- •
Metabolic diseases are independently associated with increased CVD risk.
- •
SPECT MPI is limited by soft-tissue attenuation in obese individuals; however, imaging techniques including prone and gated imaging, cardiocentric cameras, and attenuation correction improve diagnostic accuracy.
- •
Individuals with the MetS or DM have a worse prognosis with increasing metabolic impairment for a given degree of abnormality on SPECT imaging, and women with DM have the greatest risk for any degree of abnormality.
- •
For asymptomatic patients with DM who are on medical therapy for CAD, there is no clear role for radionuclide MPI to screen for CAD, unless there are other markers of disease (e.g., CAC score >400, abnormal rest ECG with pathologic Q waves) or comorbidities that increase the likelihood of CAD (e.g., peripheral arterial disease).
- •
PET MPI provides improved diagnostic accuracy compared with SPECT MPI in obese patients as a consequence of attenuation correction, higher energy tracers, and MBF measurements.
- •
PET MPI provides an assessment of both epicardial and microvascular CAD in patients with metabolic disease.
- •
MFR measurements on PET myocardial perfusion imaging predict adverse CVD events independently from baseline BMI and metabolic status.
- •
MFR is increasingly abnormal with an increasing degree of metabolic impairment.
Introduction
Cardiometabolic disease, a combination of metabolic and cardiovascular abnormalities that includes insulin resistance, impaired glucose tolerance, dyslipidemia, hypertension, and central adiposity, is increasing in incidence and prevalence across the world and extends to all ages, including children and adolescents. Recent data from the National Health and Nutrition Examination Survey (NHANES) indicated that the prevalence of obesity was 39.8% among adults and 18.5% among youth (2 to 19 years) in the United States between 2015 to 2016. It is estimated that the prevalence of obesity in the United States will reach approximately 50% by year 2035, which will be associated with a concomitant increase in the rates of prediabetes and diabetes mellitus (DM). These metabolic abnormalities are associated with higher rates of coronary artery disease (CAD) and heart failure with preserved ejection fraction (HFpEF), atrial fibrillation, and other cardiovascular diseases (CVDs).
Several pathologic effects of these metabolic abnormalities contribute to the development of CVD in this population. In addition to accelerating the development of atherosclerotic plaques with greater inflammation and larger necrotic cores, increased serum glucose, adipose tissue volume, and lipid concentrations lead to increased inflammation and oxidative stress that result in microvascular rarefaction and vasomotor dysfunction. , As such, individuals with metabolic diseases are at increased risk for both epicardial and microvascular CAD and have a propensity to develop diffuse atherosclerosis throughout the coronary tree. These same changes may also contribute to the development of HFpEF in this population. Radionuclide myocardial perfusion imaging (MPI), especially when performed with positron emission tomography (PET), provides a useful method for noninvasively evaluating for the presence of either form of CAD in this at-risk population. In this chapter, we will review the strengths and weaknesses of radionuclide MPI in this population and highlight the relative merits of single photon emission computed tomography (SPECT) and PET imaging and other imaging modalities.
Technical considerations
There are a number of important factors that one must consider when defining the imaging approach for patients with metabolic diseases who have suspected or known CAD. Some of these factors relate to strictly practical technical issues, whereas others relate to the biology of CAD in this population, which also has technical implications. The following list is a summary of factors that one must consider before defining the imaging approach. These factors will be illustrated and discussed in the case vignettes and are covered in greater detail in previous chapters as noted.
- •
Protocol selection : As discussed in greater detail in Chapters 4 and 5 , there are a range of important technical considerations regarding selection of MPI protocol, including decisions for 1-day versus 2-day studies, radiopharmaceutical selection, stress-first or rest-first, exercise versus. pharmacologic stress, and appropriate radiopharmaceutical dose. There are also clinical considerations that might influence the list above, including the patient’s age, comorbidities (e.g., pulmonary disease), and underlying clinical risk (e.g., acute vs. chronic coronary syndromes).
- •
Importance of attenuation correction : This is an important consideration in protocol selection with direct implications on image quality and diagnostic certainty, as discussed in Chapter 5 .
- •
Implications on radiation dosimetry : Protocol selection has direct implications on radiation dosimetry, which should be carefully weighted and tailored to patient demographics (age and sex) and medical history. This is discussed in greater detail in Chapter 6 .
- •
Opportunities for new technology : Technical advances in nuclear cardiology (e.g., introduction of solid-state detector SPECT and digital PET scanners) offer new opportunities with direct implications on image quality and diagnostic certainty. Please see also discussions in Chapters 1 and 2 .
- •
Relevance of diffuse atherosclerosis and microvascular dysfunction : As already briefly mentioned, there is growing evidence that diffuse atherosclerosis and microvascular dysfunction is a much greater problem in patients with cardiometabolic disease, which has important implications for considering the added value of quantification of atherosclerotic burden and ischemia, including coronary vascular function, as discussed in Chapter 3 .
Patient-centered clinical applications
Case vignette 1: Obese patient with severe attenuation on SPECT but normal PET
A 48-year-old woman with history of morbid obesity, asthma, obstructive sleep apnea on nocturnal continuous positive airway pressure ventilation, DM, HFpEF, and polymyositis presented with recurrent volume overload. She ruled-out for acute coronary syndrome and underwent diuresis. Once her volume status was improved, she underwent pharmacologic SPECT MPI with 99m Tc-Tetrofosmin, which showed findings consistent with a prior anterior myocardial infarction (MI) with mild periinfarct ischemia and a left ventricular ejection fraction (LVEF) of 73% (see Fig. 14.1 ). Given concern for attenuation artifact and a false-positive rather than a truly positive scan, she was then referred for pharmacologic 82 rubidium PET MPI. The PET scan revealed no evidence of myocardial scarring or ischemia. LVEF was 71% and the coronary artery calcium (CAC) score was zero ( Fig. 14.2 ). She was discharged on medical therapy.


Obesity affects more than half a billion adults and is independently associated with CVD, although not all patients with obesity carry the same cardiometabolic risk. Nevertheless, increased body mass index (BMI) is independently associated with CAD as well as the risk for MI. The pathophysiologic underpinnings underlying the development of CVD in obesity are complex and are thought to involve a combination of increased production of adipocyte-related factors that lead to vascular oxidative stress, neurohormonal activity, and systemic inflammation. Importantly, the presence of visceral adiposity and obesity have been associated with progression of atherosclerotic disease, even among individuals on statin therapy. As such, many obese patients undergo nuclear MPI for the diagnosis of CAD. Nevertheless, as demonstrated in Case Vignette 1, testing in this population presents unique challenges for both patients and healthcare providers.
SPECT remains the most widely used radionuclide MPI technique for patients with suspected or known CAD, including obese individuals. Importantly, overweight patients with a normal SPECT study have been found to have a low risk (<1%/year) of cardiac death. Nevertheless, overweight patients with known CAD and an abnormal SPECT imaging have a better prognosis than individuals with normal weight and an abnormal study, likely a consequence of a higher rate of false-positive tests among overweight patients due to attenuation artifacts.
Obese individuals are more likely to have a nondiagnostic test and are less likely to perform exercise. Furthermore, weight-based vasodilator dosing only applies to patients up to 250 lbs. (excluding regadenoson) and, as discussed in Chapters 4 and 5 , patients with obesity often require higher radiopharmaceutical doses for optimal image quality. Consequently, it is possible that maximal vasodilatation may not be achieved in morbidly obese patients with implications on diagnostic sensitivity at the expense of higher radiation exposure. Finally, some SPECT cameras are not able to safely image patients heavier than 300 lbs.
Increased false-positive and nondiagnostic results due to of soft-tissue attenuation and a lack of exercise data can lead to unnecessary downstream testing and increased patient burden. Several strategies have been developed to mitigate the challenges for radionuclide MPI in obese patients. First, implementation of 2-day imaging protocols allows for the injection of higher radiopharmaceutical doses for both stress and rest imaging, thereby improving image quality in the setting of increased soft-tissue attenuation. Although it is reasonable to consider stress-first imaging in obese patients to reduce radiation dose and patient convenience, one has to keep in mind that the frequency of follow-up rest imaging is generally higher, especially in morbidly obese patients. When rest imaging is necessary, it is probably best to perform this on a different day if possible so as to minimize injected dose and radiation exposure. The need for additional rest imaging can be decreased if new technology is available (e.g., solid-state SPECT camera and attenuation correction), as illustrated by Case Vignette 2. Second, although exercise stress is typically preferred over pharmacologic stress for the purposes of optimizing diagnostic information and image quality, patients with a body weight over 250 lbs. Who are unable to exercise and require vasodilator stress typically should be considered for regadenoson stress because of its improved effectiveness in obese patients at a fixed dose. Third, one additional strategy is to apply noise reduction and resolution recovery techniques during the SPECT reconstruction to improve image quality and reduce false-positive results (please refer to the detailed discussion in Chapter 1 ). Those who are too heavy for traditional SPECT cameras can often be imaged with planar imaging, but this is a more limited approach than tomographic SPECT imaging and should be reserved as a last resource. Finally, electrocardiogram (ECG)-gated and prone images can be useful to troubleshoot attenuation artifacts, as discussed in Chapter 5 .
Case vignette 2: Obese patient with normal solid-state detector SPECT MPI
A 61-year-old woman with a history of obesity (BMI 36.6 kg/m 2 ), tobacco smoking, and known CAD with prior stenting of her left anterior descending (LAD) artery 4 years before presented for outpatient follow-up and reported occasional fleeting chest discomfort that occurred largely at rest. She underwent adenosine SPECT MPI with a traditional Anger camera with findings of a medium-sized stress-induced defect in the territory of the mid LAD in the setting of differential attenuation ( Fig. 14.3 A). To clarify the findings further, her cardiologist referred her for repeat pharmacologic testing using a cadmium-zinc-telluride (CZT) cardiocentric camera. This study implemented both supine and upright stress imaging and demonstrated normal perfusion (see Fig. 14.3 B). In light of these results, she continued on her current cardiovascular regimen without further testing.


More recently, CZT cardiocentric cameras and attenuation correction using computed tomography (CT) or a line source have provided additional improvements for SPECT imaging. , As discussed in Chapter 1 , this new technology offers significantly higher photon sensitivity than conventional SPECT cameras, thereby allowing improved image quality at reasonably low radiopharmaceutical doses and improved diagnostic accuracy.
Role of PET MPI in obesity
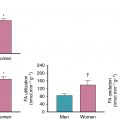
In comparison to SPECT imaging, PET MPI offers improved diagnostic accuracy and risk stratification in obese patients, including those with extreme obesity, as a consequence of the routine use of attenuation correction, the use of higher energy tracers that are less subject to attenuation, and the ability to quantify absolute myocardial blood flow (MBF). , Furthermore, because of the shorter physical half-life of PET radiopharmaceuticals, the test can be completed on the same day at a significantly lower radiation dose than SPECT MPI. Thus the evaluation of CAD in obese individuals who have or are likely to have nondiagnostic or equivocal SPECT studies is an important indication for PET MPI and should be used as the preferred test if available. Furthermore, the results provide a useful assessment of cardiovascular risk with low cardiovascular mortality associated with a normal study and incrementally increased risk in abnormal studies across a range of BMIs ( Figs. 14.4 and 14.5 ). ,

Myocardial flow reserve (MFR), a combined assessment of both large- and small-vessel ischemia, from PET MPI provides incremental discrimination of cardiovascular risk across the spectrum of BMI. , Total coronary vasodilator capacity is significantly lower in obese individuals, and BMI independently associates with abnormal MBF measurements. Among obese individuals, MBF measurements are reduced in parallel with increased biomarkers of inflammation and insulin resistance. Reduced stress MBF and MFR may also be affected by the epicardial adipose tissue volume. Moreover, decreased MFR has been shown to predict adverse cardiovascular events independently of BMI across the spectrum of obesity among those with and without clinical CAD, whereas those with obesity but preserved MFR are paradoxically at a lower risk for adverse events (see Fig. 14.5 ). ,

Alternative imaging approaches in obese patients
Although radionuclide imaging is frequently used for diagnosis and management of CAD in obese patients, other modalities may also provide useful information for this population. Vasodilator stress magnetic resonance imaging (MRI) is a safe, feasible, and effective means of obtaining prognostic information in obese patients, although it may be more challenging to perform in morbidly obese patients. Similar to other populations, a low CAC score on CT imaging confers reduced cardiovascular risk. The effectiveness of stress echocardiography is more limited because of acoustic attenuation in obese and morbidly obese patients.
Case vignette 3: Patient with CAD and coronary microvascular dysfunction
A 71-year-old woman with a history of DM on insulin, extensive tobacco use, chronic obstructive pulmonary disease, and prior cerebrovascular accident presented to the emergency department with sudden onset crushing substernal chest pain. Her pain improved with nitroglycerin and she ruled-out for MI. During admission, she underwent dobutamine SPECT MPI with negative ECGs and imaging that demonstrated a small area of scarring without ischemia in the territory of the posterior descending artery with an LVEF of 60% ( Fig. 14.6 A). She was discharged on medical therapy. Over the next several months, she continued to experience progressive exertional dyspnea and associated chest heaviness. A PET MPI was performed with regadenoson and demonstrated a medium-sized area of myocardial scarring without ischemia in the distribution of the posterior descending artery with an LVEF of 58%. Her transmission CT scan showed extensive coronary calcification (see Fig. 14.6 B). The quantitative flow data showed severely reduced stress MBF and MFR in all territories, with a mild base to apical flow gradient, and also globally ( Table 14.1 ). Follow-up coronary angiography showed diffuse calcified nonobstructive CAD ( Fig. 14.7 ). Her medical regimen was further augmented, and she was discharged without further intervention.