28
FDG PET in the Evaluation of
Infection and Inflammation
Sandip Basu, Abass Alavi, and Eugene C. Lin
Although several molecular mechanisms have been proposed as the basis for fluorodeoxyglucose (FDG) uptake in cells, overexpression of glucose transport protein 1 (GLUT1) subtype in the stimulated macrophages, neutrophils, and lymphocytes is considered the most likely underlying biological phenomenon responsible for this observation. The data on the role of combined positron emission tomography/computed tomography (PET/CT) in the assessment of infection and inflammation are sparse at this time, but undoubtedly this modality may prove to be even more effective than PET alone for evaluating certain clinical scenarios where surgical interventions are being considered.
- Advantages of FDG PET
- Securing results within a short period of time (1.5 to 2 hours)
- High-resolution tomographic images
- High target-to-background contrast ratio
- Sensitive for chronic infections
- Technically not demanding or less labor-intensive
- High interobserver agreement
- Radiation dose 2 to 3 times lower than that of conventional nuclear medicine techniques
- Useful in detecting infection in the axial skeleton, where white blood cell (WBC) scanning is of limited value
- Disadvantages of FDG PET
- Not widely available in most of the world
- Relatively high cost
- Differentiation between tumor and infection or inflammation is not possible, but delayed imaging and dual-time-point PET is of help.
- Advantages of FDG PET
- Whole-body technique
- Not affected by metallic implants
- Assessment of metabolic activity of inflammatory process is more specific in the right setting than hyperperfusion or edema (CT/MRI).
- Disadvantages of FDG PET
- Not widely available in most of the world
- Relatively low spatial resolution compared with structural techniques
- Limited added value in the diagnosis of uncomplicated cases of acute osteomyelitis compared with the combination of physical examination, biochemical alterations in combination with three-phase bone scanning or MRI
- Several studies have documented the important role of FDG PET in diagnosing patients with chronic osteomyelitis (Figs. 28.1, 28.2, and 28.3).
- In contrast to other nuclear medicine modalities, such as gallium scintigraphy and labeled leukocyte imaging, FDG has high resolution and can distinguish soft tissue infection from osteomyelitis.
- It is expected that FDG PET imaging will be used routinely in the near future to determine the presence or the absence of an infectious focus, to monitor response to antimicrobial treatment, and to develop criteria for deciding when the treatment can be safely stopped.
- Guhlmann et al1,2 reported a higher accuracy for FDG PET than antigranulocyte antibody scintigraphy in imaging the central skeleton for infection in patients with suspected chronic osteomyelitis.
- De Winter et al3 reported a sensitivity of 100%, a specificity of 86%, and an accuracy of 93% in 60 patients with suspected chronic musculoskeletal infections.
- Another prospective study by Meller et al4 on 30 patients with suspected active chronic osteomyelitis concluded that FDG PET is superior to indium 111-labeled leukocyte imaging in the diagnosis of chronic osteomyelitis in the central skeleton.
- FDG PET accurately detects spinal osteomyelitis (Fig. 28.2) and could potentially replace gallium 67 (67Ga) for this purpose.5–7
- A recent meta-analysis showed that FDG PET is not only the most sensitive imaging modality for detecting chronic osteomyelitis, but also has a greater specificity than radio-labeled WBC scintigraphy, bone scintigraphy, or MRI.8–10
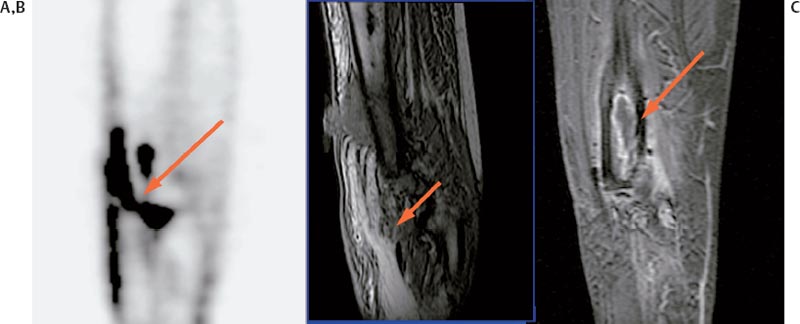
Fig. 28.1 (A) Sagittal fluorodeoxyglucose positron emission tomography (FDG PET). (B) Precontrast spoiled gradient (SPGR). (C) Postcontrast SPGR. Avid FDG uptake in the sinus tract (arrow) connecting soft tissue abscess with the medullary track of the femur in a patient of proven chronic osteomyelitis. Corresponding magnetic resonance imaging abnormalities are also shown in this figure. (From Kumar R, Basu S, Torigian D, Anand V, Zhuang H, Alavi A. Role of modern imaging techniques for diagnosis of infection in the era of 18F-fluorodeoxyglucose positron emission tomography. Clin Microbiol Rev 2008;21(1):209–224. Reprinted with permission.)
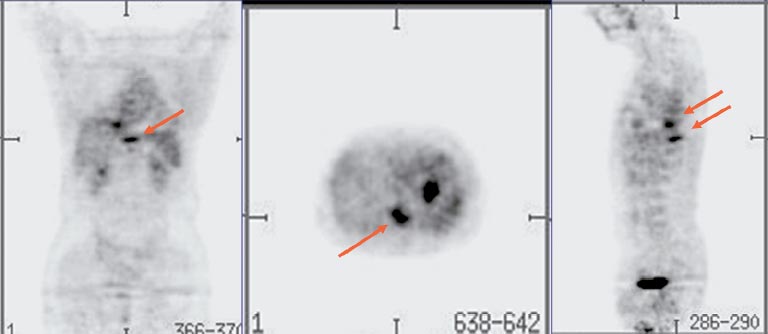
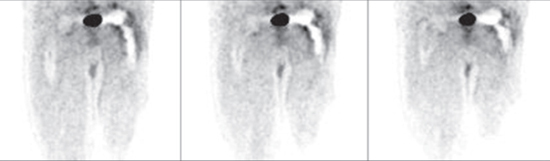
Fig. 28.2 Foci of fluorodeoxyglucose uptake in chronic osteomyelitis of the thoracic spine in two adjacent vertebral bodies. Radiolabeled white blood cell imaging in general has a low yield in this setting. (From Zhuang H, Alavi A. 18-fluorodeoxyglucose positron emission tomographic imaging in the detection and monitoring of infection and inflammation. Semin Nucl Med 2002;32:47–59. Reprinted with permission.)
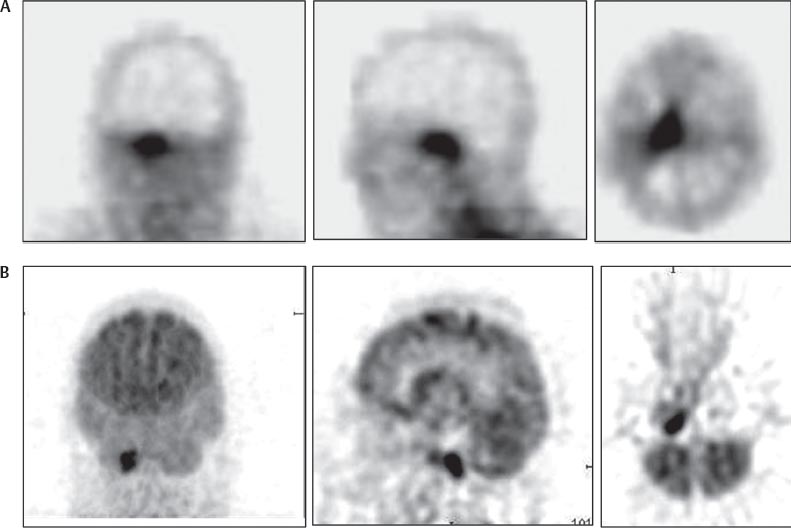
Fig. 28.3 (A) Gallium single-photon emission tomography (SPECT). (B) Fluorodeoxyglucose positron emission tomography (FDG PET). Avid FDG uptake in the focus of infection in a patient of proven malignant otitis with corresponding gallium 67 citrate-SPECT images. Note that PET images reveal the site of the disease more precisely than those of SPECT. (From Zhuang H, Alavi A. 18-fluorodeoxyglucose positron emission tomographic imaging in the detection and monitoring of infection and inflammation. Semin Nucl Med 2002;32:47–59. Reprinted with permission.)
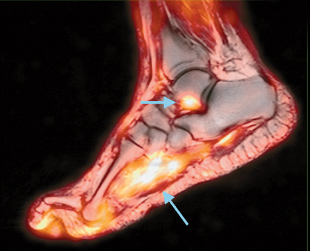
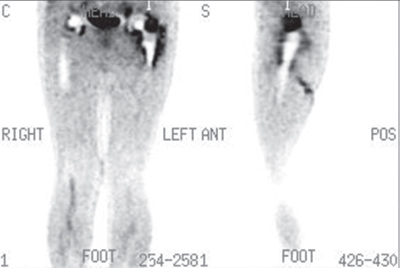
Fig. 28.4 Fused fluorodeoxyglucose positron emission tomography (FDG PET) and magnetic resonance (MR) images of a patient with a diabetic foot and a suspected bone infection. FDG PET image shows significant uptake in the soft tissue in the plantar aspect of the foot (suggestive of cellulitis); in addition, it reveals a focus of abnormal activity in the talus (consistent with talar bone osteomyelitis). (From Basu S, Alavi A. FDG-PET takes lead role in suspected or proven infection. Diagnostic Imaging San Francisco 2007; 29(11):59–64. Reproduced with permission.)
Detection of infection and differentiating it from acute neuropathic osteoarthropathy in the setting of a complicated diabetic foot is a clinical and radiological challenge. The presence of ulceration also complicates the scenario because in this setting infection is strongly considered until proven otherwise. Distinguishing osteomyelitis from Charcot osteoarthropathy by MRI is a difficult task.
- Preliminary data provide evidence for an important role for FDG PET imaging in the setting of complicated and uncomplicated diabetic osteoarthropathy.10,11
- It can differentiate between Charcot neuroarthropathy and osteomyelitis and also soft tissue infection.12,13
- FDG PET/CT was found to be highly accurate in detection of osteomyelitis (Fig. 28.4) by Keidar et al.11
- One particular challenge for orthopedic surgeons has been differentiating mechanical loosening of prosthesis from superimposed infection and has been the subject of multiple research studies during the past several years.
- FDG PET has a great potential for detecting infection in hip prostheses (Figs. 28.5, 28.6, and 28.7), and to a lesser extent in knee prostheses.
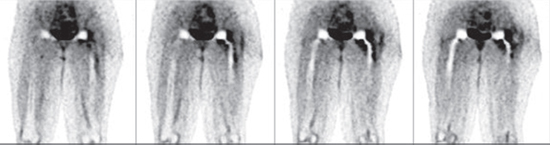
Fig. 28.5 The coronal images shown above belong to a patient with a painful left hip following arthroplasty. Although there is some inflammation seen around the neck of the prosthesis and the proximal femur, this is a common reaction in patients after insertion of hip prostheses. The images show no clear evidence of infection due to lack of fluorodeoxyglucose uptake at the bone–prosthesis interface; this aseptic diagnosis was confirmed by surgical intervention in this patient.
Fig. 28.6 Coronal images of the pelvis and thigh regions show no evidence of infection in the right hip prosthesis. On the left side, however, there is significant uptake of fluorodeoxyglucose at the bone–prosthesis interface surrounding the acetabular component and in the proximal half of the femoral stem. There is also evidence of extension of infection into the proximal soft tissue structures. The right prosthesis appears aseptic, and the left prosthesis appears infected. This was confirmed by surgical exploration.
- FDG PET is advantageous over anatomical imaging modalities because it is not affected by the metal implants and provides better resolution images than those of the conventional nuclear medicine techniques, and it is exquisitely sensitive.
- Noninfectious reactions are common months and even years after surgery, and the recognition of such reactions is important in managing these patients. Increased FDG uptake around the neck and/or head of the prosthesis is very common and should not be interpreted as a finding suggestive of infection. Most infection is found at the bone–prosthesis interface, and most noninfectious inflammatory reactions are found outside the bone–prosthesis junction.
- Presently, the potential of FDG PET in the evaluation of prostheses is relatively well defined. More research may further enhance the role of FDG PET in the evaluation of prostheses.
- In a prospective study involving 89 patients with 92 painful hip prostheses, our group14 reported that the respective sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of FDG PET for detecting infection was 95.2, 93, 80, and 98.5%, respectively. Similar figures of technetium 99m sulfur colloid indium 111–labeled white blood cell scintigraphy (TcSC-Ind BM/WBC) in the diagnosis of periprosthetic infection for hip prostheses was 50, 95.1, 41, and 88.6%, respectively.
 Comparison of FDG PET with Other Imaging Modalities for Evaluating Infection and Inflammation
Comparison of FDG PET with Other Imaging Modalities for Evaluating Infection and Inflammation Potential Clinical Applications
Potential Clinical Applications