Part 9: Spine
Case 113
Key Finding
Vertebral body fusion.
Top 3 Differential Diagnoses
Developmental: A derivative of the notochord, vertebral bodies form from the cells of the sclerotome and any deviation in the normal development results in congenital anomalies which can be in a variety of configurations, including hemivertebrae, resulting in scoliosis, block vertebrae, or congenital vertebral fusion. Block vertebra results from a failure of the segmentation process, can be complete or partial, and occurs in the cervical or lumbar spine.
Juvenile Inflammatory arthritis (JIA): JIA is a polyarticular arthritis which can involve the cervical spine, particularly at C2–C3 and C3–C4, resulting is ankylosis, as well as decreased height and width of the vertebral bodies secondary to early epiphyseal closure. Initial symptoms include cervical pain and torticollis, and loss of mobility and extension can be progressive secondary to cervical fusion.
Postoperative: Anterior cervical discectomy is approached from the front, with removal of the intervertebral disc and placement of bone graft or implant, and subsequent plate and screw fixation. Evaluation on radiographs should include instrument positioning and failure, including infection, which can appear as bony resorption, destruction surrounding the implant, and hardware fracture.
Additional Diagnostic Considerations
Klippel–Feil syndrome (KFS): Congenital malformation defined by segmentation anomalies at one or multiple levels of the cervical spine with associated fusion. Originally described as a clinical triad of a short neck, low posterior hairline, and restricted cervical motion, KFS is classified into three subtypes based on the level and extent of vertebral fusion. In KFS, the vertebral bodies are narrowed in the AP dimension and there can be associated scoliosis or Sprengel deformity, a deformity related to abnormal scapular positioning.
Postinfectious: Discitis and osteomyelitis of the spine can result in narrowing of the disc space and collapse of the adjacent vertebral bodies, resulting later in intervertebral body fusion. MRI findings of spodylodiscitis include increased T2 signal in the disc space and adjacent endplates, with corresponding T1-hypointensity, and associated enhancement.
Diagnosis
Klippel–Feil syndrome.
Pearl
A “waist” can be seen at the level of intervertebral disc between fused segments, in cases of congenital vertebral fusion/block vertebra; this is not seen in acquired vertebral fusion.
Suggested Readings
- 404 Cohen PA, Job-Deslandre CH, Lalande G, Adamsbaum C. Overview of the radiology of juvenile idiopathic arthritis (JIA).. Eur J Radiol 2000; 33 (2) 94-101 PubMed 10711510
- 405 Haque S, Bilal Shafi BB, Kaleem M. Imaging of torticollis in children.. Radiographics 2012; 32 (2) 557-571 PubMed 22411949
- 406 Young PM, Berquist TH, Bancroft LW, Peterson JJ. Complications of spinal instrumentation.. Radiographics 2007; 27 (3) 775-789 PubMed 17495292
Case 114

Key Finding
Odontoid fracture.
Top 3 Differential Diagnoses
Type 1: Based on the Anderson and D’Alonzo classification, Type 1 odontoid fractures are stable fractures involving the dens above the transverse ligament, where it is attached to C1, and are rare. The mechanism involves avulsion of the alar ligament with avulsion of the tip of the dens.
Type 2: Type 2 fractures are transverse fractures through the base of the dens and are the most common type of odontoid fractures. These fractures have a tendency for nonunion due to poor blood supply. Greater than 6 mm displacement is a risk factor for nonunion. This is also the most significant factor in determination for surgery. Treatment usually involves C1–C2 posterior fusion.
Type 3: Type 3 fractures are the second most common type of odontoid fractures and involve the body of the axis and occasionally the facets of C1–C2. These fractures are considered unstable and can be treated surgically or with halo immobilization.
Additional Diagnostic Considerations
Os odontoideum: Os odontoideum is a smooth, well-corticated, ossific density at the superior aspect of a hypoplastic dens, whose etiology has been debated to be congenital or traumatic. It can also be seen with a hypertrophied anterior arch of C1. Surgery is reserved for symptomatic or unstable cases.
Persistent ossiculum terminale: A small, smooth, well-corticated ossicle at the tip of the dens is a normal anatomic variant. It is due to the failure of fusion of the secondary ossification center of the dens, which is supposed to fuse around the age of 12.
Diagnosis
Type 2 odontoid fracture.
Pearls
Fractures are best seen on open-mouth, odontoid views on radiographs, and posterior displacement should be evaluated on lateral views.
Type 2 odontoid fractures are common in elderly secondary to falls; however, they are also seen in children secondary to blunt trauma due to large head to spine ratio.
In contrast to fractures, which are irregular and lucent, developmental variants and anomalies have smooth and well-corticated margins.
Suggested Reading
- 407 O’Brien Sr WT, Shen P, Lee P. The dens: normal development, developmental variants and anomalies, and traumatic injuries.. J Clin Imaging Sci 2015 (e-pub ahead of print); PubMed 10.4103/2156–7514.159565 26199787
Case 115

Key Finding
Hyperflexion injury.
Top 3 Differential Diagnoses
Bilateral facet dislocation: In an unstable injury associated with spinal cord injury, there is dislocation of the inferior articular facets over the lower vertebra’s superior articular facets anteriorly, with translation of the vertebral body as well. Findings are best seen on sagittal CT reconstructions, but axial views can also demonstrate a “reverse hamburger” sign. There is also associated disruption of the anterior and posterior longitudinal ligaments. Facets are considered subluxed if there is more than 2mm of diastasis, or there is less than 50% coverage of the articular surfaces.
Compression fracture: Also termed wedge fractures, these result from axial loading or can be secondary to insufficiency in osteoporotic patients. There is height loss involving the anterior vertebral body, with fracture of the superior endplate seen, as increased density secondary to impaction. This injury generally involves the mid to lower cervical spine.
Flexion teardrop fracture: The mechanism includes flexion and compression usually from motor vehicle accidents or diving, and this is an unstable injury associated with neurologic deficits and occasional paraplegia. There is a teardrop fracture fragment from the anterior inferior aspect of the vertebral body, widening of the interspinous processes, decreased height of the vertebral body, and posterior displacement of the vertebral body into the spinal canal.
Additional Diagnostic Considerations
Sprain: Soft-tissue injury without evidence of fracture is seen as edema within the posterior soft tissues. These findings are best demonstrated on STIR or fat-suppressed, T2-weighted sequences with abnormal signal in the posterior soft tissues. Occasionally, bone contusions in the form of edema within the vertebral bodies can also be seen.
Unilateral facet dislocation: In a hyperflexion injury with rotation, there is unilateral displacement of the inferior articular facet over the lower vertebra’s superior articular facet, which is also termed jumped or perched facet. Lateral views demonstrate a “bow-tie” sign of the locked facet and,often, there is widening of the interspinous distance.
Diagnosis
Unilateral facet dislocation.
Pearl
Consider CT angiography (CTA) in cases of unilateral (more common) and bilateral facet dislocations, as there is increased incidence of vertebral artery injury.
Suggested Readings
- 408 Dreizin D, Letzing M, Sliker CW et al. Multidetector CT of blunt cervical spine trauma in adults.. Radiographics 2014; 34 (7) 1842-1865 PubMed 25384284
- 409 Kim KS, Chen HH, Russell EJ, Rogers LF. Flexion teardrop fracture of the cervical spine: radiographic characteristics.. AJR Am J Roentgenol 1989; 152 (2) 319-326 PubMed 2783508
Case 116

Key Finding
Midline sacral lesion.
Top 3 Differential Diagnoses
Chordoma: This is the most common primary malignant sacral tumor. It is more common in males and occurs in the 4th to 7th decades of life. Chordomas arise from malignant degeneration of notochordal remnants and are most commonly found in the sacrococcygeal region and then in the clivus. They are lytic lesions with internal calcifications and soft-tissue component with low-T1 and increased T2 signal on MRI.
Metastasis: The most common causes include lung, breast, and kidney malignancies, which are generally lytic. Common blastic metastatic lesions include breast or prostate carcinoma. Adjacent spread to the sacrum can also be seen with bladder, rectal, or uterine cancers.
Myeloma: Myeloma is a malignant clonal neoplasm which results in overproduction of monoclonal immunoglobulins, and distribution of disease follows red marrow, including the vertebrae, ribs, skull, and pelvis. Plasmacytoma is a single myelomatous lesion with common sites of involvement including the vertebrae or pelvis. Radiographs demonstrate well-circumscribed lytic or “punched out” lucency.
Additional Diagnostic Considerations
Ewing sarcoma: It is a malignant aggressive bone tumor with bony destruction and moth-eaten or permeative pattern with associated soft-tissue component. It is seen in children and young adults. There is intermediate T1 and low-to-intermediate signal on T2-weighted images with diffuse or peripheral nodular contrast enhancement on MRI.
Giant cell tumor (GCT) of bone: The second most common primary sacral neoplasm after chordoma, GCTs are destructive, lytic, and expansile lesions which are generally eccentric in location, however, they can involve the entire sacrum as well as the sacroiliac joints. They are heterogeneous on T2- and T1-weighted images secondary to internal hemorrhage and necrosis and are very vascular lesions.
Diagnosis
Metastasis from breast cancer.
Pearls
If multiple lesions are seen within the spine in addition to the sacrum, top differentials include metastasis or multiple myeloma.
Chordomas lie in the midline, whether in sacrum or clivus, unlike chondrosarcomas, which tend to lie eccentrically.
Suggested Reading
- 410 Diel J, Ortiz O, Losada RA, Price DB, Hayt MW, Katz DS. The sacrum: pathologic spectrum, multimodality imaging, and subspecialty approach.. Radiographics 2001; 21 (1) 83-104 PubMed 11158646
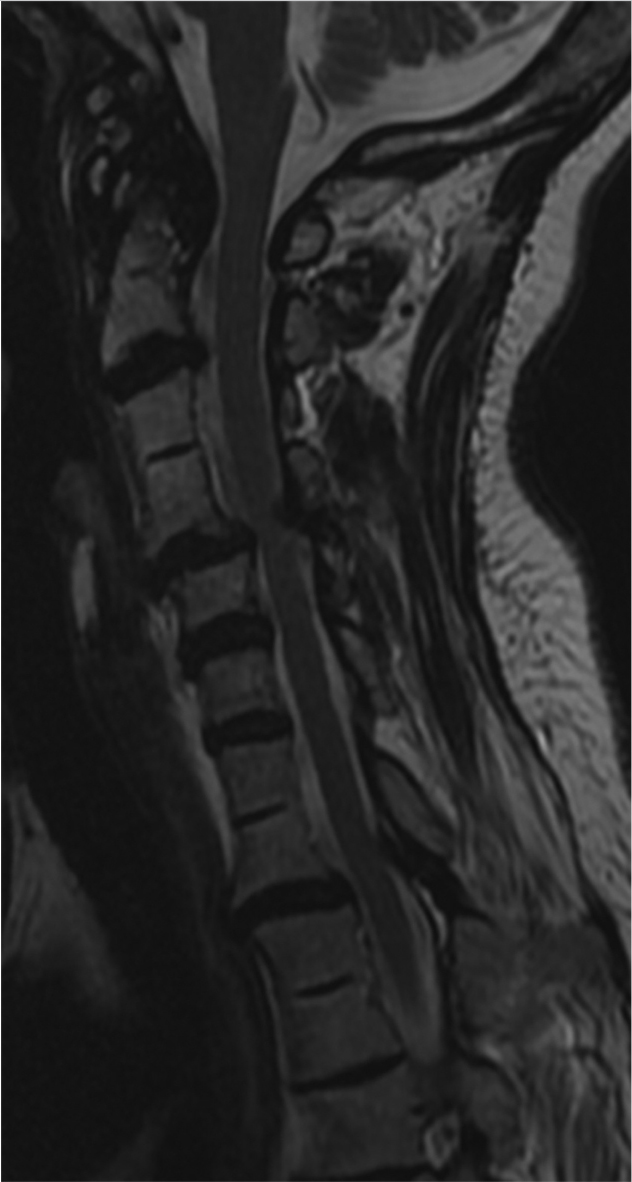
Case 117

Key Finding
Posterior vertebral body scalloping.
Top 3 Differential Diagnoses
Increased spinal pressure: Intraspinal masses, such as ependymoma, especially myxopapillary ependymoma, schwannoma, neurofibroma, lipoma, dermoid, and arachnoid cysts, can result in increased spinal pressure and exaggeration of the normal concavity or scalloping of the posterior wall of the vertebral bodies. Secondary findings of intraspinal masses can also include widening of the interpediculate distance. Cases of uncontrolled hydrocephalus have also been reported to result in posterior scalloping.
Dural ectasia: There are few inherited disorders which can exhibit dural ectasia such as neurofibromatosis (NF) type 1, Marfan’s syndrome, and Ehlers–Danlos syndrome. Dilatation of the thecal sac is postulated to be a result of pulsatile pressure of the cerebrospinal fluid on a defective dural wall, which mostly affects the lumbrosacral spinal region. Dural ectasia in NF-1 can also be secondary to neurofibromas or the presence of meningocele, most common in the thoracic spine.
Congenital disorders: Spinal findings in achondroplasia, a skeletal dysplasia resulting in dwarfism, include posterior vertebral scalloping, gibbus deformity, kyphosis, hypoplastic vertebral bodies, canal stenosis on the basis of shortened pedicles, as well as progressive decrease in interpedicular distance in the lumbar spine. Mucopolysaccharidoses such as Hurler and Morquio syndrome are also associated with dural ectasia.
Additional Diagnostic Consideration
Acromegaly: A feature sometimes seen in these patients, posterior scalloping, is thought to be the result of hypertrophy of soft tissue in the spinal canal and increased bone resorption.
Diagnosis
Dural ectasia from neurofibromatosis type 1.
Pearls
Presence of spinal manifestations including scoliosis, thoracic meningoceles, neurofibromas, and dural ectasia should suggest the diagnosis of NF-1.
Although hypoplastic vertebral bodies and dural ectasia are seen in both achondroplasia and mucopolysaccharidoses, there is no narrowing of the spinal canal in mucopolysaccharidoses.
Suggested Readings
- 411 Ho NC, Hadley DW, Jain PK, Francomano CA. Case 47: dural ectasia associated with Marfan syndrome.. Radiology 2002; 223 (3) 767-771 PubMed 12034948
- 412 Wakely SL. The posterior vertebral scalloping sign.. Radiology 2006; 239 (2) 607-609 PubMed 16641360
Case 118

Key Finding
Anterior vertebral body scalloping.
Top 3 Differential Diagnoses
Lymphadenopathy: Anterior scalloping of the vertebral bodies commonly results from mass lesions in the retroperitoneal space or mediastinum, with resorption of the bone secondary to pressure. Hodgkin’s lymphoma is a common cause of lymphadenopathy among patients between the ages of 20 to 40 years, and can result in anterior scalloping, with osteolytic and/or osteosclerotic (ivory vertebra) lesions. Adjacent paravertebral soft tissue and bony extension can also occur in Hodgkin’s lymphoma.
Tuberculous spondylitis: Also known as “Pott’s disease,” infection by tuberculosis affects the thoracolumbar spine. The extension of abscess beneath the anterior longitudinal ligament, or “subligamentous” spread, results in irregularity of the anterior margin of the vertebral body, preservation of the disc space, and paraspinal collections, in which calcifications are highly suggestive of tuberculosis (TB) infection. Progressive vertebral collapse can lead to anterior wedging, focal kyphosis, and gibbus deformity.
Aortic aneurysm: The pulsatile pressure in aortic aneurysms may result in erosion of the anterior vertebral bodies, which lie adjacent to the aorta. Imaging reveals focal dilatation of aorta. Calcifications from atheromatous disease may be present in the aortic wall.
Additional Diagnostic Considerations
Down syndrome: Other vertebral anomalies in Down syndrome include atlanto-axial and atlanto-occipital instability, scoliosis, spondylolisthesis, and squared or block vertebral bodies.
Diagnosis
Aortic aneurysm.
Pearls
In the evaluation of Pott’s disease, MRI should address the question of cord compression or epidural involvement. Postcontrast images can demonstrate subligamentous or dural enhancement.
In TB, disc space can be preserved until later stages of disease. Calcifications in paraspinal collections are highly suggestive of TB.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree