9 Pathology of the Neck
Pathology of the Suprahyoid Neck
Tonsillar Abscess
Differential Diagnosis
• Severe and acute Epstein–Barr infection.
• In unilateral cases: spread of infection from an odontogenic or parapharyngeal abscess.
• More likely without clinical signs of infection: asymmetric lymphoid hyperplasia, tonsillar retention cyst (fluid collection without capsular enhancement), lymphoma (e.g., non-Hodgkin), malignancies.
Points of Evaluation
• Lymphoproliferative growth of other lymph nodes in cases of systemic infection or lymphoma, infiltrative signs.
• Beware of airway obstruction and spread to parapharyngeal spaces, cavernous sinus (thrombosis), or cervical (pre)vertebral areas.
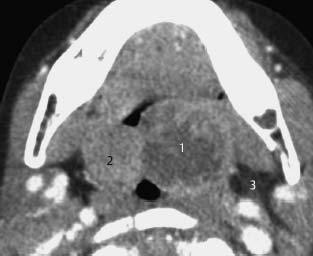
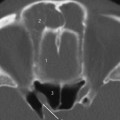
Fig.9.1 This 4-year old child had severe bilateral tonsillitis with symptoms of a left peritonsillar abscess.
CT with intravenous contrast enhancement, axial. The left tonsil (1) is much larger than the contralateral side (2) with central hypodensities suggestive of necrosis or fluid collections, confirming the presence of an abscess. The abscess is still limited to the tonsil, that is, there are no signs of peritonsillar spread.However, the parapharyngeal fat on the left side shows mildly increased density (3), indicative of edema and/or cellulitis. In this case, the tonsils were removed immediately because of airway obstruction.
Differential Diagnosis
Chronic infections with unilateral lymphadenitis (human immunodeficiency virus [HIV], syphilis, tuberculous tonsillitis, Plaut–Vincent), granulomatous diseases, aphthous diseases, parapharyngeal abscess, lymphoma.
Points of Evaluation
• Staging is based on enlarged or pathologic-appearing lymph nodes, bilaterality, and spread of tumor to the contralateral side.
• Because of the involvement of lymph nodes, infections might also be considered. However, the unilateral presentation excludes systemic infections.
• Lymphomas initially might present as unilateral lymphadenopathy.
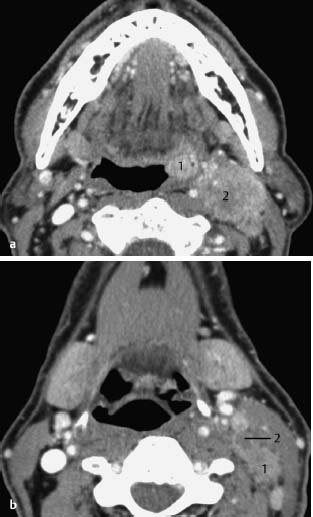
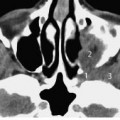
Fig.9.2 a, b Patient with complaint of pain in the oral cavity and left neck region.
a CT with intravenous contrast enhancement, axial. In the left tonsillar fossa, a small and enhancing tumor is visible (1), with enlarged level II lymph nodes (2) highly suggestive of metastasis. The internal jugular vein is not visible, probably due to the enlarged lymph nodes.
b CT with intravenous contrast enhancement, axial. Same patient as in Fig.9.2a, slice at a lower level, of the epiglottis.This area (i.e., level III) also shows enlarged lymph nodes (1), some with central necrosis (2).
Oropharyngeal Tumor, Base of Tongue
Differential Diagnosis
Benign and malignant tumors (squamous cell, salivary glands), lymphoma, granulomatous diseases (Wegener, sarcoidosis), infections (HIV, syphilis, tuberculous, Plaut–Vincent).
Points of Evaluation
• Staging by enlarged or pathological-appearing lymph nodes, bilaterality and spread of tumor to the contralateral side.
• Lymphomas (non-Hodgkin) initially may present as unilateral lymphadenopathy and ulcerative lesions.
• Evaluation of systemic disease and lymph nodes in other regions as well as secondary tumors in the hypopharynx and larynx.
• Keep in mind that (micro)metastases may be radiographically occult.

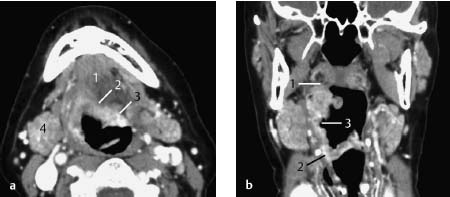
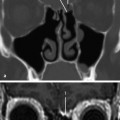
Fig.9.3 a–c Patient with globus sensation and some referred pain to the right ear.
a CT with intravenous contrast enhancement, axial. Axial slice at the level of the mandible and floor of the mouth (1). At clinical evaluation, an ulcer was found at the base of the tongue on the right side. The depth of this lesion (2) is quite well visualized on CT, with enhancement of the margins extending to the contralateral side (3) and the ipsilateral posterior side (4). This was staged as a T3N2c oropharyngeal tumor (enlarged lymph nodes not depicted).
b CT with intravenous contrast enhancement, coronal. The upper border (1) of the lesion, at the level of the soft palate, as well as the lower border (2) in the vallecula are clearly visualized, together with the ulcer at the center of the tumor (3).
c CT with intravenous contrast enhancement, sagittal. The sagittal view of the tongue shows the extent and depth of the lesion at the base of the tongue (1), its ulcerative surface (2), and infiltration into the vallecula (3). Whether the epiglottis (4) is affected remains unclear from this image. No infiltration of the pre-epiglottic space is present.
Multiple Synchronous Malignancies
Differential Diagnosis
Malignancies (squamous cell, salivary glands), diseases of the Waldeyer ring: lymphoma, granulomatous diseases (Wegener, sarcoidosis), infections (HIV, syphilis, tuberculous, Plaut–Vincent)
Points of Evaluation
• Staging is based on enlarged or pathologic-appearing lymph nodes, bilaterality, and spread of each tumor to the contralateral side.
• Lymphomas (non-Hodgkin) initially may present as unilateral lymphadenopathy and ulcerative lesions.
• Evaluation of systemic disease and lymph nodes in other regions.
• Keep in mind that (micro)metastases may be radiographically occult.
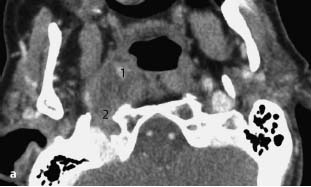
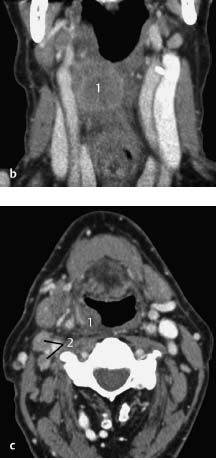
Fig.9.4 a–c Heavy smoker and alcohol abuse with complaints of a sore throat.
a CT with intravenous contrast enhancement, axial. A lesion with malignant characteristics is seen in the right tonsillar fossa (1). The internal jugular vein on the right side, often dominating the view, might be occluded by direct invasion or thrombosis (2). The carotid artery is compressed.
b CT with intravenous contrast enhancement, coronal. In the same patient, another tumor is also noted in the hypopharynx (1).Both the common carotid artery and internal jugular vein are patent at this level.
c CT with intravenous contrast enhancement, axial. The axial view through the hypopharyngeal lesion (1) shows multiple ipsilateral lymph nodes are enlarged, some of them with central necrosis (2) indicative of metastasis.
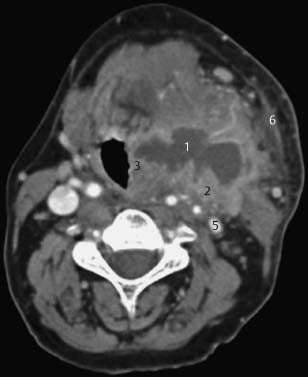
Fig.9.5 Patient having a cold and fever with a rapidly progressive red swelling of the neck and inspiratory stridor.
CT with intravenous contrast enhancement, axial. A large abscess (1) with a thick, contrast-enhanced capsule (2). The abscess is extending to the hypopharyngeal wall (3), with compression of the hypopharyngeal lumen, resulting in a severe inspiratory stridor. This slice is taken at the level of the base of the tongue (4). The left internal jugular vein (5) is much smaller than on the right side, probably due to partial compression by the abscess or physiologic asymmetry. The infiltration of the subcutaneous fat and thickened platysma on the left side (6) are suggestive of infection or edema.
Differential Diagnosis
Necrotizing lymph node metastases, lymphadenitis, mycobacterial infections, infected (epi)dermoid cyst or branchial cleft cyst, laryngocele (usually lower level).
Points of Evaluation
• The radiographic sign indicating involvement of the parapharyngeal spaces is the disappearance or compression of fat.
• Beside the important clinical features of infection, the hypodense contents of the lesion and its contrast-enhancing wall help in making the diagnosis of an abscess.
• Beware of the danger of airway obstruction and spread to the parapharyngeal spaces, the cavernous sinus (thrombosis), or the cervical (pre)vertebral areas.
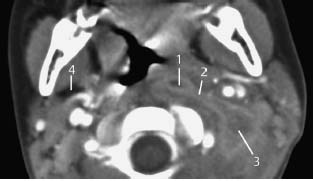
Fig.9.6 Patient with fever, trismus, and pain on swallowing.
CT with intravenous contrast enhancement, axial. Note the bulging left pharyngeal wall, as a result of a parapharyngeal abscess (1) which is spreading (2) to deeper structures in the neck (3). In contrast to the contralateral side, the fat in the parapharyngeal space is not visible on the affected side (4). A different window setting may better illustrate the enhancing wall of the abscess.
Differential Diagnosis
Reactive lymphadenopathy. Various primary infective agents: bacterial, viral, fungal, mycobacterial, toxoplasmosis, cat-scratch disease, syphilis. Neoplastic lymphoma. Sarcoidosis (sometimes with calcifications). Metastases with central necrosis.
Points of Evaluation
• Infected lymph nodes usually show homogeneous enhancement.
• Cavitation may indicate mycobacterial infections or necrotizing metastases.
• Beware of spread of infection outside the lymph nodes (parapharyngeal spaces, cavernous sinus thrombosis).
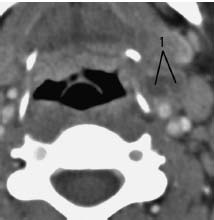
Fig.9.7 Patient with pyrexia of unknown origin and signs of infection in the neck.
CT with intravenous contrast enhancement, axial. Various enlarged level III lymph nodes are present near the internal carotid artery and jugular vein. Some of them show central necrosis (1), with slight rim enhancement. Although blood tests were indicative of bacterial infection no causative microorganism was isolated, and the patient was successfully treated with broad-spectrum antibiotics.
Differential Diagnosis
See Lymphadenitis.
Points of Evaluation
HIV infections may be associated with coexisting lymphoma and chronic lymphadenitis. Coexisting diseases may have a different clinical presentation in HIV.

Fig.9.8 Young male patient with episodes of fever and sweating during the night and enlarged cervical lymph nodes of unknown cause.
CT with intravenous contrast enhancement, coronal. Serology revealed HIV infection. On the right side, multiple homogeneously enhancing enlarged lymph nodes (1) are seen along the carotid artery and jugular vein (2), medial to the sternocleidomastoid muscle (3). On the left side, besides multiple solitary nodes, an enhancing conglomerate of lymph nodes (4) is observed.
Differential Diagnosis
• Other neoplastic lymphomas: Hodgkin disease, chronic lymphatic leukemia.
• For non-neoplastic causes, see “Lymphadenitis Colli”, page 288.
Points of Evaluation
Look for non-Hodgkin disease in extralymphatic sites such as the nasopharynx and tonsils. Hodgkin disease tends to be localized. On CT and MRI, non-Hodgkin disease usually presents as enlarged lymph nodes with homogeneous contrast enhancement. Central necrosis is typically associated with a higher likelihood of malignancy.
a CT with intravenous contrast enhancement, axial. On this slice, an area of different structure with enhancement is seen at the base of the tonsillar fossa (1). A conglomerate of deep cervical lymph nodes (2) demonstrating non-homogeneous enhancement and central hypodensities are seen at level II, medial to the sternocleidomastoid muscle (3).
b PET, axial. The positron emission tomography (PET) scan shows enhanced uptake at both locations as seen on the CT. No further hot spots are present. A biopsy confirmed non-Hodgkin B-cell lymphoma of the right tonsil.
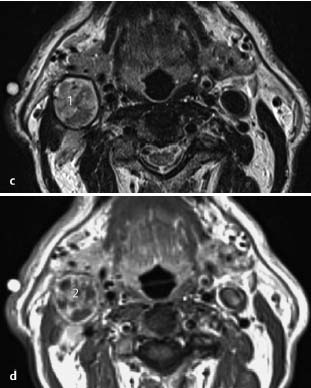
c,d MRI, T2-weighted (c) and T1-weighted with gadolinium enhancement (d), axial. At a lower level, the level II lymph node has a nonhomogeneous appearance on the T2-weighted image (1), which is confirmed by heterogeneous uptake of contrast (2).The capsule of the lymph node is intact (i.e., there are no signs of extracapsular spread). Histopathologic evaluation revealed a non-Hodgkin lesion.
Differential Diagnosis
Glomus vagale, jugulotympanic paraganglioma, hemangiopericytoma, salivary gland tumors, schwannoma, or neurofibroma (very rare). Less likely due to their hypodense nonenhancing contents: branchial cleft cysts, lymphangioma, dermoid cysts, lipoma.
Points of Evaluation
• Glomus vagale may be accompanied by displacement of the internal and external carotid arteries, however, it is not localized to the carotid bifurcation but rather to the parapharyngeal spaces in most cases. Dysfunction of cranial nerves IX, X, and XI may be associated with this pathology, especially in cases of jugulotympanic paraganglioma, which primarily occurs in the region of the jugular foramen and also can be associated with tinnitus.
• Tumor may be present in multiple locations in (familial) paraganglioma as well as in neurofibromatosis.
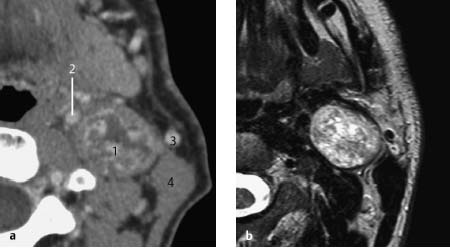
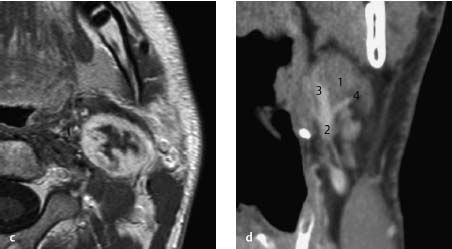
Fig.9.10 a–d Patient with a slowly progressive lesion in the neck.
a–c CT with intravenous contrast enhancement, axial (a), MRI, T2-weighted, axial (b), and T1-weighted, axial (c). Slices through the left side of the neck at the level of the lower border of the mandible. A smooth-bordered, rounded lesion (1) with a heterogeneous appearance (salt-and-pepper) is visible. On T2-weighted images the tumor displays mixed signal intensities. The enhancing parts have signal intensities equivalent to muscle, while the more cystic, nonenhancing areas demonstrate high signal intensities. There is strong heterogeneous enhancement both on CT and on MRI. The tumor is situated between the internal and external carotid arteries, a characteristic location. The internal jugular vein is not visible, probably due to compression. Also seen are the internal carotid artery (2), facial vessel (3), and the sternocleidomastoid (4).
d CT with intravenous contrast enhancement, coronal. The coronal view shows the lesion (1) located at the bifurcation of the common carotid artery (2). Note also the internal (3) and external (4) carotid arteries. This is a classic picture of a carotid body paraganglioma.
Differential Diagnosis
Laryngocele, cystic hygroma (septations), lymphoma or metastases with central necrosis (frequently multiple nodes), and dermoid cyst (fat content). Diagnoses less likely due to the appearance of the lesion in Fig.9.11 are abscess (surrounding infiltration), hemangioma or paraganglioma, and lipoma.
Points of Evaluation
• If present, the internal opening of the cleft cyst is situated in the tonsillar fossa (second branchial cleft) or in the superior part of the piriform sinus (third branchial cleft).
• Other possible differential diagnoses may need to be considered depending on the presence of septal structures inside the lesion, presence of a thickened and irregular capsule with signs of surrounding infiltration, and the density of the content.
• Papillary thyroid carcinoma has a propensity for cystic-appearing lymph node metastases. When single, such a node may present as a branchial cleft cyst.

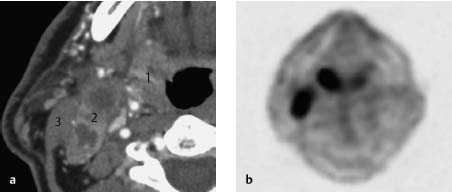
Fig.9.11 a, b Patient with a periodically fluctuating swelling of the right neck without further complaints.
CT with intravenous contrast enhancement, coronal (a) and axial (b).
Note the hypodense, cystic, smooth-bordered structure (1) with an enhancing capsule (2) that is thickened, probably due to lymphocytic infiltration or infections in the past. This location is typical for a branchial cleft cyst. In general, it is situated behind the submandibular gland (3), lateral to the jugular vein (4) and external carotid artery (5), and in front of the sternocleidomastoid (6), where the fistula, if present, frequently opens.
Differential Diagnosis
• In mild cases the lesion might be discovered as an incidental finding on radiology. In these cases other diagnoses are possible: branchial cleft cyst, laryngocele, salivary gland disorders (sialadenitis).
Less likely and depending on the appearance of the lesion and its content are: small abscesses, necrotizing lymph node metastases, lymphadenitis, neoplastic lymphoma, mycobacterial infections, hemangioma, paraganglioma, schwannoma, dermoid cyst, lipoma
Points of Evaluation
• Signs of previous infections, compression of vital structures and risk of airway obstruction, vascular compromise or neurologic deficits.
• In neonates, lymphangioma might grow rapidly and extensively, resulting in considerable deformities.
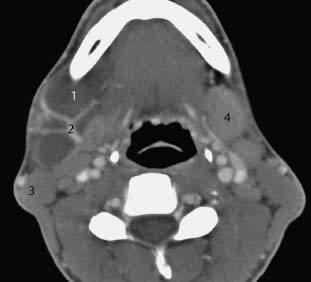
Fig.9.12 Patient with stable swellings of the neck, without any medical complaints but with some aesthetic deformity.
CT with intravenous contrast enhancement, axial. There is hypodense multilobular cystic structure (1) at the level of the mandible with medial displacement of the submandibular gland. Internal enhancing septations (2) are present in the lesion, which has no clear surrounding capsule. In this case, the sternocleidomastoid (3) is situated posterior to the lesion. Contralateral submandibular gland (4)
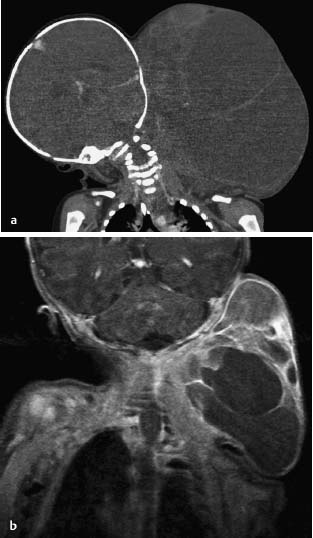
Fig.9.13 a, b Neonate with an extensive cystic hygroma of the head and neck.
a CT with intravenous contrast enhancement, coronal. During the first weeks, the lesion enlarged rapidly and, due to compression of the trachea, a tracheostomy was necessary.
b MRI, T1-weighted with gadolinium enhancement, coronal. Note the heterogeneous contents of the lesion in the left neck and its enhancing septations. The largest part of the lesion is not enhanced due to the predominant fluid content. Ultrasound can be useful for initial evaluation of such lesions.
Pathology of the Infrahyoid Region of the Neck
Supraglottic and Pharyngeal Tumors
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree