Part 8: Metabolic Musculoskeletal Conditions
Case 105
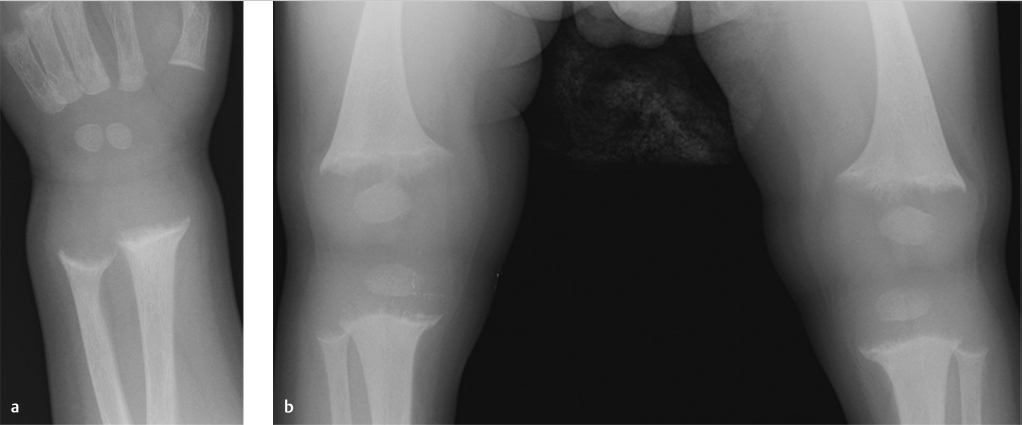
Key Finding
Frayed metaphyses.
Top 3 Differential Diagnoses
Rickets: Rickets is caused by deficiency of Vitamin D. It may be due to nutritional deficiency, malabsorption, anticonvulsant therapy, chronic liver disease, renal tubular insufficiency (Fanconi syndrome), or chronic renal disease. Vitamin D is essential for mineralization of osteoid. Failure of mineralization at growth plates leads to disorganized chondrocyte growth, and hypophosphatemia leads to impaired apoptosis of hypertrophic chondrocytes, which results in long cartilage cell columns and the radiographic findings of widening of growth plate and cupping and fraying of the metaphyses. Diaphyseal bowing, protrusio acetabuli, rachitic rosary (expansion of the anterior rib ends at costochondral junctions), and scoliosis can also be seen due to increased malleability of bones. Rachitic manifestations are most prominent at the sites of greatest growth, including the knee, distal tibia, proximal humerus, distal radius and ulna, and anterior ends of middle ribs.
Hypophosphatasia: In hypophosphatasia, a rare genetic disorder, there is decreased mineralization of bone caused by deficiency of tissue nonspecific alkaline phosphatase. The skeletal findings, including metaphyseal fraying, resemble those of rickets.
Stress: Excessive stress on growing physes and metaphyses can cause widening of the growth plate, sclerosis, and irregularity of metaphyses. This is seen in “gymnast wrists”—a chronic overuse injury seen in children who participate in gymnastics. Repetitive compressive forces can result in a chronic Salter–Harris 1 injury of distal radius.
Additional Diagnostic Considerations
Achondroplasia: Achondroplasia is an autosomal dominant rhizomelic dwarfism with several characteristic skeletal abnormalities like metaphyseal irregularity, short and bowed extremities, narrowing of interpediculate distances caudally in spine, cranial enlargement, and short broad ribs.
Metaphyseal chondrodysplasia: This is a group of disorders characterized by metaphyseal widening and flaring similar to rickets. Short stature, atlantoaxial instability, and platyspondyly are also commonly associated.
Diagnosis
Rickets.
Pearls
Rachitic manifestations are most prominent at the sites of greatest growth.
Skeletal findings of hypophosphatasia resemble those of rickets and osteomalacia.
“Gymnast wrists” present as physeal widening, metaphyseal irregularity, and sclerosis at wrists.
Suggested Readings
- 386 Chang CY, Rosenthal DI, Mitchell DM, Handa A, Kattapuram SV, Huang AJ. Imaging findings of metabolic bone disease.. Radiographics 2016; 36 (6) 1871-1887 PubMed 27726750
- 387 Glass RB, Norton KI, Mitre SA, Kang E. Pediatric ribs: a spectrum of abnormalities.. Radiographics 2002; 22 (1) 87-104 PubMed 11796901
Case 106

Key Finding
Generalized periosteal reaction.
Top 3 Differential Diagnoses
Hypertrophic osteoarthropathy (HOA): The secondary form of HOA is much more common than primary (pachydermoperiostosis). The majority of cases are associated with intrathoracic disease, most commonly malignancy, but extrathoracic causes include cirrhosis, biliary disease, and inflammatory bowel disease. The common clinical presentation is clubbing and bone and joint pain. Radiographs show symmetric, solid, or layered periostitis involving the diaphysis of long bones, with tibia, fibula, radius, and ulna being most commonly affected. Advanced cases can affect all tubular bones and extend to the metaphysis and epiphysis. The exact mechanism is unclear, but neurogenic and humoral pathways have been proposed.
Thyroid acropachy: Thyroid acropachy is a rare complication of autoimmune thyroid disease presenting with swelling of the hands and feet, clubbing of the digits, and often pretibial myxedema and exophthalmos. It can be seen after treatment of Grave’s disease, and patients may be euthyroid or hypothyroid. Radiographs show a characteristic spiculated, feathery or lacy periosteal reaction, usually bilateral and symmetric, and involving the tubular bones of hands and feet. Long bone involvement is rare.
Voriconazole-induced periostitis: This is a relatively recently described etiology of painful diffuse periostitis in posttransplant patients taking voriconazole, an antifungal medication, for prophylaxis or treatment of aspergillus infection. Radiographs show dense, focal, nodular, and irregular periostitis that can affect the tubular bones as well as clavicles, ribs, scapula, and pelvis. Symptoms resolve with discontinuation of the drug.
Additional Diagnostic Considerations
Pachydermoperiostosis (primary HOA): This is a rare hereditary disease that presents in a similar fashion to secondary HOA. Skin thickening of the forehead and scalp may be additional components.
Venous stasis: This is usually seen in the lower extremities, and may be associated with phleboliths, subcutaneous edema, and sometimes soft-tissue calcifications.
Hypervitaminosis A: Common causes include high-dose dietary supplements and long-term use of retinoids for acne or cancer. Cortical thickening and ligament and tendon calcification may be other features.
Diagnosis
Voriconazole-induced periostitis.
Pearls
Voriconazole-induced periostitis can be distinguished from HOA by more diffuse involvement (as opposed to predominantly long bone involvement), absence of clubbing, and elevated alkaline phosphatase. A clinical history of transplantation and voriconazole therapy is helpful.
Thyroid acropachy can be distinguished from HOA by less involvement of the long bones, and a spiculated, fluffy, or lacy appearance of periosteal proliferation.
The finding of generalized symmetric periostitis requires a search for underlying malignancy if other underlying causes are not recognized.
Suggested Readings
- 388 Chen L, Mulligan ME. Medication-induced periostitis in lung transplant patients: periostitis deformans revisited.. Skeletal Radiol 2011; 40 (2) 143-148 PubMed 20652242
- 389 Yap FY, Skalski MR, Patel DB et al. Hypertrophic osteoarthropathy: clinical and imaging features.. Radiographics 2017; 37 (1) 157-195 PubMed 27935768
Case 107

Key Finding
Periarticular calcified mass.
Top 3 Differential Diagnoses
Calcinosis of renal failure: The most frequent cause of periarticular calcified mass is chronic renal failure. This lesion is also called secondary tumoral calcinosis. There is no radiologic or histologic difference between these lesions and lesions of tumoral calcinosis. The diagnosis is made solely on clinical history, serum chemistry, and glomerular filtration rate. These calcium accumulations can be massive. Typically, other imaging features of renal osteodystrophy are present.
Tumoral calcinosis: Tumoral calcinosis is a familial condition characterized by single or multiple painless, calcified masses. The patients are usually of African descent. It has a characteristic radiographic appearance of an amorphous, cystic, multilobulated, calcified mass in a periarticular location. Extensor surfaces are usually affected. These masses most commonly occur around hip, shoulder, and elbow. Fluid–fluid levels may be seen due to layering of calcium on CT, commonly termed “sedimentation sign.”
Heterotopic ossification: Heterotopic ossification is usually due to injury, cerebrospinal disorder, or burns. In cases of spinal cord injury, it is most commonly seen around hips. It primarily occurs in muscles but may be seen around ligaments or joint capsules. Faint calcifications are seen initially which evolve into well-defined ossification after 6 weeks or more. Maturation of ossification proceeds centrifugally with more mature bone seen at the periphery surrounding less mature bone in the center. Late lesions look like mature bone.
Additional Diagnostic Considerations
Gout: Tophaceous gout may result from long-standing hyperuricemia. Calcified periarticular tophi are usually faintly radiopaque and commonly associated with underlying erosions of bone.
Synovial sarcoma: Synovial sarcoma is a malignant mesenchymal neoplasm, which may show calcifications in one third of cases. Two thirds of synovial sarcomas occur in lower extremities and can involve periarticular regions. Radiologic appearance of this tumor is variable but can show dense calcification involving only a portion of the tumor.
Diagnosis
Calcinosis of renal failure.
Pearls
Calcinosis of renal failure is radiologically similar to tumoral calcinosis.
Tumoral calcinosis has a characteristic amorphous, lobulated, calcific mass in a periarticular location.
Late lesions of heterotopic ossification look like mature bone with cortex and medullary space.
Suggested Readings
- 390 Manaster BJ, May DA, Disler DG. Musculoskeletal Imaging, The Requisites. 4th ed. Philadelphia: Mosby Elsevier; 2013
- 391 Olsen KM, Chew FS. Tumoral calcinosis: pearls, polemics, and alternative possibilities.. Radiographics 2006; 26 (3) 871-885 PubMed 16702460
Case 108

Key Finding
Long bone sclerosis.
Top 3 Differential Diagnoses
Fibrous dysplasia: Fibrous dysplasia is a benign, noninherited bone disease that is characterized by replacement of normal lamellar cancellous bone by abnormal fibrous tissue. It is categorized as monostotic or polyostotic and may occur as a component of McCune–Albright syndrome or the rare Mazabraud syndrome. Classically, the lesions are intramedullary, expansile, and well-defined. There may be endosteal scalloping but a smooth cortical contour is always maintained. Lesions show varying degrees of hazy density. Some lesions may appear completely radiolucent or sclerotic. Amongst the long bones, the most common sites of involvement include femur, tibia, and humerus.
Paget’s disease: Paget’s disease of the bone is a relatively common disorder that typically presents after 40 years of age. Classically, three phases have been described: lytic, mixed, and blastic. The blastic phase manifests as osseous sclerosis, resulting in coarse trabecular, cortical thickening and bone enlargement. Although Paget’s disease predominantly affects the axial skeleton, proximal long bones such as femur are frequently involved. Long bone involvement typically begins in a subchondral location.
Melorheostosis: Melorheostosis (Leri disease) is a sporadic sclerosing skeletal dysplasia that typically manifests in late childhood or early adulthood. Patients may present with pain and stiffness of involved bones. It has a characteristic radiographic appearance consisting of cortical and medullary hyperostosis of a single bone or multiple adjacent bones with a flowing “dripping candle wax” appearance. Lower extremities are more commonly affected than upper extremities.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree