Part 1: Trauma
Case 1
Clinical History
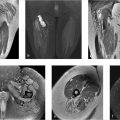
A 36-year-old male with shoulder pain after motor vehicle accident (Fig. 1‑1).

Key Finding
Shoulder dislocation.
Top 3 Differential Diagnoses
Anterior shoulder dislocation: A large majority of shoulder dislocations are anterior in direction, and typically occur with external rotation and abduction of the humerus. Complications include bony or soft tissue avulsion from the anterior inferior glenoid (Bankart lesion) and compression injury of the posterior humeral head (Hill–Sachs lesion). Greater tuberosity fracture is more common in older patients. Although diagnosis is usually apparent on frontal radiographs, an axillary view or transcapular “Y” view helps confirm the presence and direction of dislocation.
Posterior shoulder dislocation: Posterior dislocations are rare, accounting for less than 5% of shoulder dislocations. Many cases are initially missed on radiographs. Common causes are high-energy trauma with force on a shoulder in flexed, adducted, and internally rotated position, seizure, electrocution, and falls on an outstretched hand. The humeral head is locked in internal rotation, which is a sign noted both clinically and radiographically. An axillary view or transcapular “Y” will confirm presence. The compression deformity on the anteromedial humeral head is termed “reverse Hill–Sachs” lesion. Similarly, a posterior labral tear and posterior glenoid rim fracture are termed soft tissue and osseous “reverse Bankart” lesions, respectively.
Luxatio erecta: This is a rare form (less than 1%) of shoulder dislocation secondary to hyperabduction. The arm is characteristically locked in an elevated position, with the humeral head inferior to the glenoid on radiographs. This type of dislocation is frequently associated with neurovascular and musculoskeletal injuries, with rotator cuff tears and greater tuberosity fractures more prevalent than in the other types.
Additional Diagnostic Considerations
Pseudosubluxation/pseudodislocation: Inferior subluxation of the humeral head due to hemarthrosis or joint effusion may mimic posterior dislocation on AP view, but axillary or transcapular view shows no dislocation.
Rotator cuff tear: Superior subluxation of humeral head is seen with large chronic rotator cuff tears. No dislocation is apparent on axillary or transcapular views.
Diagnosis
Posterior shoulder dislocation.
Pearls
Axillary or transcapular view are essential in diagnosing shoulder dislocations.
Failure to see the joint articulation on a true AP (Grashey) view is a sign of dislocation.
Signs to look for on the AP view with posterior dislocation include the “lightbulb” appearance of the humeral head due to fixed internal rotation of the humerus, widened glenohumeral joint due to lateral displacement of the humeral head, and “trough” sign secondary to bony impaction.
Associated bony and soft tissue injuries are not well-evaluated on radiographs. CT and MRI are more sensitive for evaluation of bone and soft-tissue injuries.
Suggested Readings
- 1 Cicak N. Posterior dislocation of the shoulder.. J Bone Joint Surg Br 2004; 86 (3) 324-332 PubMed 15125117
- 2 Cutts S, Prempeh M, Drew S. Anterior shoulder dislocation.. Ann R Coll Surg Engl 2009; 91 (1) 2-7 PubMed 19126329
- 3 Hassanzadeh E, Chang CY, Huang AJ. CT and MRI manifestations of luxatio erectahumeri and a review of the literature.. Clin Imaging 2015; 39 (5) 876-879 PubMed 25979120
- 4 Kowalsky MS, Levine WN. Traumatic posterior glenohumeral dislocation: classification, pathoanatomy, diagnosis, and treatment.. Orthop Clin North Am 2008; 39 (4) 519-533, viii PubMed 18803981
Case 2
Clinical History
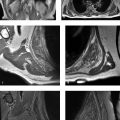
A 32-year-old female with shoulder pain (Fig. 2‑1).

Key Finding
Distal clavicular erosion.
Top 3 Differential Diagnoses
Trauma: Stress osteolysis of distal clavicle can occur when repeated forces are applied to the acromioclavicular (AC) joint. This is classically seen in weightlifters. Symptoms begin with aching pain in the AC region which are exacerbated by weight training (e.g., bench presses, push-ups, dips on the parallel bars, overhead activities, and horizontal adduction). The most accepted etiology is that repetitive microtrauma causes subchondral stress fractures and remodeling in the distal clavicle. Acromion is spared in this entity.
Rheumatoid arthritis (RA): Rheumatoid arthritis can cause distal clavicular resorption identical to other etiologies. Presence of other findings of inflammatory arthropathy including periarticular osteopenia, erosions of acromion, glenohumeral joint space narrowing, and erosions of the glenohumeral joint can help in pinpointing the diagnosis.
Hyperparathyroidism: Besides the distal clavicular erosion, another finding that can be seen in hyperparathyroidism on the shoulder or clavicular radiographs is subligamentous resorption at the site of coracoclavicular ligament on the clavicle. Generalized bone demineralization is a uniform feature of all types of hyperparathyroidism. Subchondral bone loss can also be seen at sacroiliac, sternoclavicular and temporomandibular joints, and at symphysis pubis, in addition to the AC joint.
Additional Diagnostic Considerations
Scleroderma: Scleroderma is a multisystem disease. Radiographically, acro-osteolysis and soft tissue calcifications are commonly seen. Erosions can occur but arthritis is not a prominent feature.
Infection: Septic arthritis should always be entertained as a possibility in distal clavicular erosion.
Diagnosis
Posttraumatic osteolysis.
Pearls
Posttraumatic distal clavicular osteolysis is most commonly associated with weight training involving upper extremities.
In RA, presence of other findings like periarticular osteopenia, glenohumeral joint space narrowing and erosions can help in narrowing the differential.
Hyperparathyroidism will also demonstrate other findings like generalized osteopenia, subligamentous, and subperiosteal resorption.
Suggested Readings
- 5 Currie JW, Davis KW, Lafita VS et al. Musculoskeletal mnemonics: differentiating features.. Curr Probl Diagn Radiol 2011; 40 (2) 45-71 PubMed 21266270
- 6 Manaster BJ, May DA, Disler DG. Musculoskeletal Imaging, The Requisites. 4th ed. Philadelphia: Mosby Elsevier; 2013
- 7 Schwarzkopf R, Ishak C, Elman M, Gelber J, Strauss DN, Jazrawi LM. Distal clavicular osteolysis: a review of the literature.. Bull NYU Hosp Jt Dis 2008; 66 (2) 94-101 PubMed 18537776
Case 3
Clinical History
A 32-year-old male with shoulder pain after 6-foot fall onto right shoulder (Fig. 3‑1).

Key Finding
Widening of acromioclavicular (AC) joint.
Top 3 Differential Diagnoses
Trauma: AC injuries are more common in men and are caused by contact sports, heavy overhead manual labor, and falls on outstretched hand. An AC interval greater than 6 to 7 mm or a difference in AC interval of greater than 2 to 3 mm between the two sides are considered pathologic. AC joint separation is categorized using the Rockwood classification. Type I involves sprain or partial tear of the AC ligaments. Radiographically, the AC joint is normal. In type II AC separation, the AC ligaments are completely torn, and coracoclavicular ligaments sprained. Radiographically, the AC joint is widened, and there may be mild elevation of the clavicle. Type III injuries show complete disruption of both AC and coracoclavicular ligaments. The clavicle is more significantly elevated and the coracoclavicular interspace is 25 to 100% increased. Type IV to VI occur in more severe injuries.
Distal clavicle erosion: Distal clavicle erosion can present as widening of the AC joint on radiographs. More common causes include posttraumatic osteolysis, rheumatoid arthritis, and hyperparathyroidism. With posttraumatic osteolysis, there is commonly a history of repetitive trauma such as weightlifting. Rheumatoid arthritis and hyperparathyroidism are systemic diseases, thus most often present bilaterally.
Postsurgical change: Distal clavicular resection or Mumford procedure can be performed as part of subacromial decompression. Subacromial decompression consists of enlarging the subacromial space with osseous burring or excision of the undersurface of acromion. Concomitant symptomatic AC joint arthrosis is treated with resection of the AC joint and up to 1 cm of distal clavicle. The AC joint thus appears widened, even up to 2.5 cm.
Diagnosis
Type III acromioclavicular separation.
Pearls
Less than 15% of shoulder girdle injuries involve injury to the AC joint.
The most common grading system for AC joint injuries used is the Rockwood classification system, which grades injury from type I to VI, with the most common being types I–III.
Simultaneous view of bilateral AC joints helps to distinguish pathologic widening from normal variation.
Stress views of the AC joints with 10 to 15 pounds of weight suspended from each forearm can reveal more severe injuries than originally apparent. They are especially helpful in distinguishing Type II from Type III injuries.
MRI can be used to assess injury of coracoclavicular ligaments and deltoid and trapezius tendon insertions; thus, it is helpful in more accurately grading injuries.
Suggested Readings
- 8 Alyas F, Curtis M, Speed C, Saifuddin A, Connell D. MR imaging appearances of acromioclavicular joint dislocation.. Radiographics 2008; 28 (2) 463-479, quiz 619 PubMed 18349451
- 9 Ha AS, Petscavage-Thomas JM, Tagoylo GH. Acromioclavicular joint: the other joint in the shoulder.. AJR Am J Roentgenol 2014; 202 (2) 375-385 PubMed 24450680
- 10 Macdonald PB, Lapointe P. Acromioclavicular and sternoclavicular joint injuries.. Orthop Clin North Am 2008; 39 (4) 535-545, viii PubMed 18803982
- 11 Melenevsky Y, Yablon CM, Ramappa A, Hochman MG. Clavicle and acromioclavicular joint injuries: a review of imaging, treatment, and complications.. Skeletal Radiol 2011; 40 (7) 831-842 PubMed 20526774
Case 4
Clinical History
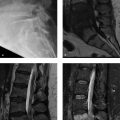
A 23-year-old male after fall on an outstretched arm (Fig. 4‑1).

Key Finding
Fracture dislocation of forearm.
Top 3 Differential Diagnoses
Galeazzi fracture: The Galeazzi fracture is a fracture through the distal radius (between the middle and distal thirds) with disruption of the distal radioulnar joint (DRUJ). With distal radial fractures, care must be taken to evaluate the distal radioulnar joint both clinically and radiographically. Thus, evaluation requires both forearm and wrist radiographs. Evidence of DRUJ disruption include widening of the DRUJ space, lack of overlap of the ulnar head on the distal radius on PA view, dislocation of the ulnar head relative to the radius on a true lateral view, or shortening of the distal radius by more than 5 mm. Treatment of this injury is almost always surgical.
Monteggia fracture: The Monteggia fracture is a fracture of the proximal third of the ulna with associated radial head dislocation. With proximal ulna fractures, attention should be paid to radiocapitellar joint alignment. A line drawn through the center of the proximal radius should intersect the capitellum on all the views. Injuries may involve the deep branch of the radial nerve (posterior interosseous nerve) which is intimately associated with the radial head at the elbow.
Essex–Lopresti fracture: This rare but often overlooked injury is the combination of a comminuted radial head fracture with disruption of the interosseous membrane, resultant dislocation of the distal radioulnar joint, and proximal migration of the distal radius. Because the dislocation at the DRUJ is often missed both clinically and radiographically, it is important to obtain dedicated wrist views with attention to this area. Failure to address these injuries will lead to poor outcome.
Additional Diagnostic Consideration
“Nightstick” fracture: This is an isolated fracture of the ulna with no joint or radius involvement. Unlike the fracture dislocations of the forearm, which typically occur with an axial load such as a fall on an outstretched hand, the nightstick fracture is caused by a direct blow, thus being an exception to the forearm “ring rule,” which states that injury to one part of the forearm should result in a second fracture or dislocation elsewhere.
Diagnosis
Monteggia fracture.
Pearls
Most forearm injuries from axial load follow the “ring rule,” that is, an injury of one bone or joint is often associated with fracture or dislocation in a second location. An exception to this rule is the “nightstick” fracture.
With a distal radius or comminuted radial head fracture, wrist radiographs should be obtained to evaluate the distal radioulnar joint.
With a fracture of the proximal ulna, elbow films should be obtained to evaluate radial head dislocation. A line drawn through the proximal radius can confirm a dislocation, as this should always intersect the capitellum of the humerus.
If a Galeazzi, Monteggia, or Essex–Lopresti fracture is missed, long-term disability and pain often result.
Suggested Readings
- 12 Bock GW, Cohen MS, Resnick D. Fracture-dislocation of the elbow with inferior radioulnar dislocation: a variant of the Essex-Lopresti injury.. Skeletal Radiol 1992; 21 (5) 315-317 PubMed 1502585
- 13 Gyftopoulos S, Chitkara M, Bencardino JT. Misses and errors in upper extremity trauma radiographs.. AJR Am J Roentgenol 2014; 203 (3) 477-491 PubMed 25148150
- 14 Perron AD, Hersh RE, Brady WJ, Keats TE. Orthopedic pitfalls in the ED: Galeazzi and Monteggia fracture-dislocation.. Am J Emerg Med 2001; 19 (3) 225-228 PubMed 11326352
Case 5
Clinical History
A 29-year-old male after fall on an outstretched hand (Fig. 5‑1).

Key Finding
Carpal dislocation.
Top 3 Differential Diagnoses
Perilunate dislocation: Perilunate injuries result from forced hyperextension of the wrist with ulnar deviation and carpal supination. They occur in a sequence of ligamentous disruptions termed “progressive perilunar instability,” which extends from a radial to ulnar direction. The perilunate dislocation is an intermediate stage in this sequence. On PA radiograph of the wrist, the lunate will appear triangular in shape, and a normal capitolunate articulation will not be visible. On lateral radiograph, the lunate articulates normally with the distal radius, but the capitate is dorsally dislocated.
Lunate dislocation: This injury occurs as the last stage of “progressive perilunar instability.” With increasing hyperextension force, a perilunate dislocation may become a lunate dislocation, as the dislocated capitate forces the lunate ventrally, disrupting its ligamentous attachment to the radius. Thus, the capitate becomes realigned with the distal radius, and the lunate is dislocated in a palmar direction. As with the perilunate dislocation, PA view of the wrist will show an abnormally shaped lunate, without a normal articulation between the lunate and capitate.
Midcarpal dislocation: The intermediate stage between perilunate and lunate dislocation, the midcarpal dislocation is a result of ligamentous injury at the lunotriquetral joint. The PA view of the wrist is similar to that of perilunate and lunate dislocations. However, lateral view of the wrist typically shows dorsal dislocation of the capitate, and volar tilt and subluxation of the lunate. Thus, neither the lunate nor the capitate is normally positioned in relation to the distal radius.
Additional Diagnostic Consideration
“SLAC” wrist: Scapholunate advanced collapse (SLAC) is a progressive form of wrist osteoarthritis most commonly secondary to trauma or calcium pyrophosphate dihydrate (CPPD) crystal deposition disease. Beginning with scapholunate dissociation, there is a progressive pattern of involvement with osteoarthritic changes initially occurring at the radioscaphoid joint and eventually affecting capitolunate joint with proximal migration of the capitate, causing more pronounced separation of the scapholunate interspace.
Diagnosis
Perilunate dislocation.
Pearls
Perilunate instability has been classified into four stages of ligamentous injury, starting at the scapholunate joint, progressing through the capitolunate and lunotriquetral joint (resulting in perilunate and midcarpal dislocation), with the final stage resulting in lunate dislocation.
Perilunate injuries may either be purely ligamentous (lesser arc injuries) or be associated with fractures (greater arc injuries), most commonly through the scaphoid (transscaphoid perilunate dislocation).
Review of the lateral wrist radiograph is essential in detecting and classifying these injuries.
Detection of perilunate injuries is important because early treatment can prevent the complications of chronic carpal instability and posttraumatic arthritis.
Suggested Readings
- 15 Grabow RJ, Catalano L, III . Carpal dislocations.. Hand Clin 2006; 22 (4) 485-500, abstract vi–vii PubMed 17097469
- 16 Kaewlai R, Avery LL, Asrani AV, Abujudeh HH, Sacknoff R, Novelline RA. Multidetector CT of carpal injuries: anatomy, fractures, and fracture-dislocations.. Radiographics 2008; 28 (6) 1771-1784 PubMed 18936035
- 17 Kennedy SA, Allan CH. In brief: Mayfield et al. Classification: carpal dislocations and progressive perilunar instability.. Clin Orthop Relat Res 2012; 470 (4) 1243-1245 PubMed 22322787
- 18 Scalcione LR, Gimber LH, Ho AM, Johnston SS, Sheppard JE, Taljanovic MS. Spectrum of carpal dislocations and fracture-dislocations: imaging and management.. AJR Am J Roentgenol 2014; 203 (3) 541-550 PubMed 25148156
Case 6

Key Finding
Avulsion fracture of finger.
Top 3 Differential Diagnoses
Terminal extensor tendon avulsion: The “mallet finger” is the most common closed tendon injury seen in sports, usually secondary to a direct blow (often baseball or basketball), which forcibly flexes an extended finger. This may result in a tendinous or bony avulsion of the extensor tendon. Clinically, the patient is unable to actively extend the distal interphalangeal (DIP) joint, and radiographs often show flexion of the DIP joint. If left untreated, the imbalance in extensor forces may lead to a swan neck deformity.
Volar plate avulsion: The volar plate, a fibrocartilaginous structure that reinforces the joint capsule, is present at the proximal interphalangeal (PIP) and metacarpophalangeal (MCP) joints. The term volar plate avulsion is used most commonly for PIP injuries, and is secondary to hyperextension, with avulsion of the volar plate from the base of the middle phalanx. Pure ligamentous or bony avulsions can occur, and injury may be associated with dorsal dislocation. Fracture involvement of greater than 40% of the articular surface is considered unstable.
Flexor digitorum profundus avulsion: Avulsion of the profundus tendon (“jersey finger”) is caused by forceful hyperextension of a flexed DIP joint, most commonly of the ring finger. Most avulsions are tendinous and invisible on radiographs, thus requiring US or MRI for definitive diagnosis. A bony fragment may avulse in some cases and be visualized radiographically.
Additional Diagnostic Considerations
Central slip rupture: Acute central slip ruptures occur most commonly with forced flexion of an extended PIP joint, with injury at or near the dorsal insertion on the base of the middle phalanx. Other mechanisms include blow to the dorsum of the middle phalanx, or volar dislocation of the PIP joint. Avulsion fractures are much less common than ligamentous injury. An unrecognized injury often results in a boutonniere deformity.
Collateral ligament avulsion: Collateral ligament injury is caused by forced ulnar or radial deviation, and it can occur at the MCP or any interphalangeal joint, most commonly the PIP joint. Radiography may show an avulsion fracture at the insertion. Treatment is based on size of fragment and stability.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree