II
Clinical Basics
Proper patient preparation prior to and during the positron emission tomography (PET) study is important to ensure maximum diagnostic yield. The most important factors are glucose level, minimizing the effects of physiologic activity, and timing the performance of a scan relative to the type of treatment.
Acceptable glucose levels for oncologic PET can be achieved by keeping the patient NPO (nothing by mouth) for a time before the study (see Diet subsection). Diabetic patients may require insulin or other drugs to control their blood glucose levels.
- Acceptable glucose levels. High glucose levels can compete with fluorodeoxyglucose (FDG) uptake and can substantially degrade image quality and the accuracy of the results.
- Glucose level should be ≤ 150 mg/dL if possible for optimal image quality.
- PET usually should not be performed if glucose is above 200 mg/dL.
- Diabetic patients. If needed, the physician managing the patient should be consulted for lowering blood glucose levels.
- Type I diabetes: Scan in morning after overnight fast.
- Type II diabetes: May require insulin in the morning.
- Insulin administration. Insulin (2 to 5 units) can be given if glucose is elevated. Glucose should be rechecked prior to FDG injection.
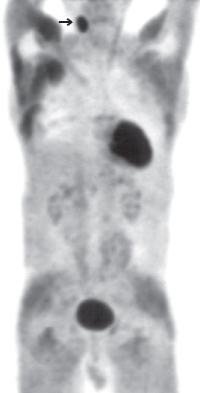
- Insulin administration will increase FDG uptake in the heart, skeletal muscles, and liver (the same pattern is seen if the patient has eaten before FDG administration). This will degrade image quality and therefore the ability to detect lesions (Fig. 4.1).
- A minimum time interval of 1 hour is necessary between insulin administration and FDG injection to minimize undesirable effects.1
- Other diabetic medications. Because the mode of action of metformin is a reduction of hepatic gluconeogenesis, this medication should not interfere with FDG up take. Other oral antidiabetic drugs, such as sulfonyl-ureas (tolbutamide, glyburide, glipizide), lower plasma glucose primarily by stimulating insulin secretion, and it makes sense to stop them before an FDG PET study. Insulin sensitizers, such as rosiglitazone, may not affect FDG uptake because their mode of action is primarily activation of peroxisome proliferator-activated receptors.
- The patient should be fasting for at least 4 hours prior to the exam.
- If there is known or suspected thoracic pathology, fasting for at least 12 hours is desirable to minimize cardiac activity.
- A low carbohydrate/high protein/high fat diet prior to the exam can optimize uptake and decrease myocardial uptake. This diet should be followed for at least 24 hours before the exam.
- Caffeine, nicotine, and alcohol should be avoided for 24 hours before the exam.
- Caffeine can have a variable effect on cardiac uptake; it can increase uptake or stimulate myocardial fatty acid metabolism and decrease FDG uptake.2
- Oral hydration. Oral hydration starting the day before the scan and continued hydration after the scan is recommended.3 Along with frequent voiding, this reduces bladder radiation dose and possibly improves image quality by reducing urinary artifact.
- Intravenous hydration. Intravenous hydration is useful but less frequently employed. If intravenous hydration is used, the fluid should not contain dextrose or lactose.
Physiologic uptake in muscle, brown fat, the urinary tract, and bowel can obscure or mimic disease.
- Muscle uptake
- The patient should avoid strenuous exercise the day of the study.
- Muscle relaxants such as diazepam are helpful in reducing muscle uptake from stress. Note that diazepam may be helpful in reducing brown fat uptake as well.
- Pretreatment with diazepam should be considered for all patients with suspicion of cervical and supraclavicular nodal disease because muscular uptake is most common in these regions.
- Laryngeal muscle uptake can be minimized by instructing the patient not to talk 5 minutes before and 20 minutes after the injection.
- Brown fat uptake (see Chapter 6). Brown fat uptake can be limited by decreasing adrenergic stimulation. This can be achieved by pharmacologic intervention and/or limiting patient exposure to cold temperatures.
- Pharmacologic interventions
- Diazepam. Diazepam may decrease brown fat uptake (brown fat has benzodiazepine receptors; in addition diazepam may decrease general sympathetic activity).
- However, in one report4 diazepam did not affect brown fat uptake in rats.
- Other drugs. Administration of resperine and propanolol has been shown to decrease brown fat uptake in rats.4
- Drugs to avoid. Drugs that stimulate the sympathetic nervous system (e.g., nicotine and ephedrine) can potentially increase brown fat uptake and should be avoided prior to the study if possible.
- Minimized exposure to cold temperature. Patients should dress warmly and avoid cold temperature for 48 hours before the scan. Also, patients should be kept warm between injection and imaging.5 Temperature control may be helpful even when pharmacologic intervention is unsuccessful.
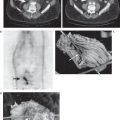
- Urinary activity. FDG activity is seen in renal collecting systems, ureters, and bladder. The role of intervention to reduce urinary artifacts depends on the pathology being evaluated. Collecting system activity can mimic or obscure renal neoplasms. Reducing ureteral activity is helpful for evaluating retroperitoneal nodes. Reduction of bladder activity is important for evaluating pelvic pathology and nodes (see Chapters 22 and 23). However, in many circumstances, additional intervention is usually not necessary, particularly if the cancer being evaluated does not have a propensity for pelvic or retroperitoneal metastases. A protocol can be designed to reduce bladder activity, collecting system/ureteral activity, or both. Nevertheless, in our experience, these interventions are rarely required. Combined PET/ computed tomographic (CT) imaging will also reduce the need for such interventions.
- Reducing bladder activity
- Hydration/diuretics
- Hydration and/or diuretics dilute urine activity and also result in more frequent voiding.
- Diuretic administration has a potential additional advantage over hydration alone: both hydration and diuretics increase urine volume, but hydration can also increase FDG delivery to the bladder (potentially offsetting the value of increased voiding).6
- Foley catheter
- Placement of a Foley catheter for drainage will greatly reduce bladder activity and decrease radiation dose to the bladder.
- However, the bladder may be helpful in certain cases as an anatomic landmark on non-PET/CT studies. If the bladder is filled with saline through the catheter before imaging the pelvis, this will result in a full bladder that can be used as a landmark, but without intense activity that may obscure important findings.
- Catheter placement has the disadvantage of adding an invasive component to a noninvasive study.
- Bladder irrigation
- In conjunction with a Foley catheter, warm saline is used to irrigate the bladder during the time of the scan.
- If bladder irrigation is used, diuretics may not be necessary.7
- Reducing collecting system/ureteral activity. Collecting system and ureteral activity can be reduced by diluting the urine with hydration and/or diuretics.
- Sample protocol to reduce urinary activity:8
- Hydrate after FDG injection.
- Administer furosemide 30 minutes after FDG injection.
- Place Foley catheter before scanning.
- Scan the pelvis as the last bed position.
- Fill the bladder retrograde with normal saline and clamp catheter before scanning the pelvis.
- Bowel activity. Bowel activity is primarily seen in the cecum, right colon, and rectosigmoid and to a lesser extent in the remaining colon and small bowel. Several methods can be used to reduce bowel activity (uptake is mostly in the wall and to a lesser extent the lumen; no one method is completely successful to reduce bowel activity). As with urinary activity, combined PET/CT imaging may reduce the need to minimize bowel activity with interventions.
- Administer isosmotic solution (e.g., Go-LYTELY, Braintree Laboratories, Inc., Braintree, MA) the evening prior to the exam. NPO until the exam.
- Administration of glucagon or oral spasmolytic medications (e.g., mebeverine) to decrease peristalsis is typically less helpful.9
- Postbiopsy. 1 week
- Postsurgery. 6 weeks
- Should be adjusted based upon the invasiveness of the procedure.
- Postradiofrequency ablation. 4 weeks10
- Postchemotherapy. 2 to 4 weeks
- Postradiation. 2 to 6 months
- Both chemotherapy and radiation can cause false-positive results (from inflammation) and false-negative results (from presumed “stunning” of viable tumor). Corticosteroids decrease the inflammatory response after chemotherapy.11
- False-positive/negative results have been reported up to 3 months postchemotherapy12 and 5 months postradiation.13 One study14 suggests that PET can be accurately performed 1 month after radiotherapy of head and neck cancer. The preceding time intervals represent a general range based upon the published literature.
- Baseline studies should be performed before initiation of chemotherapy because FDG uptake can be decreased even 1 day after start of chemotherapy.15
- Postgranulocyte colony-stimulating factor (G-CSF). 1 week to 1 month
- The reported time interval after cessation of G-CSF necessary to avoid increased uptake due to the stimulation is variable, ranging from 5 days to 1 month (see Chapter 6).16,17
- Radiation dose. Most of the radiation dose to the baby is from proximity to the mother rather than FDG excretion into breast milk.18
- Discontinuation. Breastfeeding can be discontinued for 24 hours after FDG injection.
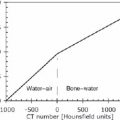
FDG can be administered orally if intravenous access is not available (Fig. 4.2). The same delay before imaging used with intravenous injection can be employed with oral administration.
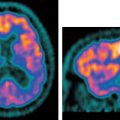
The myocardium metabolizes free fatty acids in the fasting state. To image the myocardium specifically, the nutrient substrate must be switched to glucose. This can be achieved either by oral glucose loading or by hyperinsulinemic-euglycemic clamp. Another approach is to decrease myocardial fatty acid metabolism.19,20
Twenty-five to 100g of oral glucose can be administered prior to FDG injection.
- Advantages. Glucose loading is very practical to perform compared with hyperinsulinemic–euglycemic clamp.
 Oncological PET
Oncological PET Cardiac PET
Cardiac PET
![]()