Pediatric Abdominal Emergencies
Keith P. Cross
Matthew A. Monson
David J. McLario
INTRODUCTION
Abdominal complaints are encountered frequently in emergency pediatrics and often prompt lengthy and expensive evaluations. The ability to rapidly narrow a diverse list of potential conditions is important for the timely treatment of affected children as well as the efficient use of emergency department (ED) resources. Bedside ultrasound may provide a shortcut through the maze of possible diagnoses (1). Although conditions affecting children overlap somewhat with those experienced by adults, several important abdominal emergencies are unique to or more prevalent in children.
CLINICAL APPLICATIONS
Ultrasound is useful in the evaluation of children with a variety of abdominal complaints, including pain, distention, vomiting, hematochezia, or a palpable mass, and it can facilitate the workup of possible appendicitis, intussusception, pyloric stenosis, and volvulus.
IMAGE ACQUISITION
The smaller size of children contributes to the extraordinary utility of ultrasound. Compared to adults, children have less subcutaneous and peritoneal fat, facilitating the sonographic assessment of abdominal organs. In most children, a high-frequency (5 to 15 MHz) linear probe can be used and provides high-resolution images. In cooperative and verbal children capable of communicating the precise location of maximal abdominal pain or tenderness, relevant ultrasound images may be acquired rapidly at the bedside, expediting diagnosis and treatment.
Patient positioning is strategic for the rapid acquisition of images. If sonographic evaluation is not accomplished in a timely manner, many children will be unable to cooperate. Relaxation of the abdominal musculature allows the sonographer to compress intra-abdominal organs with minimal applied pressure. This can be facilitated by placing a roll under the knees of the supine patient, serving to shorten and relax the rectus abdominus muscles. Similarly, positioning a caregiver opposite the sonographer to hold the child’s hands
at waist level may also minimize patient stretching and tightening of the abdominal musculature.
at waist level may also minimize patient stretching and tightening of the abdominal musculature.
In infants with suspected pyloric stenosis, the administration of an oral fluid such as glucose water facilitates distention of the stomach and improves the ability to distinguish tissue layers of different echogenicity. When administering oral fluids, tilting the supine infant slightly to his or her right side fills the distal stomach and facilitates fluid passage through the pyloric channel.
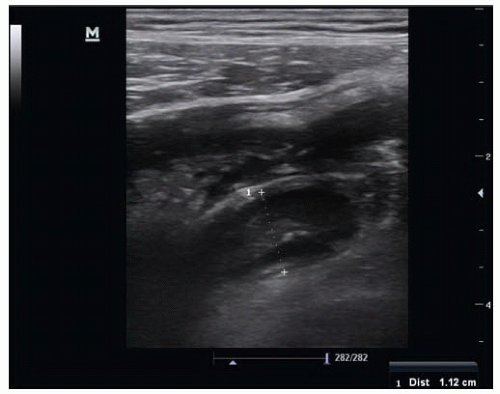
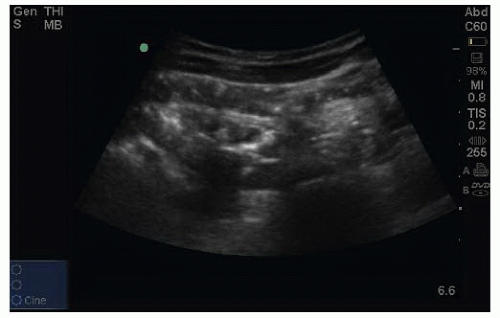
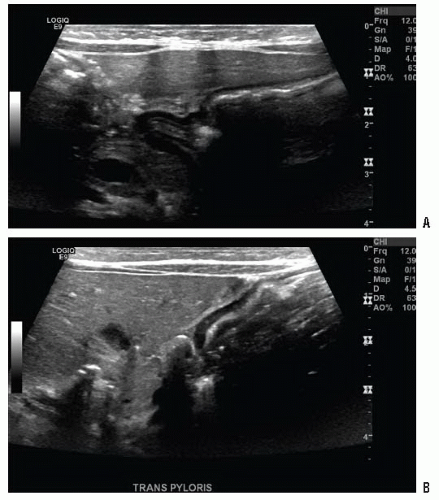
Ultrasound assessments should utilize both transverse and longitudinal planes to optimize accuracy. For example, the appendix can be differentiated from surrounding bowel as a blind-ended loop. This feature is noted when sonographic assessment occurs along its long axis (Fig. 27.1). The diagnosis of pyloric stenosis normally involves measurement of pyloric muscle width as well as channel length in short and long-axes views, respectively (Fig. 27.2).
Moderate doses of analgesic medication are often useful in abdominal conditions where patient feedback and/or compression of suspicious structures facilitate diagnostic efforts. Children may not be capable of cooperating without analgesia.
NORMAL ULTRASOUND ANATOMY
Appendix
The appendix is a blind-ending structure that arises from the inferior cecum, approximately 2 cm caudad to the terminal ileum. It projects in various positions relative to the cecum and the pelvis. The appendix is tubular in shape, measuring 6 mm or less in diameter, and should be freely compressible. Due to its relatively small size, variable orientation, and obscuration by adjacent gas-filled bowel loops, the normal appendix is frequently difficult to visualize using ultrasound.
Small Bowel
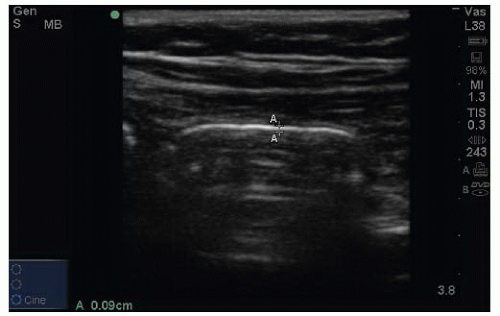
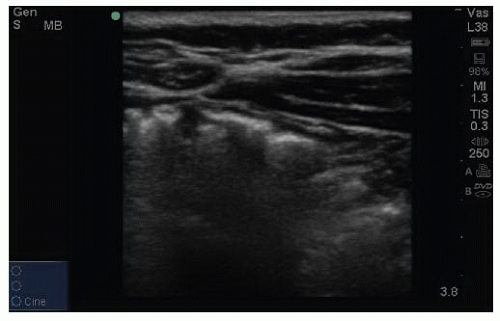
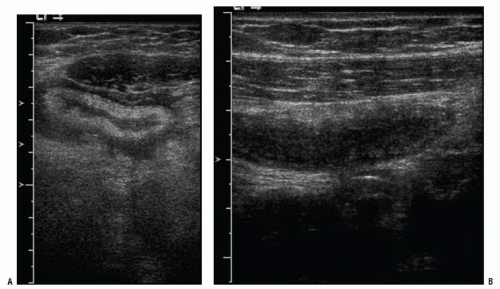
Normal bowel is characterized by active peristalsis and compressibility (Fig. 27.3). Small bowel is considerably larger in diameter than the normal appendix and is oval in transverse axis. Long-axis views often reveal considerable air with associated reverberation artifact (Fig. 27.4). Probe compression may be used to determine compressibility as well as displace intra-intestinal air to facilitate assessment of nearby structures of interest. It is critical, however, when conditions associated with intestinal perforation are suspected, that over zealous compression be avoided. The sonographic appearance of normal bowel wall reflects concentric, alternately echogenic and hypoechoic layers reflecting interfaces of mucosa, muscularis, and serosa. The average thickness of the normal bowel wall is 1 to 2 mm (Fig. 27.5) (2). A loop of small
bowel may occasionally be mistaken for a dilated appendix, but compressibility, the presence of peristalsis, and lack of a blind end are characteristics helpful to avoid this mistake.
bowel may occasionally be mistaken for a dilated appendix, but compressibility, the presence of peristalsis, and lack of a blind end are characteristics helpful to avoid this mistake.
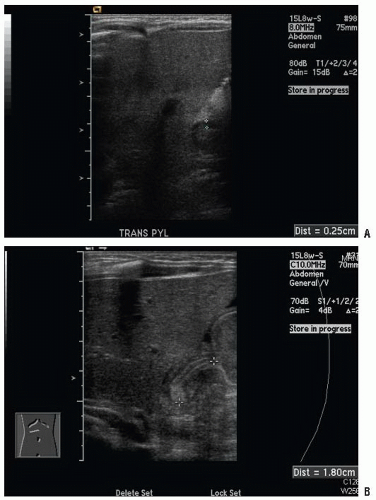 FIGURE 27.2. Pyloric Stenosis. A: Short-axis view. B: Long-axis view. (Images courtesy of Dr. Russ Horowitz, MD.) |
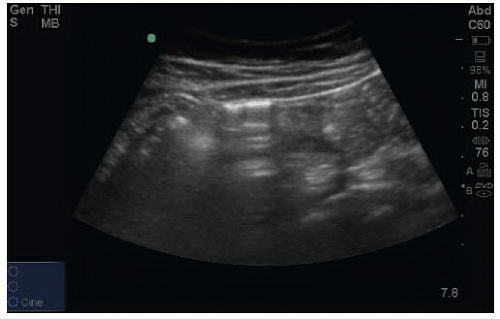 FIGURE 27.4. Long-Axis View of Normal Bowel. Demonstrates characteristic horizontal lines emanating from the near wall. |
Cecum
The cecum constitutes the first part of the large intestine. It is best identified as a large gas- and/or stool-filled pouch-like structure in the longitudinal plane when imaging the right lower quadrant. It may be distinguished sonographically from adjacent bowel by a characteristic “bumpy air” appearance (Fig. 27.6).
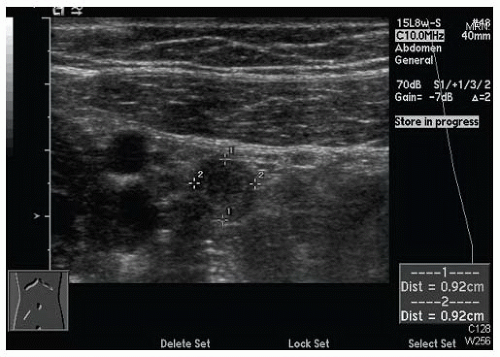
Pylorus
The pyloric sphincter is a circular muscle located at the distal stomach that provides a degree of restriction to stomach outflow, effecting the maceration and fragmentation of ingested food as it resists peristaltic contractions of the stomach. Its physical dimensions include normal wall thickness of <3 mm and length of <15 mm (Fig. 27.7) (3).
PATHOLOGY: APPENDICITIS
Appendicitis is the most common surgical emergency in children and occurs as a result of obstruction of the appendiceal lumen. Causes of obstruction include inspissated fecal material (an appendicolith), hypertrophied lymph tissue, and foreign bodies. As intraluminal accumulation of fluid and mucus continues, appendiceal dilatation and rounding ensues. Patients often provide a history of initial nonlocalized periumbilical aching characteristic of hollow viscous distention. Increasing intraluminal distention eventually results in increased intramural pressure within the walls of the appendix. The resulting impairment in venous drainage initiates a cycle that further increases intramural pressure and eventually compromises arterial flow. When arterial flow to the appendix is compromised, ischemia occurs and results in inflammation that produces the localized peritoneal irritation responsible for the characteristic migration of pain to the right lower quadrant.
Ultrasound Findings in Appendicitis
Ultrasound findings of appendicitis, are noted in Table 27.1, and include static and dynamic findings as well as direct and indirect signs. The presence of hyperechoic soft tissue in the vicinity of the suspected appendix predicts an
inflammatory process and is considered a highly sensitive indicator for appendicitis in the appropriate clinical context (Fig. 27.8; eFig. 27.1). Unfortunately, hyperechoic soft tissue is a nonspecific finding that may be seen in mesenteric adenitis as well as various infectious gastroenteritides.
inflammatory process and is considered a highly sensitive indicator for appendicitis in the appropriate clinical context (Fig. 27.8; eFig. 27.1). Unfortunately, hyperechoic soft tissue is a nonspecific finding that may be seen in mesenteric adenitis as well as various infectious gastroenteritides.
TABLE 27.1 Appendicitis | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
The classic static sonographic features of appendicitis include a round shape noted on transverse axis, a fluid-filled appearance, a diameter >6mm (Fig. 27.9; eFig. 27.2), and the presence of an appendicolith. Although a transverse view of the distended appendix provides the classic view of appendicitis, any abnormality should be viewed in two dimensions to confirm that the suspected appendix is a blindloop structure and not an adjacent loop of bowel (Fig. 27.10). The presence of an appendicolith, accentuated by posterior shadowing, is a very specific finding for appendicitis, although not required for diagnosis (Fig. 27.11). Other findings include peri-appendiceal hyperemia (Fig. 27.12) and pelvic fluid (Fig. 27.13). “Dynamic” findings of appendicitis include absence of peristalsis and lack of compressibility. Care should be taken to distinguish movement of bowel around the appendix from movement within the appendiceal lumen. Time is well spent gaining the trust and cooperation of the child to help determine the site of maximal tenderness relative to suspicious ultrasound findings. In our experience, short-acting analgesia may be necessary to optimize the graded compression technique.
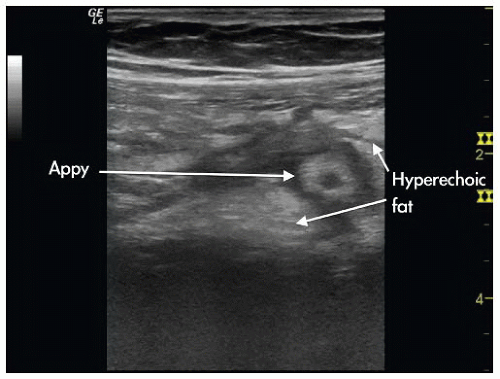 FIGURE 27.8. Ultrasound Image of Appendicitis. Demonstrates hyperechoic soft tissue in the vicinity of the diseased appendix. |
Use of the Image in Clinical Decision Making
Although the specificity of ultrasonography performed by experienced users for the evaluation of possible pediatric appendicitis is comparable to that of computed tomography (CT), sensitivity is compromised when detection of a normal appendix is difficult (4). Appendiceal visualization rates have varied widely in the literature, with one study reporting a rate of only 22%, while others have reported higher rates, particularly when adjunct maneuvers are used (5, 6, 7, 8). However, the presence or absence of certain indirect, or so-called “secondary,” signs of appendicitis may be helpful. The finding of hyperemia in and around a suspicious loop of bowel suggests an inflammatory process (9). Conversely, the absence of hyperechoic soft tissue in the vicinity of abdominal tenderness contends against appendicitis when the appendix cannot be seen.
A possible strategy for the diagnosis of pediatric appendicitis may involve initial sonographic evaluation of children at low risk for perforation and alternative diagnoses. CT may then be reserved for those at increased risk for perforation or those whose ultrasound is indeterminate. For example, the absence of signs of soft-tissue inflammation in an area of focal abdominal tenderness may, in concert with other indicators of low likelihood of appendicitis, allow clinicians to confidently utilize a period of observation as opposed to immediate CT.
Pitfalls
Failing to visualize the common iliac blood vessels, important landmarks for the appendix (Fig. 27.14).
Discarding the diagnosis of appendicitis due to inability to visualize a retrocecal appendix.
Mistaking artifact from a normal loop of bowel for periappendiceal inflammation (Fig. 27.15).
Inadequate period of observation to declare loop aperistaltic.
Finally, it behooves the clinician-sonographer to be willing to accept at least occasional indeterminate readings to avoid false-positive sonographic evaluations.
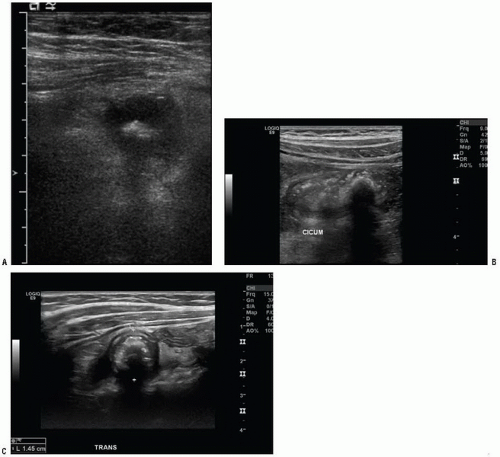 FIGURE 27.11. Appendicitis. Three cases (A, B, and C) where an appendicolith was visualized within an inflammed appendix. |
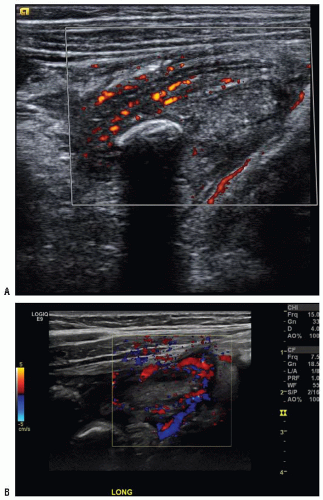 FIGURE 27.12. Peri-Appendiceal Hyperemia. (Images courtesy of Dr. Russ Horowitz, MD.)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|