Fig. 6.1
Example of an information sheet that is sent out to the patient prior to the examination. Patients are asked to inform us in case contraindications to coronary CT angiography might be present that have been overlooked during the prior referral procedure (Chap. 5)
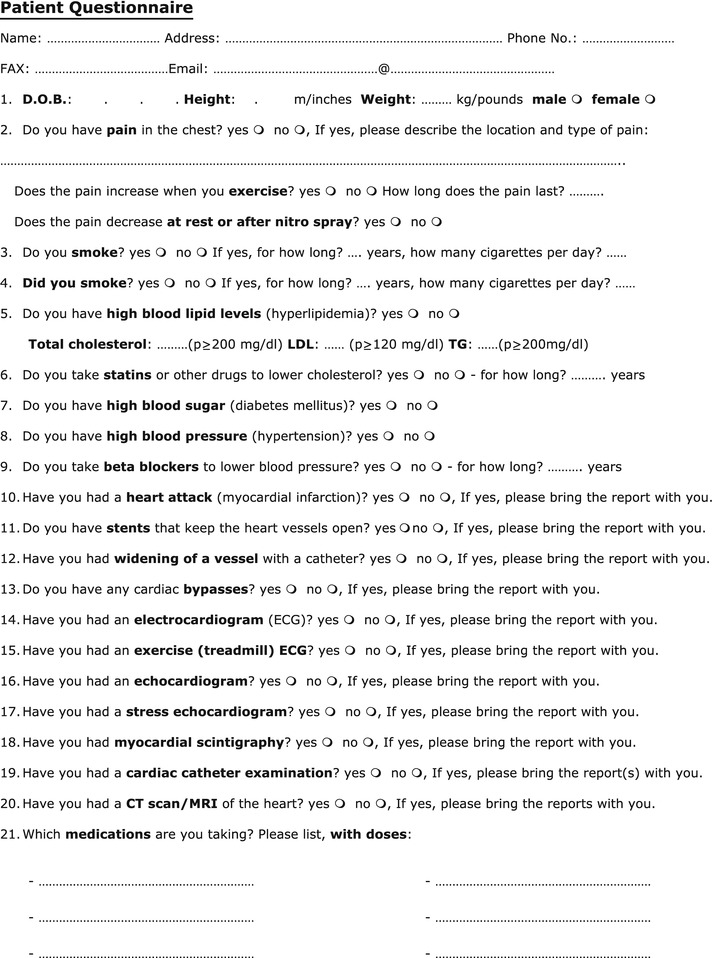
Fig. 6.2
Example of a medical history questionnaire that is also sent out to the patient prior to the examination. This questionnaire elicits information about the patient’s entire cardiovascular medical history and is very valuable for diagnostic procedures in the outpatient setting
6.2 General Information
The patient should be assured that CT is a noninvasive diagnostic procedure and that it does not take long to perform the examination. The short duration of the CT examination (about 15 min in the scanner room) and the comfortably wide and short gantry (in contrast to the narrow, claustrophobia-inducing bore in MRI) are major advantages of CT over MRI and should be stressed while talking to the patient. On the one hand, clearly explaining these aspects before the patient enters the scanner room reduces psychological stress and may relax the patient as well as reduce heart rate in some cases. On the other hand, the patient must also be given explicit information about the radiation exposure, which is the most important disadvantage of cardiac CT. As it does not mean much to a layperson that the effective exposure of a typical retrospectively gated exam is approximately 10–20 mSv, meaningful comparisons should be used, such as “the radiation exposure of cardiac CT angiography is five to ten times the annual background radiation” or “the effective radiation dose is the same as that of 100–200 chest X-rays.” Using prospective gating (“step-and-shoot”) will dramatically reduce the effective dose of cardiac CT to below 5 mSv in nearly all patients with low and stable heart rates (Chap. 7). Such effective doses are lower than necessary for nuclear myocardial perfusion imaging (about 8–12 mSv) and conventional coronary angiography (about 8 mSv). Thus, in patients with low and stable heart rates, the radiation exposure of CT is lower than that of alternative diagnostic tests. Nevertheless, especially in younger patients with a higher lifetime risk of cancer induced by CT, it is essential to carefully consider alternative imaging tests that might yield the same clinical information without radiation exposure.
Patients should know that lower heart rates (<60 beats per min) are associated with longer cardiac rest periods and thus improve image quality and diagnostic accuracy while they also help to reduce radiation dose. Informing them about the entire procedure prevents inadvertent reactions to unexpected events that might increase their heart rate. Hence, patients should be informed that they might experience a sensation of warmth when the contrast medium is injected and should also be told beforehand about the expected duration and number of breath-hold periods. Patients who are aware that the target structures are just a few millimeters in size will better understand that any motion during the breath-hold periods may severely degrade the images and may even result in a nondiagnostic scan. They also need to be informed that they should hold their breath after submaximal inspiration (ca. 75% of maximum inspiration), a maneuver that should be taught either prior to the examination or during scanning as part of the training related to the breath-hold commands (Chap. 8). The submaximum depth of inspiration is important, because maximal inspiration may increase intrathoracic pressure (Valsalva maneuver) and reduce inflow of the contrast medium.
The length of the breath-hold periods varies between 3 and 30 s, depending on the scanner used and the examination performed (Chap. 2). Breath-hold training on the scanner table is therefore also important to determine whether a patient is able to hold his or her breath for the required duration, or whether oxygen administration is needed to improve compliance. Preoxygenation is rarely required when the examination is performed on a 64-row CT scanner, with scan times of only 8–12 s. Using wide-volume scanning (320-rows) or fast prospective spiral acquisitions with second-generation dual-source CT, the scanning time is greatly reduced to just a single heart beat and breath-hold time is about 3–5 s (Chap. 2).
6.3 Contraindications
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree