Part 4 Musculoskeletal Imaging
Case 90

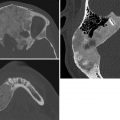
Key Imaging Finding
Short rib skeletal dysplasia.
Top Three Differential Diagnoses
Asphyxiating thoracic dystrophy (Jeune syndrome). In this syndrome, the thorax is long and bell-shaped, with short, horizontal ribs that flare anteriorly. This configuration results in early respiratory compromise. Dysplastic acetabula resembling an upside-down trident are often seen. There is associated mild acromelic (distal) limb shortening, but long bones are not bowed. A normal spine and trident acetabula help differentiate this condition from thanatophoric dysplasia.
Ellis–van Creveld syndrome (chondroectodermal dysplasia). Hair, nail, and teeth abnormalities are clinical hallmarks of this syndrome. There is progressive mesomelic (middle—tibial and radial) and acromelic (distal) limb shortening. The fibulae are markedly shortened. Radiographic features also include short ribs, fused capitate and hamate, cone-shaped epiphyses, and postaxial polydactyly. The femoral heads ossify prematurely, and the pelvis is abnormal, with flared iliac wings and a trident acetabulum. Congenital heart disease, typically atrial septal defect or atrioventricular cushion defect, is the major cause of morbidity.
Short rib polydactyly. In this condition, the ribs are extremely short. Polydactyly may be either preaxial or postaxial. The pelvis and spine appear fairly normal, and long bones are normal. However, there may be cleft palate, hypoplastic epiglottis, cystic kidneys, and fetal hydrops.
Additional Differential Diagnoses
Thanatophoric dysplasia. Thanatophoric dysplasia is the most common lethal skeletal dysplasia and is uniformly fatal in the neonatal period. The ribs are very short, and as a result the thorax is narrow. Lung hypoplasia causes respiratory failure. Patients with this disproportionate dwarfism have severe platyspondyly but wide intervertebral disks, leading to normal trunk length. The head is disproportionately large, and some patients have cloverleaf skull. Iliac bones are small. There is rhizomelic (proximal) limb shortening. Long bones are bowed and short. The femurs have a characteristic “telephone receiver” appearance.
Holt–Oram syndrome. Like Ellis–van Creveld syndrome, this condition is characterized by cardiac disease (usually an atrial or ventricular septal defect) and limb abnormalities. However, the ribs are normal. The thumb is usually duplicated, hypoplastic, or triphalangeal. The radius is often hypoplastic, and there may be other anomalies of the shoulder and upper extremity.
Diagnosis
Ellis–van Creveld syndrome.
Pearls
Jeune syndrome (asphyxiating thoracic dysplasia) demonstrates a bell-shaped thorax, trident acetabula, and normal spine.
Patients with Ellis–van Creveld syndrome have cardiac disease as well as progressive limb shortening, short ribs, and postaxial polydactyly.
Bones in patients with short rib polydactyly are otherwise normal.
Suggested Readings
Glass RB, Norton KI, Mitre SA, Kang E. Pediatric ribs: a spectrum of abnormalities. Radiographics. 2002; 22(1):87–104 Miller E, Blaser S, Shannon P, Widjaja E. Brain and bone abnormalities of thanatophoric dwarfism. AJR Am J Roentgenol. 2009; 192(1):48–51 Panda A, Gamanagatti S, Jana M, Gupta AK. Skeletal dysplasias: a radiographic approach and review of common non-lethal skeletal dysplasias. World J Radiol. 2014; 6(10):808–825 Parnell SE, Phillips GS. Neonatal skeletal dysplasias. Pediatr Radiol. 2012; 42 Suppl 1:S150–S157Case 91

Key Imaging Finding
Abnormal epiphyses.
Top Three Differential Diagnoses
Spondyloepiphyseal dysplasia (SED). SED “congenita” manifests at birth with absent calcaneal, knee, and pubic bone ossification, pear-shaped vertebrae, and short, broad iliac wings. Severe platyspondyly develops, with thin intervertebral disks. SED “tarda” usually manifests at age 5 to 10 years with platyspondyly (including hump-shaped posterior vertebral bodies), small pelvis, and mildly to moderately small, irregular epiphyses.
Chondrodysplasia punctata. There are two common subtypes, both characterized by stippled epiphyses at birth. The autosomal-recessive form shows symmetrical rhizomelic shortening, stippling in the large joints, and sometimes stippling of laryngeal and tracheal cartilage. Coronal clefts are seen in vertebrae. The hands and feet are normal. The X-linked dominant type, “Conradi–Hünermann,” shows occasional and asymmetrical limb shortening and involvement of the hands and feet as well as the large joints. The larynx and trachea are normal, but vertebral bodies and endplates are stippled, leading to eventual kyphoscoliosis. Stippling resolves over time, and the patients have a normal life span. Mental retardation is a feature of the lethal form but not Conradi–Hünermann syndrome.
Spondyloepimetaphyseal dysplasia. This dysplasia resembles multiple epiphyseal dysplasia, but there is concomitant metaphyseal involvement.
Additional Differential Diagnoses
Multiple epiphyseal dysplasia. This genetically heterogeneous disorder presents after age 2 to 4 years. Bilateral and symmetrical delayed and fragmented epiphyses of long bones and distal extremities are characteristic. Pronounced wedging of distal tibial epiphysis may trigger the diagnosis. The spine resembles Scheuermann disease, with endplate irregularities, slight anterior wedging, and numerous Schmorl nodes.
Morquio syndrome. A mucopolysaccharidosis, Morquio syndrome is characterized by delayed ossification of femoral heads, irregular epiphyses, and secondary metaphyseal widening. Other bones are involved as well—notably the spine, where there is platyspondyly with anterior beaking of the mid portion of vertebral bodies. The bases of the second through fifth metacarpals are pointed and clustered together. Ribs have a paddle appearance.
Diagnosis
Chondrodysplasia punctata.
Pearls
Spondyloepiphyseal dysplasia tarda manifests during childhood with mild to moderately small, irregular epiphyses and platyspondyly with hump-shaped posterior vertebral bodies.
A wedged, slightly small distal tibial epiphysis is a clue to the diagnosis of multiple epiphyseal dysplasia.
With Morquio syndrome, ossification of the femoral heads is delayed, and there are multiple irregular epiphyses; as with Hurler syndrome, there is anterior vertebral body beaking.
The autosomal-recessive type of chondrodysplasia punctata has stippled epiphyses of large joints and less involvement of the axial skeleton, whereas with Conradi–Hünermann syndrome the spine, hands, and feet may be affected as well.
Suggested Readings
Panda A, Gamanagatti S, Jana M, Gupta AK. Skeletal dysplasias: a radiographic approach and review of common non-lethal skeletal dysplasias. World J Radiol. 2014; 6(10):808–825 Parnell SE, Phillips GS. Neonatal skeletal dysplasias. Pediatr Radiol. 2012; 42 Suppl 1:S150–S157Case 92

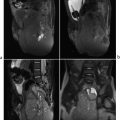
Key Imaging Finding
Dense bones.
Top Three Differential Diagnoses
Osteopetrosis. Osteopetrosis refers to a rare, heterogeneous group of heritable diseases. All have increased predominantly medullary bone density and sclerosis, due to impaired osteoclast differentiation/function. Patients often present with fractures, as the bones are relatively inelastic. The skull may have a “hair-on-end” appearance in older patients. Vertebral bodies have a “sandwich” appearance, with a sharp transition between the sclerotic endplates and the relatively lucent center (unlike the “rugger jersey” spine of renal osteodystrophy, which has an ill-defined transition). A “bone-withinbone” appearance may be seen at the pelvis and long bones. Characteristic radiolucent bands may alternate with areas of increased density in the metaphyses. The appendicular skeleton may also be diffusely dense, with flaring at the metaphyses of long bones (“Erlenmeyer flask” deformity). Marrow crowding leads to extramedullary hematopoiesis and splenomegaly. If children are not treated with bone marrow transplantation, overwhelming infection and other complications of bone marrow suppression generally prove fatal. However, patients with adult-onset disease have normal life expectancy.
Osteopoikilosis. Also known as “spotted bones,” osteopoikilosis is a diagnosis of exclusion. Existing in hereditary and sporadic forms, osteopoikilosis is caused by defective endochondral bone formation in the long and flat bones. Radiographs show multiple round, oval, or lenticular sclerotic foci in a periarticular distribution within the epiphyseal and metaphyseal regions. It is usually benign and asymptomatic. However, giant cell tumor, chondrosarcoma, osteosarcoma, and spinal stenosis have been reported. Osteopoikilosis must be differentiated from osteoblastic metastases and other sclerosing dysplasias.
Melorheostosis. This sporadic mesenchymal disorder is characterized by cortical and medullary hyperostosis along a sclerotome, leading to undulating longitudinal sclerosis that resembles dripping candle wax. The axial skeleton is generally spared. Melorheostosis is often asymptomatic in childhood.
Additional Differential Diagnoses
Metastatic disease. Medulloblastoma, neuroblastoma, and lymphoma may present with sclerotic osseous metastases. Skeletal metastases from other pediatric tumors are typically lytic.
Fluorosis. This metabolic disorder is caused by ingestion or inhalation of large amounts of fluoride, causing increased bone turnover, impaired collagen synthesis, and irregular osteoid deposition. Fumes from household coal-burning stoves along with high fluoride levels in water may lead to this disorder. Classic X-ray appearance includes increased bone density, blurred trabeculae, periosteal bone formation, and ossification of attachments of tendons, ligaments, and muscles. Patients may develop areas of osteopenia.
Diagnosis
Osteopetrosis.
Pearls
Osteopetrosis is an inherited disorder characterized by diffuse sclerosis or “bone-within-bone” appearance, increased risk for fractures, and—in its most severe form—bone marrow failure.
Osteopoikilosis is characterized by multiple sclerotic lesions in a periarticular distribution.
Fluorosis results from ingestion or inhalation of large amounts of fluoride, with radiographs showing coarse trabeculae and diffuse sclerosis, predominantly within the axial skeleton.
Suggested Readings
Di Primio G. Benign spotted bones: a diagnostic dilemma. CMAJ. 2011; 183(4):456–459 Stark Z, Savarirayan R. Osteopetrosis. Orphanet J Rare Dis. 2009; 4:5 Wang Y, Yin Y, Gilula LA, Wilson AJ. Endemic fluorosis of the skeleton: radiographic features in 127 patients. AJR Am J Roentgenol. 1994; 162(1):93–98Case 93

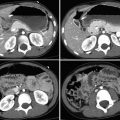
Key Imaging Finding
Multifocal osseous deformities.
Top Three Differential Diagnoses
Ollier disease. Ollier disease is a relatively rare nonhereditary enchondromatosis, characterized by intraosseous cartilaginous benign enchondromas located near the growth plate. Unilateral limb-length discrepancy and extremity bowing are common clinical findings. The enchondromas are usually distributed asymmetrically. The affected metaphysis and epiphysis may fuse prematurely, with resultant limb shortening. Radiographically, enchondromas appear as geographic, columnar radiolucent defects extending from the metaphysis into the diaphysis of the affected bone. Phalanges and metacarpals are involved most often. About 50% of enchondromas calcify with typical chondroid “snowflake” or “ring and arc” patterns. About 40% of patients with Ollier disease eventually develop chondrosarcoma. Patients may develop other tumors as well.
Maffucci syndrome. This extremely rare enchondromatosis presents with multiple enchondromas associated with soft-tissue venous malformations and potentially also lymphatic malformations. Clinical presentation is similar to that of Ollier disease but is distinguished by dermal raised bluish-red areas with obvious blood vessels and surrounding pallor. In addition to the enchondromas, calcifications within the soft-tissue venous malformations are a radiographic hallmark of this disease. In up to half of cases, enchondromas eventually transform into chondrosarcoma. The incidence of liver, pancreas, ovary, brain, and other tumors is increased.
Polyostotic fibrous dysplasia. Fibrous dysplasia is characterized by abnormal fibrous tissue that replaces normal bone. It may be monostotic or polyostotic, and may appear as a geographic lucency, as “ground glass” opacity, or as sclerosis. Osseous deformities may result, including “shepherd’s crook” configuration of the proximal femur. McCune–Albright syndrome is polyostotic fibrous dysplasia associated with such endocrine abnormalities as precocious puberty.
Diagnosis
Ollier disease.
Pearls
Enchondromatosis is characterized by asymmetrical distribution of radiolucent metaphyseal lesions.
Enchondromas originate in the metaphyses and may extend to the diaphysis as bone grows.
Chondroid calcifications are seen in about 50% of enchondromas.
Degeneration to chondrosarcoma is more common in Maffucci syndrome than in Ollier syndrome.
Suggested Readings
Foreman KL, Kransdorf MJ, O’Connor MI, Krishna M. AIRP best cases in radiologic-pathologic correlation: Maffucci syndrome. Radiographics. 2013; 33(3):861–868 Kumar A, Jain VK, Bharadwaj M, Arya RK. Ollier disease: pathogenesis, diagnosis and management. Orthopedics. 2015; 38(6):e497–e506 Silve C, Jüppner H. Ollier disease. Orphanet J Rare Dis. 2006; 1:37 Vlychou M, Athanasou NA. Radiological and pathological diagnosis of paediatric bone tumours and tumour-like lesions. Pathology. 2008; 40(2):196–216Case 94

Key Imaging Finding
Erlenmeyer flask deformity.
Top Three Differential Diagnoses
Multiple hereditary exostoses. Osteochondromatosis is an autosomal-dominant dysplasia. As with solitary lesions, the cortex of the lesions is continuous with the underlying bone. Lesions that cause Erlenmeyer flask deformity tend to be sessile rather than pedunculated. Complications include growth disturbance, pain due to compression of neurovascular bundles, and—rarely—malignant transformation.
Fibrous dysplasia. Fibrous dysplasia may be monostotic or polyostotic. Lesions typically arise in the central part of the bone and are expansile; they rarely involve the epiphysis. Density varies depending on the amount of osseous and fibrous tissue, but the classic lesion has a ground glass matrix and thin cortex. Pathological fracture is the most common complication. The polyostotic form is more aggressive and often affects one side of the body. Associated disorders include McCune–Albright (precocious puberty and café au lait spots) and Mazabraud (intramuscular myxomas) syndromes.
Hemoglobinopathy. The most common hemoglobinopathies include sickle cell disease and the thalassemias. Bony changes in these conditions are due to marrow hyperplasia and vascular occlusion. Marrow hyperplasia causes osteopenia, hair-on-end appearance of the skull, and remodeling. Vascular occlusion may cause avascular necrosis, bone infarcts, and dactylitis. Physeal involvement may lead to growth disturbance.
Additional Differential Diagnoses
Osteopetrosis. Osteopetrosis is an inherited disorder caused by failure of osteoclast function. As a result, primary spongiosa accumulates in the medullary space. In addition to Erlenmeyer flask deformity, findings include increased bone density, encroachment on the medullary space, bone-in-bone appearance, and alternating dense and lucent metaphyseal bands. Complications include fractures, anemia, and thrombocytopenia.
Gaucher disease. Gaucher disease is a rare, inherited metabolic disorder caused by deficiency of a lysosomal enzyme. The deficiency leads to accumulation of glucosylceramide in reticuloendothelial cells, which infiltrate marrow spaces. Radiographs demonstrate osteopenia, medullary expansion, and remodeling. Complications include bone infarcts, avascular necrosis, and pathological fractures. MRI may be useful to determine the extent of marrow infiltration. Infiltrating cells have signal similar to hematopoietic marrow.
Diagnosis
Osteopetrosis.
Pearls
Sessile lesions associated with multiple hereditary exostoses may cause Erlenmeyer flask deformity.
Fibrous dysplasia may be monostotic or polyostotic; the classic lesion has a ground glass matrix and thin cortex.
Hemoglobinopathies (sickle cell and thalassemias) result in marrow hyperplasia, expansion, and infarcts.
Osteopetrosis results from osteoclast failure, leading to dense but fragile bones.
Suggested Readings
Ihde LL, Forrester DM, Gottsegen CJ, et al. Sclerosing bone dysplasias: review and differentiation from other causes of osteosclerosis. Radiographics. 2011; 31(7):1865–1882 Katz R, Booth T, Hargunani R, Wylie P, Holloway B. Radiological aspects of Gaucher disease. Skeletal Radiol. 2011; 40(12):1505–1513 Khanna G, Bennett DL. Pediatric bone lesions: beyond the plain radiographic evaluation. Semin Roentgenol. 2012; 47(1):90–99 States LJ. Imaging of metabolic bone disease and marrow disorders in children. Radiol Clin North Am. 2001; 39(4):749–772Case 95

Key Imaging Finding
Pseudarthrosis.
Top Three Differential Diagnoses
Posttraumatic deformity. Nonunion is most common in fractures that were initially not recognized and/or inadequately reduced. The lateral condyle of the elbow is most often affected, sometimes leading to angular deformity. The patient should have a clinical history of traumatic fracture. In Salter–Harris fractures, lateral bowing may ensue if medial growth is halted and lateral growth continues. Radiographs will show normal bone adjacent to the pseudarthrosis, rather than the smooth, tapered margins commonly seen with either neurofibromatosis type 1 (NF1) or non-NF1 congenital pseudarthrosis.
NF1. Tibial pseudarthrosis develops in up to 10% of patients with NF1, and about 50% of cases of tibial pseudarthrosis are associated with NF1. The fibula is affected less often than the tibia. Other bones may be affected as well. Pseudarthrosis usually occurs at the junction between the middle and distal thirds of the diaphysis. Considered congenital, it is usually diagnosed by age 2 years and may be apparent at birth. More often, dysplastic bone is bowed at birth, usually anterolaterally; bowing progresses, leading to pathological fracture as the child bears weight. If the abnormal bone fails to heal, pseudarthrosis results. Hamartomatous fibrous proliferation is found at the site of pseudarthrosis. The pseudarthrosis appears as a transverse defect with smooth, sclerotic margins. Unlike in posttraumatic pseudarthrosis, the adjacent tibia may appear thin, sclerotic, tapered, or cystic. Serial imaging shows no evidence of callus formation. MRI shows hypointense periosteum intact across the pseudarthrosis. Treatment is challenging, and residual deformity is common. Satisfactory healing is more likely if patients are older at presentation. Other relatively common osseous manifestations of NF1 include calvarial defects, dysmorphic vertebrae, scoliosis and kyphosis, and thin, ribbonlike ribs. Nonossifying fibromas are often numerous. NF1 is diagnosed on the basis of the presence of at least two of the following diagnostic criteria: at least six café au lait large macules, neurofibromas, axillary/groin freckling, optic pathway gliomas, Lisch nodules, bony dysplasia, and/or a first-degree affected relative.
Non-neurofibromatosis (non-NF1) congenital pseudarthrosis. Fifty percent of cases of pseudarthrosis are not associated with NF1. As with NF1, patients may present at birth with apex anterolateral tibial bowing or with a bony defect due to pseudarthrosis. Some present as infants, when an area of weak bone fractures and does not heal, resulting in pseudarthrosis. The appearance is indistinguishable from pseudarthrosis in patients with NF1. A thorough systemic and familial evaluation is necessary to determine the presence of NF1 diagnostic criteria (see above).
Diagnosis
Tibial pseudarthrosis in a patient with neurofibromatosis type 1.
Pearls
Congenital pseudarthrosis in patients with or without neurofibromatosis type 1 typically develops in an area of bowed, dysplastic bone.
Fifty percent of congenital pseudarthroses are associated with neurofibromatosis type 1.
The presence or absence of associated diagnostic criteria is important for determining whether a pseudarthrosis is isolated or associated with neurofibromatosis type 1, since the radiographic appearance is similar.
Posttraumatic pseudarthrosis is most common at the lateral condyle of the elbow.
Suggested Readings
Feldman DS, Jordan C, Fonseca L. Orthopaedic manifestations of neurofibromatosis type 1. J Am Acad Orthop Surg. 2010; 18(6):346–357 Pannier S. Congenital pseudarthrosis of the tibia. Orthop Traumatol Surg Res. 2011; 97(7):750–761 Patel NB, Stacy GS. Musculoskeletal manifestations of neurofibromatosis type 1. AJR Am J Roentgenol. 2012; 199(1):W99–W106Case 96

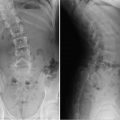
Key Imaging Finding
Posterior vertebral body scalloping.
Top Three Differential Diagnoses
Dural ectasia. Dural ectasia refers to enlargement or widening of the dural sac. Common causes include connective tissue disorders, such as Marfan and Ehlers–Danlos syndromes, and neurofibromatosis (NF). The weak dura transmits pressure along the posterior aspect of the vertebral bodies, with resultant posterior vertebral body scalloping. In patients with NF, masses such as neurofibromas and thoracic meningoceles may also cause posterior vertebral body scalloping. Patients with Marfan and Ehlers–Danlos syndromes are prone to connective tissue abnormalities elsewhere, such as aneurysms. NF patients may have cutaneous and neurological manifestations of the disease.
Mucopolysaccharidosis (MPS). These inherited disorders are caused by deficiencies in lysosomal enzymes necessary to break down certain complex carbohydrates. This leads to excessive accumulation and deposition of lysosomal glycosaminoglycans. Patients often present with short stature, craniofacial abnormalities, and in some cases mental retardation. There are multiple variants of MPS, with Hurler and Morquio syndromes being the most common. Both syndromes are associated with diffuse posterior vertebral scalloping, but the mechanism is not established. Those with Hurler syndrome also demonstrate anterior beaking of the inferior aspect of the vertebral body, while patients with Morquio syndrome have anterior beaking in the midportion of the vertebral body. An enlarged, J-shaped sella is classically seen with Hurler syndrome.
Skeletal dysplasia/achondroplasia. Achondroplasia is a common skeletal dysplasia, with autosomal-dominant inheritance. Radiographic findings include a large skull with narrow foramen magnum, spinal stenosis, squared iliac wings, progressively decreasing interpediculate distance in the lumbar spine, flat acetabula, short metacarpals, and short ribs. Posterior vertebral body scalloping is common and believed to be an adaptive response to congenital spinal stenosis. Posterior scalloping is also associated with metatropic dwarfism and osteogenesis imperfecta.
Additional Differential Diagnoses
Spinal tumor. Intrathecal tumors may cause increased pressure within the spinal canal, leading to compensatory posterior vertebral body scalloping. The level of the vertebral scalloping typically corresponds to the location of the tumor. Common primary spinal cord tumors include ependymoma (most common primary cord tumor in adults) and astrocytoma (most common spinal cord tumor in children). Lipomas, dermoids/epidermoids, and perineural cysts may also lead to mass effect and vertebral body scalloping.
Normal variant. When mild and not associated with other skeletal abnormalities, posterior vertebral body scalloping may be a normal variant. Patients are typically followed after other causes are excluded.
Diagnosis
Mucopolysaccharidosis (Hurler syndrome).
Pearls
Dural ectasia with posterior vertebral body scalloping occurs in connective tissue disorders and neurofibromatosis.
Mucopolysaccharidoses (Hurler and Morquio syndromes) show posterior scalloping and anterior beaking of the vertebral body.
Intrathecal tumors may show focal posterior vertebral scalloping (and wide interpediculate distance).
Mild posterior vertebral body scalloping may be a normal developmental variant.
Suggested Readings
Lachman R, Martin KW, Castro S, Basto MA, Adams A, Teles EL. Radiologic and neuroradiologic findings in the mucopolysaccharidoses. J Pediatr Rehabil Med. 2010; 3(2):109–118 Wakely SL. The posterior vertebral scalloping sign. Radiology. 2006; 239(2):607–609Case 97

Key Imaging Finding
Limb deficiency.
Top Three Differential Diagnoses
Longitudinal deficiency of the fibula. In this condition, the fibula may be partly or completely absent, or it may simply be mildly hypoplastic. The anomaly is often accompanied by proximal focal femoral deficiency, coxa vara, clubfoot, and absent lateral rays. The remainder of the skeleton is usually normal. Perhaps counterintuitively, femoral abnormalities are more common with a hypoplastic fibula than with one that is completely absent. A cartilaginous fibular anlage is often present, which tethers growth of the tibia. If the hip and/or femur is clearly abnormal as well, the diagnosis may be made in utero. If the fibula is absent or markedly hypoplastic, X-ray diagnosis is straightforward. The tibia is often bowed, short, and thick. However, subtle cases are diagnosed by an abnormally high distal fibular physis (above the proximal tibial physis). Treatment is directed at establishing a usable weight-bearing lower extremity and often involves amputation. Longitudinal deficiency of the tibia is much less common than that of the fibula.
Longitudinal deficiency of the radius. This sporadic condition usually consists of complete absence of the radius. However, the deficiency may be more limited and is occasionally manifested only by absence or hypoplasia of the thumb. Onethird of patients are otherwise normal, but one-third have a syndrome, such as thrombocytopenia-absent radius (TAR), Vertebral anomalies, Anal atresia, Cardiac defects, Tracheo-Esophageal fistula, Renal anomalies, with or without Limb malformations (VACTERL), or Holt–Oram syndrome. One-third have nonsyndromic-associated bone anomalies, with the likelihood of this increasing with the severity of deficiency. The radius is partly or (more often) completely absent, and the thumb is hypoplastic or absent. The ulna is short and bowed. If the radius is partially present, it may be fused with the ulna, and the radial head is often congenitally dislocated. The hand may be at a right angle to the forearm (radial clubhand).
Proximal focal femoral deficiency (PFFD). This nonhereditary malformation ranges from mild dysgenesis of the proximal femur to near-complete absence of the entire bone. Usually isolated and unilateral, it may be part of caudal regression syndrome. The tibia and fibula may be hypoplastic as well. The condition is classified according to the presence of the femoral head, connection between the femoral head and the shaft (bony, cartilaginous, or absent), and extent of acetabular dysplasia. US and MRI assess nonossified structures.
Additional Differential Diagnosis
Longitudinal deficiency of the ulna. At least part of the ulna is usually present in this disorder, which is more common in boys, usually on the right, and infrequently bilateral. Anomalies of the hand, wrist, and elbow bones are more severe than with radial deficiency. Carpal bones and digits are often missing or fused. Clubhand alignment is uncommon. Remote bony anomalies are common, including scoliosis, phocomelia, and PFFD. Other organ systems are usually normal. X-rays usually show a hypoplastic ulna, with ossification sometimes delayed until age 2 years. The radius appears bowed and short. The radial head may be normal, dislocated, or fused to the humerus. The rays are often deficient or fused.
Diagnosis
Longitudinal deficiency of the radius with clubhand.
Pearls
Mild cases of fibular longitudinal deficiency are diagnosed by an unusually high distal fibular physis.
One-third of patients with longitudinal deficiency of the radius have an accompanying syndrome.
US and MRI are useful for evaluating nonossified cartilaginous structures in proximal focal femoral deficiency.
Suggested Readings
Birch JG, Lincoln TL, Mack PW, et al. Congenital fibular deficiency: a review of 30 years’ experience at one institution. J Bone Joint Surg Am. 2011; 93:1144–1151 Stein-Wexler R. The elbow and forearm: congenital and developmental conditions. In Stein-Wexler R, Wootton-Gorges SL, Ozonoff MB, eds. Pediatric Orthopedic Imaging. Berlin/Heidelberg: Springer; 2015:159–186Case 98

Key Imaging Finding
Genu varum.
Top Three Differential Diagnoses
Physiological bowing. Tibial bowing is a common normal developmental finding until age 2 years, but it does increase the risk of developing pathological tibia vara. It results from either intrauterine molding or delayed transition to normal mild genu valgus. Measurement depends on the tibiofemoral angle, which is the angle subtended by lines drawn longitudinally to the diaphyses. In infants, up to 16 to 20 degrees of varus angulation at the knee is normal, but by about age 3 years this should change to 10-degree valgus. Images show prominent but nonfragmented medial proximal tibial beaks. Distal femoral and proximal tibial medial epiphyses are wedge-shaped. Medial cortical thickening of femurs and tibias resolves as the bones straighten.
Blount disease (tibia vara). Obesity or early walking stresses the posteromedial proximal tibial metaphysis, leading to deformity of the epiphysis and physeal damage due to shearing stress. Like developmental bowing, this condition is more common in African-Americans. Infantile Blount disease presents before age 4 years, whereas juvenile and adolescent forms manifest in older children, likely constituting later presentations of the same disease. Infantile Blount disease is defined by a tibial metaphyseal/diaphyseal angle of at least 16 degrees. Early cases show only metaphyseal beaking, but as disease progresses the metaphysis becomes more irregular, depressed, and possibly fragmented. The tibia may subluxate laterally. Conservative treatment with orthoses is effective in mild cases of infantile Blount disease. Severe or delayed disease may be treated with realignment wedge osteotomy. MRI is primarily employed to evaluate for formation of a medial physeal bar, which, if present, mandates more complex surgery.
Rickets. Cartilage accumulates due to deficient growth plate cartilage and osteoid mineralization, leading to growth failure and osseous deformity. Nutritional vitamin D deficiency and X-linked hypophosphatemia are the most common underlying metabolic abnormalities. The growth plate widens due to dis-organized, excessive cartilage. The metaphyses and metaphyseal equivalents of rapidly growing bones are most severely affected: wrist, knees, and anterior ribs. Insufficiency fractures, periosteal new bone, and bowing are seen in the diaphyses. Lower extremity bowing develops as children begin to stand. In addition to bowing, X-rays show physeal widening and metaphyseal flaring, cupping, and fraying.
Additional Differential Diagnosis
Syndromic bowing. Metaphyseal chondrodysplasia, osteogenesis imperfecta, neurofibromatosis, and other syndromes may cause genu varum due to a variety of mechanisms.
Diagnosis
Blount disease.
Pearls
Genu varus up to 16 to 20 degrees is normal in children younger than 2 years of age.
Pathological tibia vara shows excess bowing in children younger than 2 years or bowing that persists beyond age 2 years.
In Blount disease, metaphyseal beaking progresses to irregularity and sometimes fragmentation with lateral subluxation of the tibia.
Rickets, commonly due to nutritional vitamin D deficiency or X-linked hypophosphatemia, shows physeal widening and metaphyseal cupping and fraying along with insufficiency fractures and diaphyseal bowing.
Suggested Readings
Cheema JI, Grissom LE, Harcke HT. Radiographic characteristics of lower-extremity bowing in children. Radiographics. 2003; 23(4):871–880 Ho-Fung V, Jaimes C, Delgado J, Davidson RS, Jaramillo D. MRI evaluation of the knee in children with infantile Blount disease: tibial and extra-tibial findings. Pediatr Radiol. 2013; 43(10):1316–1326 Shore RM, Chesney RW. Rickets: part I. Pediatr Radiol. 2013; 43(2):140–151 Shore RM, Chesney RW. Rickets: part II. Pediatr Radiol. 2013; 43(2):152–172Case 99

Key Imaging Finding
Tarsal coalition.
Top Three Differential Diagnoses
Talocalcaneal coalition. Talocalcaneal (or subtalar) and calcaneonavicular are the most common tarsal coalitions. They result from failure of segmentation of the hindfoot bony anlage during development. Fusion between the talus and calcaneus may be osseous (synostosis), cartilaginous (synchondrosis), or fibrous (syndesmosis). Talocalcaneal coalition is bilateral in about half of cases, and boys are affected more often than girls. Patients usually present around age 12 to 16 years, classically complaining of painful flatfoot. Some patients have pes cavus, however, and many are asymptomatic. X-ray findings include a distal talar beak and continuous “C” sign (a continuous arc formed by the medial outline of the talar dome and posteroinferior aspect of the sustentaculum tali) on the lateral view. There is narrowing or obliteration of the subtalar joint on the Harris–Beath view. CT and MRI (especially coronal) provide more precise evaluation of the extent of coalition. MRI is especially useful for defining fibrous or cartilaginous coalition.
Calcaneonavicular coalition. This fusion connects the calcaneus and navicular. Patients usually present at age 8 to 12 years, with symptoms similar to those for talocalcaneal coalition. Normal feet have no articulation between the calcaneus and the navicular, but in cases of coalition the anterior process of the calcaneus is elongated, providing an articulation with the inferolateral aspect of the navicular. The elongated anterior process results in the “anteater” sign, evident on the lateral view. The coalition itself is best seen on the oblique view. Radiographic findings on this view range from osseous apposition with a narrow articulation and marginal sclerosis (for fibrocartilaginous coalitions) to a solid bony bar connecting the calcaneus and navicular. Sagittal MRI facilitates detailed analysis of this coalition.
Talonavicular coalition. This unusual coalition connects the talus and navicular. It may be bilateral in 25% and if symptomatic usually presents before age 10 years.
Additional Differential Diagnosis
Other coalitions. Other or multiple coalitions are rare. They are often associated with congenital abnormalities such as longitudinal deficiency of the fibula or Apert syndrome.
Diagnosis
Talocalcaneal coalition.
Pearls
Talocalcaneal and calcaneonavicular coalitions are most common.
Talocalcaneal coalition may show a talar beak and continuous “C” on the lateral view, with narrowing or fusion of the subtalar joint on the Harris–Beath view.
Calcaneonavicular coalition may show an elongated anterior calcaneal process on the lateral view, and an osseous or fibrocartilaginous calcaneonavicular articulation on the oblique view.
CT and MRI allow more precise evaluation of type of coalition—fibrous, cartilaginous, osseous, or combined.
Suggested Readings
Iyer RS, Thapa MM. MR imaging of the paediatric foot and ankle. Pediatr Radiol. 2013; 43 Suppl 1:S107–S119 Lawrence DA, Rolen MF, Haims AH, Zayour Z, Moukaddam HA. Tarsal coalitions: radiographic, CT and MR imaging findings. HSS J. 2014; 10(2):153–166 Mosca VS. Subtalar coalition in pediatrics. Foot Ankle Clin. 2015; 20(2):265–281Case 100

Key Imaging Finding
Lucent metaphyses.
Top Three Differential Diagnoses
Leukemia. Acute leukemia is the most common pediatric malignancy, and acute lymphocytic leukemia comprises the majority of cases. Radiographic abnormalities are seen in up to two-thirds of patients at diagnosis. Metaphyseal lucencies are the most common finding and occur at sites of fastest growth, such as the knees, ankles, and wrists. Other findings include periosteal reaction, focal osteolytic lesions, osteopenia, and fractures. Compression fractures of the spine are common.
Osteomyelitis. Acute osteomyelitis is a significant cause of bone pathology in children, especially those younger than 5 years. Most cases are due to hematogenous spread and involve the metaphyses. Scintigraphy and MRI are more sensitive than radiographs for early diagnosis. After about 10 days, radiographic findings such as ill-defined metaphyseal lucencies and periosteal bone formation may be seen.
Neuroblastoma. Neuroblastoma commonly metastasizes to bone. Children with skeletal metastases may complain of bone pain and arthritis-like symptoms. Radiographic appearance resembles that of other small round blue cell tumors, such as Ewing sarcoma and leukemia. There may be periosteal reaction, one or more lytic foci, lucent horizontal metaphyseal lines, and pathological fractures. MRI, positron emission tomographic CT (PET-CT), and metaiodobenzylguanidine (MIBG) scans help assess for metastases.
Additional Differential Diagnoses
TORSCH. TORSCH (toxoplasmosis, rubella, syphilis, cytomegalovirus [CMV], herpes) infections are acquired transplacentally and often affect the metaphyses. Syphilis and others may cause symmetrical lucent metaphyseal bands adjacent to a subphyseal dense band. Wimberger sign—symmetrical focal destruction of the medial proximal tibial metaphyses—is seen in about 50% of cases of congenital syphilis as well. Rubella classically leads to a “celery stalk” appearance with longitudinally arrayed linear striations extending from the epiphyses into the metaphyses. Other TORSCH infections may cause similar findings.
Rickets. Rickets is caused by vitamin D deficiency and leads to decreased mineralization of physeal cartilage. X-ray findings of physeal widening, loss of the zone of provisional calcification, metaphyseal fraying, and metaphyseal cupping are most evident at the fastest growing long bones (wrist and knee).
Scurvy. This lethal but treatable disease is caused by vitamin C deficiency. Radiographic findings include prominent zones of provisional calcification in the metaphyses (“white lines” of Frankel) with subjacent lines of demineralization (“scurvy lines”) and physeal widening.
Diagnosis
Osseous acute lymphocytic leukemia.
Pearls
Metaphyseal lucent bands are commonly seen with leukemia.
TORSCH infections may manifest metaphyseal lucency with a “celery-stalk” appearance.
Bony metastases are common in neuroblastoma and may show periosteal reaction, metaphyseal lucencies, lucent foci in other locations as well, and pathological fractures.
Suggested Readings
Blickman JG, van Die CE, de Rooy JW. Current imaging concepts in pediatric osteomyelitis. Eur Radiol. 2004; 14 Suppl 4:L55–L64 Mostoufi-Moab S, Halton J. Bone morbidity in childhood leukemia: epidemiology, mechanisms, diagnosis, and treatment. Curr Osteoporos Rep. 2014; 12(3):300–312 Ranson M. Imaging of pediatric musculoskeletal infection. Semin Musculoskelet Radiol. 2009; 13(3):277–299Case 101

Key Imaging Finding
Dense metaphyses.
Top Three Differential Diagnoses
Physiological dense metaphyses. In healthy young children age 2 to 6 years, increased metaphyseal density may be seen during periods of prolonged exposure to sunlight, especially common after winter. The exact mechanism is unknown, but this phenomenon may result from overproduction of endogenous vitamin D. Clues to diagnosis are that (1) at the knee the proximal end of the fibula appears normal, with no dense band, and (2) the dense band is no more dense than the diaphyseal or metaphyseal cortex.
Lead toxicity (plumbism). Lead toxicity is most common between ages 1 and 3 years. It results from inhalation of lead dust or ingestion of contaminated water or fragments of lead paint. When serum lead levels exceed 50 µg/dL, excess lead impairs osteoclast function, leading to failure of bone resorption in the zone of provisional calcification. Bilateral, symmetrical, dense metaphyseal bands develop—typically denser than the cortex of the adjacent metaphysis or diaphysis. Such a band at the proximal end of the fibula is useful for diagnosis, since density in this area does not increase even with physiological dense metaphyses. If high lead levels persist, growth deformity, such as Erlenmeyer flask deformity, may develop. Other heavy metals have a similar effect. Although radiological findings are suggestive, diagnosis rests on laboratory tests.
Treated leukemia. After treatment for leukemia, the metaphyses may appear dense. However, children with leukemia more often demonstrate lucent metaphyses.
Additional Differential Diagnoses
Healing rickets. Although patients with active rickets have frayed, flared, cupped metaphyses with widening of the physis, healing bone shows dense juxtaphyseal metaphyseal bands. This is most pronounced in the metaphyses or metaphyseal equivalents of rapidly growing bones: the wrists, knees, and anterior ribs.
Bisphosphonate therapy. Bisphosphonates treat patients with osteoporosis, usually due to osteogenesis imperfecta, steroid treatment, and neuromuscular disorders. These drugs increase bone density by inhibiting osteoclast-mediated bone resorption. Cyclical therapy leads to thin dense metaphyseal lines that parallel the physis in long bones (“zebra stripes”) and a “bone-within-bone” appearance of the spine and flat bones.
Syphilis. In utero infection with Treponema pallidum may lead to bone abnormalities that manifest during the first 2 months of life. A dense sclerotic band may be positioned between the physis and the abnormally lucent metaphysis. About 50% of patients demonstrate the Wimberger sign, focal osteolysis of the medial proximal tibial metaphysis. Pathological fractures and periosteal new bone formation may be present as well. Patients may have a rash, hepatosplenomegaly, anemia, ascites, and nephrotic syndrome.
Diagnosis
Lead toxicity.
Pearls
Physiological dense metaphyses appear no denser than adjacent cortex and spare the proximal fibula.
Although active rickets is characterized by wide, frayed metaphysis, during the treatment phase the metaphyses may appear dense.
If lead levels exceed 50 µg/dL, dense metaphyseal bands may develop.
Infants with syphilis may show a dense band between the physis and the abnormally lucent metaphysis.
Suggested Readings
Raber SA. The dense metaphyseal band sign. Radiology. 1999; 211(3):773–774 States LJ. Imaging of metabolic bone disease and marrow disorders in children. Radiol Clin North Am. 2001; 39(4):749–772Case 102

Key Imaging Finding
Periosteal thickening.
Top Three Differential Diagnoses
Physiological periostitis of infancy. In up to half of all infants between ages 1 and 6 months, rapid growth and relatively loose, thick periosteum may lead to periosteal thickening. Both the upper and lower extremities may be affected, and findings are typically symmetrical. The tibia is most commonly involved. Initially, a faint, amorphous line parallels the cortex; with time, the new bone thickens and becomes denser. This is eventually absorbed into the cortex, contributing to transverse bone growth. Unlike pathological periosteal thickening, physiological periostitis spares the metaphysis and is relatively thin (<2 mm).
Trauma. Periosteal new bone formation may manifest as early as 7 to 10 days after injury, becoming progressively denser and thicker until it is incorporated into adjacent bone, beginning about 2 months post injury. There may be no associated fracture in cases of stress reaction, or with nonaccidental trauma. Unlike physiological periostitis of infancy, periosteal new bone formation resulting from trauma may involve the metaphysis.
Infection. MRI may show periosteal elevation by day 2, and by about days 7 to 10 lamellar periosteal thickening may be radiographically evident. Chronic osteomyelitis may show thick, ossified periosteal reaction (“involucrum”).
Additional Differential Diagnoses
Neoplasm. Slow-growing tumors are often associated with solid periosteal reaction, whereas aggressive lesions classically show a lamellated, spiculated, or interrupted (Codman triangle) periosteal reaction.
Prostaglandin therapy. Children with cyanotic heart disease who are treated with prostaglandins may develop diffuse, symmetrical periosteal new bone formation as early as 6 days but more often 30 to 40 days from treatment onset. Remodeling eventually occurs.
Caffey disease (infantile cortical hyperostosis). This rare, self-limited disease usually affects infants younger than 5 months. Painful, often asymmetrical periosteal inflammation leads to lamellar periosteal thickening and eventual remodeling. The mandible is classically involved, but many bones may be affected.
Diagnosis
Periosteal thickening due to prostaglandin therapy.
Pearls
Physiological periostitis is typically symmetrical, measures less than 2 mm, and spares the metaphysis.
With nonaccidental trauma and stress reaction, periosteal new bone formation may be the only sign of injury.
The periosteal thickening in infants treated with prostaglandins is usually symmetrical, whereas with Caffey disease it is often asymmetrical.
Suggested Readings
Kwon DS, Spevak MR, Fletcher K, Kleinman PK. Physiologic subperiosteal new bone formation: prevalence, distribution, and thickness in neonates and infants. AJR Am J Roentgenol. 2002; 179(4):985–988 Poznanski AK, Fernbach SK, Berry TE. Bone changes from prostaglandin therapy. Skeletal Radiol. 1985; 14(1):20–25 Wenaden AE, Szyszko TA, Saifuddin A. Imaging of periosteal reactions associated with focal lesions of bone. Clin Radiol. 2005; 60(4):439–456Case 103

Key Imaging Finding
Cortical thickening.
Top Three Differential Diagnoses
Stress fracture. Children and adolescents are prone to stress (fatigue) fractures, which occur when normal bone is subjected to abnormal activity. The most common etiology of fatigue fractures is chronic and repetitive workload. The tibia and fibula are most often affected in children, but the femur, tarsals, and metatarsals may be involved. Radiographs are relatively insensitive and detect 15% of fractures in the acute setting. Manifestations vary with age and type of load. Tibial/fibular toddler fractures, associated with onset of ambulation, may show a slight linear lucency and, as they heal, periosteal reaction and eventual smooth cortical thickening, whereas tarsal fractures manifest as a band of sclerosis due to callus. MRI is more sensitive and specific and demonstrates marrow edema and a hypointense fracture line. Scintigraphy is sensitive but nonspecific.
Osteoid osteoma. Osteoid osteoma typically presents in patients under age 20 years, about twice as often in males. Classic presentation is pain at night, relieved by salicylates. These diaphyseal or metaphyseal lesions are typically eccentric. More than half of these lesions occur in the tibia or femur, with most others in the spine, hands, or feet. X-rays show a lucent nidus, typically less than 1 cm in diameter and surrounded by a rim of sclerosis. MRI shows the lesion, along with bone marrow and soft-tissue edema. The goal of treatment is removal or destruction of the nidus, performed surgically or by image-guided percutaneous thermoablation.
Chronic osteomyelitis. Chronic osteomyelitis is sometimes characterized by sequestra (necrotic bone in an area of inflammation) and involucra (periosteal new bone formation around dead bone). The radiographic appearance is of diffuse cortical thickening, sometimes with a lucent central lesion. One-third of cases occur in patients younger than 2 years, with a 2:1 male predominance. Over 75% of cases involve the long bones, especially the faster growing bones and metaphyses. MRI and scintigraphy may be helpful. Other findings that suggest infection include marrow edema, subperiosteal fluid, and a sinus tract, with relatively little soft-tissue involvement. Tissue biopsy is often necessary for confirmation.
Additional Differential Diagnosis
Osteoblastoma. Osteoblastoma is a rare, benign tumor that is most common in the flat bones or the vertebrae (posterior elements) and less common in the extremities. Though a distinct entity, it may mimic the appearance of a large osteoid osteoma (but osteoblastoma is larger). It may be blastic, lytic, or mixed, and well defined, exophytic, or aggressive. On histological analysis, there is osteoid and pure woven bone production, occasionally with focal osteoblastic rimming.
Diagnosis
Osteoid osteoma.
Pearls
Radiographs are relatively insensitive for stress fractures but may show subtle periosteal reaction.
Osteoid osteoma is an eccentrically located benign lesion with a lucent nidus surrounded by sclerosis.
MRI findings in chronic osteomyelitis may include sequestra and involucra, marrow edema, subperiosteal fluid, and a sinus tract, with relatively little involvement of surrounding soft tissues.
Osteoblastoma is a rare, benign tumor that may appear blastic, lytic, or mixed.
Suggested Readings
Blickman JG, van Die CE, de Rooy JW. Current imaging concepts in pediatric osteomyelitis. Eur Radiol. 2004; 14 Suppl 4:L55–L64 Jaimes C, Jimenez M, Shabshin N, Laor T, Jaramillo D. Taking the stress out of evaluating stress injuries in children. Radiographics. 2012; 32(2):537–555 Levine SM, Lambiase RE, Petchprapa CN. Cortical lesions of the tibia: characteristic appearances at conventional radiography. Radiographics. 2003; 23(1):157–177Case 104

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree