSD is present, there is usually cardiomegaly and increased pulmonary blood flow. A right-sided aortic arch is present in about 10% of patients.
Additional Differential Diagnoses
Double outlet right ventricle. Double outlet right ventricle occurs when both the aorta and pulmonary outflow tracts arise from the right ventricle. With 16 described variants, radiographic appearance varies. Some forms mimic tetralogy of Fallot, with pulmonary oligemia and diminished left hilar shadow.
Ebstein anomaly. Ebstein anomaly consists of apical displacement of the tricuspid valve, resulting in atrialization of the right ventricle. Tricuspid regurgitation and stasis of blood flow within the right atrium lead to massive right-sided cardiomegaly with a “box-shaped” heart and pulmonary oligemia. A right-to-left shunt at the atrial level is common.
Diagnosis
Tetralogy of Fallot.
Pearls
Tetralogy of Fallot is the most common cyanotic congenital heart disease.
Tetralogy is characterized by pulmonic stenosis, ventricular septal defect, right ventricular hypertrophy, and overriding aorta.
Pulmonary atresia with a ventricular septal defect is considered a severe variant of tetralogy of Fallot.
Ebstein anomaly leads to massive right-sided cardiomegaly with a “box-shaped” heart.
Suggested Readings
Ferguson EC, Krishnamurthy R, Oldham SA. Classic imaging signs of congenital cardiovascular abnormalities. Radiographics. 2007; 27(5):1323–1334 Kellenberger CJ, Yoo SJ, Büchel ER. Cardiovascular MR imaging in neonates and infants with congenital heart disease. Radiographics. 2007; 27(1):5–18 Lapierre C, Déry J, Guérin R, Viremouneix L, Dubois J, Garel L. Segmental approach to imaging of congenital heart disease. Radiographics. 2010; 30(2):397–411 Schweigmann G, Gassner I, Maurer K. Imaging the neonatal heart: essentials for the radiologist. Eur J Radiol. 2006; 60(2):159–170Case 6

Key Imaging Finding
A cyanotic infant with increased pulmonary vascularity.
Top Three Differential Diagnoses
Transposition of the great arteries (TGA). In d-TGA (dextro-TGA), the aorta arises from the right ventricle and the pulmonary trunk arises from the left ventricle. Without a source for admixture (patent foramen ovale [PFO], ventricular septal defect [VSD], or patent ductus arteriosus [PDA]), this anatomy is incompatible with life. The historical classical radiographic appearance of cardiomegaly, a narrowed mediastinum (“egg on string”), and increased pulmonary vascularity is less common in the current era since patients are now treated in the immediate postnatal period. Instead, in the neonate a normal chest radiograph may be encountered.
Truncus arteriosus. Truncus arteriosus results from failure of division of the primitive single truncal vessel into the aorta and main pulmonary artery. This uncommon lesion accounts for only 1% of cases of congenital heart disease. There is always a large, high VSD. The degree of pulmonary blood flow is initially variable, depending upon pulmonary resistance. When pulmonary resistance drops, usually day 2 to 3 of life, pulmonary blood flow may dramatically increase. The combination of cardiomegaly, a right-sided arch (30% of cases), and increased pulmonary vascularity suggests the diagnosis.
Total anomalous pulmonary venous return (TAPVR). In TAPVR, the pulmonary veins do not connect normally with the left atrium; instead, they drain into the right heart via various venous pathways. There are three types, classified by the location of pulmonary venous drainage: supracardiac, cardiac, and infracardiac. Supracardiac (usually nonobstructed) type 1 is the most common and may result in the “snowman” configuration of the heart due to an enlarged superior vena cava (SVC) and left vertical vein. In the cardiac type, pulmonary veins drain via the coronary sinus. With infracardiac TAPVR, pulmonary veins drain below the diaphragm into the portal veins or inferior vena cava; typically, this obstructed form of TAPVR demonstrates a normal-sized heart and vascular congestion. Infracardiac TAPVR is associated with heterotaxy. In all three types, intracardiac shunting occurs via a PFO. Imaging and clinical features vary with the type of TAPVR.
Additional Differential Diagnoses
Tricuspid atresia. In tricuspid atresia, there is no direct path for blood flow from the right atrium into the right ventricle. There must therefore be a right-to-left shunt at the atrial level, usually through a PFO. Pulmonic blood flow depends on leftto-right shunting through a VSD and/or PDA. When a large VSD is present, there is usually cardiomegaly and increased pulmonary blood flow.
Single ventricle. In this rare malformation, the interventricular septum is absent. The nomenclature describing this diagnosis can be confusing, indicating specific associated anatomy. Patients without pulmonic stenosis demonstrate cardiomegaly, an enlarged main pulmonary artery, and increased pulmonary blood flow.
Diagnosis
Supracardiac total anomalous pulmonary venous return.
Pearls
The superior vena cava and left vertical vein result in the “snowman” configuration in type 1 total anomalous pulmonary venous return.
Severe pulmonary edema with normal heart size is the classic appearance of infradiaphragmatic total anomalous pulmonary venous return.
Transposition of the great arteries shows parallel rather than crossing great vessel origins on prenatal ultrasound (US) and—if chronic—“egg on a string” on radiographs.
Suggested Readings
Ferguson EC, Krishnamurthy R, Oldham SA. Classic imaging signs of congenital cardiovascular abnormalities. Radiographics. 2007; 27(5):1323–1334 Lapierre C, Déry J, Guérin R, Viremouneix L, Dubois J, Garel L. Segmental approach to imaging of congenital heart disease. Radiographics. 2010; 30(2):397–411 Schweigmann G, Gassner I, Maurer K. Imaging the neonatal heart: essentials for the radiologist. Eur J Radiol. 2006; 60(2):159–170Case 7

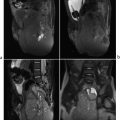
Key Imaging Finding
Shunt vascularity.
Top Three Differential Diagnoses
Ventricular septal defect (VSD). VSD is the most common of the four causes of acyanotic shunt vascularity and is the second most common congenital cardiac malformation after bicuspid aortic valve. Radiographs may be normal when the defect is small. Larger defects are associated with cardiomegaly with left atrial enlargement, increased number and size of visualized, well-defined, “sharp” pulmonary vessels (i.e., shunt vascularity), and an enlarged main pulmonary artery. Hyperinflation is common. Patients typically present after 6 weeks of age with failure to thrive and a holosystolic murmur on physical examination (pulmonary vascular resistance drops at this time, allowing the left-to-right shunt of VSD to manifest). As with any left-to-right shunt, if untreated VSD may lead to severe pulmonary hypertension with eventual reversal of flow across the shunt, referred to as Eisenmenger’s physiology.
Atrial septal defect (ASD). As with VSD, radiographic findings may be absent with ASD. Larger ASDs, however, are associated with mild cardiomegaly, enlarged right atrium, normal to enlarged main pulmonary artery, and shunt vascularity. In contrast to an isolated VSD, the left atrium is not enlarged with an ASD. Patients with ASD usually present at an older age than those with VSD, since there is relatively little blood flow across this lower pressure shunt. ASDs are more likely to be clinically occult, and therefore patients are more likely to have severe pulmonary hypertension at presentation.
Patent ductus arteriosus (PDA). The ductus arteriosus normally closes in the perinatal period. Failure to close results in continued left-to-right shunting of blood across the ductus. As an isolated lesion, PDA is commonly seen in premature infants. Radiographic findings include variable degrees of cardiomegaly and shunt vascularity. Over time, left atrial and left ventricular enlargement may develop. When associated with more complex congenital heart disease, PDA may be necessary for survival.
Additional Differential Diagnosis
Atrioventricular canal defect (aka endocardial cushion defect). This anomaly is characterized by failure of the atrial and ventricular septa to develop fully; the mitral and/or tricuspid valves are abnormal as well. Nearly 50% of patients have trisomy 21. As with other left-to-right shunts, radiographic findings include cardiomegaly with a squared, enlarged right atrial border, pulmonary artery enlargement, and shunt vascularity.
Diagnosis
Ventricular septal defect.
Pearls
Ventricular septal defect is the most common septal defect; larger lesions result in cardiomegaly and shunt vascularity.
Patients with atrial septal defect typically present at a later age than ventricular septal defect due to less flow across the shunt.
Patent ductus arteriosus commonly occurs in premature infants, as well as patients with complex congenital heart disease.
Nearly half of patients with an atrioventricular canal (endocardial cushion defect) have trisomy 21.
Suggested Readings
Ferguson EC, Krishnamurthy R, Oldham SA. Classic imaging signs of congenital cardiovascular abnormalities. Radiographics. 2007; 27(5):1323–1334 Kellenberger CJ, Yoo SJ, Büchel ER. Cardiovascular MR imaging in neonates and infants with congenital heart disease. Radiographics. 2007; 27(1):5–18 Lapierre C, Déry J, Guérin R, Viremouneix L, Dubois J, Garel L. Segmental approach to imaging of congenital heart disease. Radiographics. 2010; 30(2):397–411 Schweigmann G, Gassner I, Maurer K. Imaging the neonatal heart-essentials for the radiologist. Eur J Radiol. 2006; 60(2):159–170Case 8

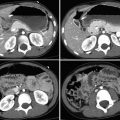
Key Imaging Finding
Congestive heart failure (CHF) in an infant.
Top Three Differential Diagnoses
Hypoplastic left heart syndrome (HLHS). Underdevelopment of the left heart causes CHF during the first 2 days of life. The principal feature is a very small left ventricle and atresia or stenosis of the aortic valve. In severe cases, the mitral valve may be stenotic, the left atrium small, and the ascending aorta hypoplastic. Most blood leaves the left heart by an obligatory patent foramen ovale (PFO) or atrial septal defect (ASD) to the right heart. It recirculates through pulmonary vasculature, reaching the body via a patent ductus arteriosus (PDA). However, as pulmonary vascular resistance drops and the PDA closes, blood floods the pulmonary vasculature, leading to CHF and systemic hypoperfusion. X-rays are initially normal, but cardiomegaly and vascular congestion develop within a few days.
Aortic coarctation (AC). There are two types of AC. The less common, “tubular,” form causes CHF in infants. Also called preductal coarctation, this consists of long segment aortic narrowing beyond the origin of the innominate artery, along with focal constriction before the ductus arteriosus. The aortic valve is often abnormal as well. Neonates present with shock and weak pulses, and chest radiographs show CHF. The more common, localized form of AC presents in older children. This form usually occurs just beyond the origin of the left subclavian artery or ligamentum arteriosum. The brachial pulses are normal, but the femoral pulses are weak. Chest X-ray in localized AC may show the “figure of 3,” caused by proximal dilatation of the left subclavian artery and aorta, narrowing at the site of stenosis, and then poststenotic dilatation. AC diagnosed in patients older than 8 years may show notching of ribs 4 through 8 due to collateral blood flow.
Critical aortic valvular stenosis. Most cases of aortic valvular stenosis are diagnosed in later life, but in about 10% the stenosis is so severe that CHF develops in the first 24 hours. In these patients, severely increased left ventricular pressure leads to decreased subendocardial oxygen supply and myocardial ischemia. Radiographs show cardiomegaly and vascular congestion. Echocardiography is diagnostic.
Additional Differential Diagnoses
Systemic overcirculation. Infants with hepatic hemangioendothelioma, intracranial arteriovenous (AV) malformation with aneurysmal dilatation of the vein of Galen, or other systemic AV shunts may present with high-output CHF. In this setting, cardiac anatomy is normal but unable to cope with increased blood volume.
Endocardial fibroelastosis. This rare condition usually presents with CHF by age 6 months. It may be primary or it may complicate congenital cardiac diseases, such as HLHS and aortic stenosis, or it may complicate congenital cardiac diseases, such as HLHS and aortic stenosis. Fibrous and elastic tissue in the endocardium and subendocardium is increased, leading to thickening of the heart wall and impaired myocardial contractility. The myocardium appears unusually echogenic at echocardiography. Chest radiography shows CHF. The heart is usually dilated but may be contracted.
Diagnosis
Hypoplastic left heart.
Pearls
Hypoplastic left heart is a spectrum of disorders characterized by underdevelopment of the left side of the heart; it leads to CHF in the first few days of life.
Tubular, preductal aortic coarctation is much less common than the localized form and leads to CHF in neonates.
The myocardium affected by endocardial fibroelastosis is extremely echogenic.
Suggested Readings
Ferguson EC, Krishnamurthy R, Oldham SA. Classic imaging signs of congenital cardiovascular abnormalities. Radiographics. 2007; 27(5):1323–1334 Schweigmann G, Gassner I, Maurer K. Imaging the neonatal heart: essentials for the radiologist. Eur J Radiol. 2006; 60(2):159–170Case 9

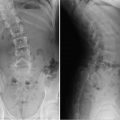
Key Imaging Finding
Unilateral small dense lung.
Top Three Differential Diagnoses
Atelectasis. It is important to establish whether there is increased or decreased volume of a dense lung and/or pleural space. Shift of the mediastinum toward the denser side indicates ipsilateral decreased volume. This most often results from atelectasis of all or part of the lung. Atelectasis usually affects only one lobe or lobar segment. However, unilateral atelectasis of an entire lung may be seen in patients with asthma, mucus plugging, a foreign body lodged in the mainstem bronchus, a misplaced endotracheal tube, hilar lymphadenopathy, mediastinal mass, and a variety of other pathologies.
Unilateral pulmonary hypoplasia/aplasia. Hypoplastic lung is differentiated from aplastic lung by the presence of underdeveloped parenchyma and hypoplastic vessels; both have rudimentary bronchi. Isolated primary pulmonary hypoplasia, which is most common, usually affects the left lung. Pulmonary hypoplasia/aplasia may be primary or secondary. If primary, there is no identifiable cause, other than hypoplasia of bronchovascular structures. Secondary cases may result from such space-occupying lesions as an ipsilateral mass or congenital diaphragmatic hernia and chest wall deformity. Oligohydramnios or impaired diaphragm motion usually affects both lungs; large masses or hernias and thoracic dystrophy also cause bilateral pathology. CT differentiates between hypoplasia, aplasia, and (much rarer) complete agenesis.
Hypogenetic lung (scimitar) syndrome. The scimitar vein differentiates scimitar syndrome from simple pulmonary hypoplasia/aplasia. This vein drains all or part of the lung, usually into the inferior vena cava but sometimes into a portal or hepatic vein. Its diameter increases as it descends, resembling the Turkish sword. The syndrome consists of the combination of a scimitar vein with lung hypoplasia (virtually always the right), cardiac dextroposition, and right pulmonary artery hypoplasia. The abdominal aorta supplies the affected lung. About one-fourth of patients have other cardiac pathology, but isolated small lesions are usually asymptomatic.
Additional Differential Diagnosis
Hyperinflation of the contralateral lung. Mass effect from hyperinflation may lead to volume loss or hypoplasia of the contralateral lung. This may result from air trapping due to an aspirated foreign body. Congenital lobar hyperinflation (CLH) may also cause contralateral mediastinal shift. If the pathology affects only one lobe (usually the case with CLH), there will be adjacent increased density due to compressive atelectasis of the unaffected ipsilateral lobe. However, if the entire lung is hyperinflated, it may be difficult to decide whether the small-volume dense or large-volume lucent side is abnormal. CT may assist with diagnosis.
Diagnosis
Scimitar syndrome.
Pearls
Mediastinal shift toward a dense lung usually indicates atelectasis or hypoplasia, but it may result from hyperinflation of the contralateral lung.
Asthma, mucus plugging, foreign body, or a misplaced endotracheal tube are common causes of ipsilateral atelectasis.
Isolated pulmonary hypoplasia affects the left side more often than the right side.
Scimitar syndrome virtually always affects the right lung and consists of an aberrant draining vein (scimitar), pulmonary hypoplasia, cardiac dextroposition, and hypoplasia of the associated pulmonary artery.
Suggested Readings
Lee EY, Dorkin H, Vargas SO. Congenital pulmonary malformations in pediatric patients: review and update on etiology, classification, and imaging findings. Radiol Clin North Am. 2011; 49(5):921–948Case 10

Key Imaging Finding
Neonatal lung disease with diffuse granular opacities.
Top Three Differential Diagnoses
Surfactant deficiency. Surfactant deficiency is the most common cause of respiratory distress in preterm infants, especially in those born before 34 weeks of gestation and who weigh less than 1.5 kg. It occurs because immature lungs are unable to produce enough surfactant to keep alveoli open for effective air exchange. Clinical manifestations of grunting, nasal flaring, subcostal retractions, tachypnea, and cyanosis are seen shortly after delivery, and almost always within the first 8 hours of life. Radiographs typically show diffusely hazy, low-volume lungs with air bronchograms. The granularity results from diffuse alveolar collapse, while the air bronchograms represent normal air-filled prealveolar airways. In severe cases (extreme prematurity and very low birth weight), assisted ventilation along with surfactant application may be needed to achieve acceptable gas exchange. Potential complications of positive pressure ventilation include pulmonary interstitial emphysema (PIE), pneumomediastinum, and pneumothorax. Chronic intubation and oxygen administration may eventually result in bronchopulmonary dysplasia (BPD).
Neonatal pneumonia. Bacterial pneumonias, especially those caused by group B Streptococcus, predominate in the neonatal period. The more common route of infection is through the birth canal, especially after early rupture of membranes in febrile mothers who are positive for this organism. Since neonatal pneumonia is usually not lobar in distribution, X-ray findings of diffuse haziness and granularity with low lung volumes may mimic surfactant deficiency. However, in patients with neonatal pneumonia caused by organisms other than group B Streptococcus, lung volumes are usually normal to slightly expanded (even without mechanical ventilation) due to exudate-filled and distended alveoli. Pleural effusions are rare in surfactant deficiency but are seen in as many as two-thirds of patients with neonatal pneumonia. With adequate antibiotic therapy, complications such as empyema, pulmonary abscess, and pneumatocele are unusual.
Transient tachypnea of the newborn (TTNB). This is the most common cause of respiratory distress in a newborn. Transient and benign, TTNB occurs when immature lymphatic vessels cannot absorb residual lung fluid quickly. Radiographs typically demonstrate central streaky opacities and small pleural effusions, with fluid in the minor fissure. Patients improve clinically within 48 hours of birth, and radiographs normalize within 72 hours. Treatment is limited to supportive care and observation.
Diagnosis
Surfactant deficiency.
Pearls
Surfactant deficiency is the most common cause of respiratory distress in preterm infants.
Neonatal pneumonia may mimic surfactant deficiency, but neonatal pneumonia often has pleural effusions.
Transient tachypnea of the newborn is transient and shows rapid clinical improvement; radiographs are normal at 72 hours.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree