1.
Introduction to facility
Date:
Initial:
a. Physical layout
b. Supply areas
c. Location of offices
d. Location of hospital and unit manuals
e. Medication stock and narcotics
f. ECG, crash cart, respiratory supplies
2.
Flow of patients: introduction to areas
a. Admitting area
b. Minor surgery suite: frame placement
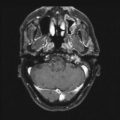
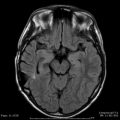
c. Radiology: MRI, CT, angiography suite
d. Gamma Knife: waiting area, treatment room, family waiting
e. Transfer to recovery suite
f. Discharge
3.
Introduction to interdisciplinary staff
a. Physicians: neurosurgeons, radiation oncologist, physicist, medical director
b. Gamma Knife secretary
c. Radiology technicians and scheduling assistant
d. Neurosurgery anesthesiologist for pediatric cases
4.
Equipment
a. G-frame, tray, and contents
b. Emergency equipment
c. Gamma Knife couch, video and audio monitoring
d. Physiologic monitoring
e. Fiducial indicators: MRI, CT, angiography, instructions for use
f. Filling of indicators
g. Assisting with “skull measurement”
5.
Charting
a. Admission note
b. Special Procedure Nurses Note
c. Time-out signatures
d. Physician orders
e. Patient treatment log
f. Discharge documentation
g. Patient teaching: pre-and post-procedure
6.
Policies, protocols, and procedures
a. Unit safety manual
b. Credentialing manual
c. Nursing procedure/policy manual (i.e., conscious sedation policy)
d. Radiation dosimetry badges and monthly reports
e. Routine patient care: adult
f. Patient care: pediatric
g. Radiation emergency procedures
7.
Manage patient flow-through procedure
a. Readies necessary equipment in treatment and prep room
b. Greets patient, preps for procedure
c. Assist with frame placement
d. Assist with radiology procedures
e. Assist with skull measurements
f. Reunite family with patient
g. Provide ongoing education as well as post-procedure instructions
h. Administer medications (pre-procedure such as steroid, anticonvulsant, pain)
i. Assist with positioning during treatment
j. Monitor vital signs, chart treatment records in appropriate book
k. Assist with frame removal, apply dressings
l. Ready chart and transport patient to recovery
m. Clean, reassemble, and store G-frame, ready fixations pins for sterilization
n. Complete discharge instructions
Date and initial each item after completion during orientation
Quality Assurance
Every radiosurgery center needs a quality assurance program in place. All patients should be interviewed after treatment, possibly during a follow-up phone call from the nurse. Questions regarding patient satisfaction and outcome expectations are essential. Quarterly meetings involving the entire professional staff should be held to discuss the results of the patient interviews. Patient satisfaction goals can be set and constant reevaluation conducted to ensure quality improvement.
Meetings can also be utilized to discuss any additions or changes to current protocol. Radiation safety classes and review of emergency patient procedures for all existing and new staff can be conducted in this medium. Documentation of minutes and attendance will ensure all staff have been properly included in the quality assurance process.
The Patient Flow Process
Intake
Patients will enter the radiosurgery program either by physician or self-referral. In the age of the Internet, more individuals are educating themselves about healthcare options in the comfort of their own homes in front of computers. Eventually, a phone call will be made to set up consultation appointments.
All the usual information regarding the patient’s demographic data is collected at this time. Referring and primary care physician information is gathered as well. Past hospitalizations and locations of treatment records, particularly pertaining to the diagnosis that is relevant to the radiosurgery treatment, should be gathered. Radiographic imaging such as MRI, CT, and angiography prints as well as reports is an absolute must for the consultation process. A preprinted comprehensive intake form will ensure consistent data collection. A follow-up letter should be sent to each patient after this phone call. The letter should contain directions, appointment dates and times, and concise instructions on what materials the individual is responsible for bringing to the appointment.
Many patients are eager to ask questions about radiosurgery and what it entails during this initial intake call. It is never too early to begin the education process. Having a clinical person available to begin dialogue at the time of intake is invaluable. Inappropriate referrals can be redirected at this time as well. The RN is an excellent resource for this role. The earlier the involvement of the nursing staff, particularly the staff who will be present at the time of treatment, the better the patient satisfaction and outcome with the entire experience.
Preprocedure Consultation
At the time of initial intake, the patient will be given appointment(s) with all the team members necessary to properly evaluate the appropriateness of radiosurgery. This may include consultations with neurosurgery, radiation-oncology, neuroradiology, medical oncology, and nursing. In that most patients who need to travel a distance and also rely on others for transportation attempt to combine as many appointments as possible into one visit. The neurosurgery-oncology multidisciplinary clinic is ideal for this type of referral. Prior to rendering a definite treatment plan, the patient’s case should be presented at a weekly neurosurgery-oncology team conference for final approval.
It is imperative that the patient records are gathered prior to the appointment so as to expedite the scheduling of the appropriate treatments. After consulting with the appropriate medical personnel, the patient should meet with a representative of the nursing staff. Viewing of a patient education video, tours of the radiosurgery facility, and the answering of questions can all help to ease anxiety. Appropriate consent forms should be obtained at this time as well. The patient should leave at the end of this consultation period with a firm treatment plan in place.
Preauthorization and Collection of Preoperative Data
The preauthorization process should be started when the patient makes the decision and is scheduled for the radiosurgery treatment. Designated personnel from the treating institution contacts the patient’s insurance company. Information to have handy at the time of contact may include:
Diagnosis
Procedure code
Outpatient versus inpatient visit
Date of procedure
Referring physician consultation note
Number of lesions to be treated
List of treatments that have been completed related to the diagnosis
Allow several days for preauthorization to be finalized.
Each institution has a policy regarding what preoperative evaluations are required prior to procedures. The following list should be considered as a guide regarding data collection and chart completeness:
Preauthorization obtained from insurance company
Preoperative check list completed by RN (Table 67.2)
Table 67.2
Preoperative nursing check list
• Review patient allergy history
• Assess any contraindication to imaging studies (contrast allergies, MRI metal concerns)
• NPO status
• Review of appropriate medications patient is to take prior to procedure
• What to bring to hospital (music, appropriate clothing, snack, medications)
• Assess anxiety level (help plan for proper sedation)
• Describe flow of the procedure and when and where family members will be allowed to wait and visit
• Review post-procedure course
History and physical complete
Anesthesia consult (select patient’s receiving deep or general anesthesia)
ECG
Serum results (electrolytes, complete blood count, coagulation)
Pregnancy testing on women of child-bearing age
Anticonvulsant serum levels (Dilantin, Tegretol, phenobarbital, etc.)
All consents complete (including angiography, MRI, CT, etc.)
Acquisition of imaging and reports necessary for localization
Completing the above list will minimize the risk of postponement, cancellation, or a negative outcome on the day of the procedure.
Patient Arrival and Preparation
The majority of radiosurgery centers require individuals to arrive early on the morning of the procedure. Patient registration should be complete prior to arrival to minimize any added anxiety. Patients should first change into comfortable clothing as outlined in pre-procedure instructions. Intravenous access is obtained, as well as any last-minute blood work. Diabetic patients should be checked for baseline serum glucose to determine any intervention. Vital signs are obtained, and a baseline neurologic assessment is completed by nursing staff. Medications taken in the past 12 h are reviewed, and a final check of consent forms occurs.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree