Hepatocellular carcinoma (HCC)
Patterns of tumour spread
INITIAL COMMON PATTERNS OF TUMOUR SPREAD
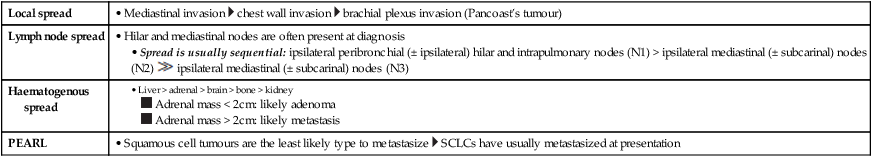
Local spread
• Mediastinal invasion  chest wall invasion
chest wall invasion  brachial plexus invasion (Pancoast’s tumour)
brachial plexus invasion (Pancoast’s tumour)
Lymph node spread
• Hilar and mediastinal nodes are often present at diagnosis
• Spread is usually sequential: ipsilateral peribronchial (± ipsilateral) hilar and intrapulmonary nodes (N1) > ipsilateral mediastinal (± subcarinal) nodes (N2)  ipsilateral mediastinal (± subcarinal) nodes (N3)
ipsilateral mediastinal (± subcarinal) nodes (N3)
Haematogenous spread
PEARL
• Squamous cell tumours are the least likely type to metastasize  SCLCs have usually metastasized at presentation
SCLCs have usually metastasized at presentation
Local spread
• Local spread into adjacent structures (e.g. pancreas, colon, spleen)
Lymph node spread
• Perigastric: pericardial  lesser curvature
lesser curvature  greater curvature
greater curvature  suprapyloric
suprapyloric
• Extraperigastric: left gastric  common hepatic
common hepatic  coeliac
coeliac  splenic hilum and artery
splenic hilum and artery  hepatic pedicle
hepatic pedicle  retropancreatic
retropancreatic  mesenteric root
mesenteric root  middle colic
middle colic  para-aortic
para-aortic
• NB: retropancreatic, para-aortic and mesenteric nodes are classified as M1 metastatic disease
Haematogenous spread
• Via the portal vein to the liver (25% at presentation)  a similar number will have peritoneal metastases
a similar number will have peritoneal metastases
PEARL
• Transcoelomic spread can occur through the peritoneum (e.g. Kruckenberg tumours)
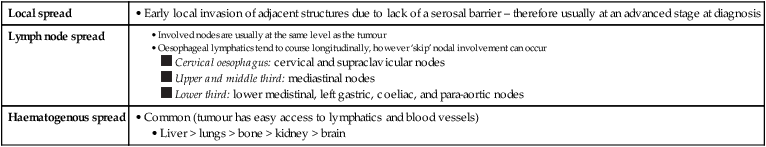
Local spread
• Early local invasion of adjacent structures due to lack of a serosal barrier – therefore usually at an advanced stage at diagnosis
Lymph node spread
Haematogenous spread
• Common (tumour has easy access to lymphatics and blood vessels)
• Liver > lungs > bone > kidney > brain
Local spread
• Invasion through the bowel wall into the perirectal fat – an important predictor of local recurrence and survival
• Extramural venous invasion is an adverse prognostic factor
Lymph node spread
• From the level of the tumour cranially within the mesorectum – proximal blockage (e.g. extensive adenopathy) may cause retrograde spread with lower rectal tumours rarely spreading to the inguinal nodes
• Pelvic side wall spread is unusual
Haematogenous spread
• Liver (via the portal vein)
PEARLS
• Involvement of the circumferential resection margin (CRM) is an adverse prognostic feature (including disruption during surgery)
• Perforation of the peritoneal membrane can result in transcoelomic spread as well as an increased risk of recurrence
• Transcoelomic spread favours the lower right small bowel mesentery and the pouch of Douglas
Local spread
• Vascular invasion of the portal or hepatic veins
Lymph node spread
• Spread to lymph nodes along the hepatoduodenal ligament
Haematogenous spread
• Lung = bone > adrenals > peritoneum
PEARL
• Abdominal lymph nodes are often enlarged with cirrhosis
Local spread
• 70% of tumours arise within the pancreatic head
• Tumour spreads by direct perivascular and perineural invasion
• Head/uncinate process tumours: these usually extend along the SMA and mesenteric root
• Body/tail tumours: these usually infiltrate the coeliac, hepatic or splenic arteries
• Local invasion can involve the stomach, duodenum and retroperitoneum
Lymph node spread
• Early micrometastases at presentation are common
• Primary drainage: superior, inferior, anterior, posterior and splenic lymph nodes
• Secondary drainage: porta hepatis, common hepatic, coeliac, mesenteric root lymph nodes
• Tertiary drainage: peri-aortic and distal superior mesenteric lymph nodes
Haematogenous spread
• Early micrometastases at presentation are common
• These usually involve the liver and peritoneal surfaces
PEARL
• Usually only tumours of the head and uncinate process are surgically resectable (tumours of the body and tail usually have perivascular or perineural metastases at presentation)
Local spread
• Vascular invasion of the portal or hepatic veins
Lymph node spread
• Spread to lymph nodes along the hepatoduodenal ligament – with a propensity to spread to the portocaval lymph node chain as well as the anterior and posterior pancreaticoduodenal chain
Haematogenous spread
• Less common than with HCC – remote metastases are usually to the lung (less commonly to bone, the adrenals and peritoneum)
Local spread
• Perinephric fat  ipsilateral adrenal
ipsilateral adrenal  adjacent viscera (including muscles)
adjacent viscera (including muscles)
• Renal vein invasion (± IVC)
Lymph node spread
• Via lymphatics following the renal vessels to the ipsilateral para-aortic nodes  direct connections with the thoracic duct and mediastinum also exist
direct connections with the thoracic duct and mediastinum also exist
Haematogenous spread
• Common sites: lungs > bones, CNS, adrenals
PEARL
• IVC tumour thrombus extending above the hepatic veins requires a transthoracic surgical approach – right atrial involvement requires cardiopulmonary bypass
Local spread
• Initially perivesical fat infiltration  subsequent invasion of adjacent pelvic organs and the pelvic side wall by direct invasion
subsequent invasion of adjacent pelvic organs and the pelvic side wall by direct invasion
Lymph node spread
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access











